Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(2); 2023 > Article
-
Scoping Review
Pre-pregnancy Diet to Maternal and Child Health Outcome: A Scoping Review of Current Evidence -
Fadila Wirawan1
 , Desak Gede Arie Yudhantari2
, Desak Gede Arie Yudhantari2 , Aghnaa Gayatri3
, Aghnaa Gayatri3
-
Journal of Preventive Medicine and Public Health 2023;56(2):111-127.
DOI: https://doi.org/10.3961/jpmph.22.472
Published online: March 13, 2023
- 3,558 Views
- 198 Download
- 2 Scopus
1Department of Public Health Nutrition, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
2Child Health Division, Leuwiliang General District Hospital, Bogor District, Indonesia
3Department of Family and Community Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
- Corresponding author: Fadila Wirawan, Department of Public Health Nutrition, Faculty of Public Health, Universitas Indonesia, Depok 16424, Indonesia, E-mail: fadila.wirawan@gmail.com
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- Pre-pregnancy diet has an important role in preparing for healthy generation. However, evidence on this issue has been scarce. A scoping review synthesising current evidence will support the demand to map ‘what has been researched’ on pre-pregnancy diet and maternal and child health.
-
Methods
- Systematic search was performed using PICOS (Population, Intervention, Comparison, Outcomes, and Study design) framework in electronic databases. Articles were screened for eligibility, summarized, and the quality was assessed using the National Institute of Health assessment tool. The review structure complies with Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guide.
-
Results
- Forty-two articles were included after full-text screening. Twenty-five studies were in high-income countries (HICs), six in each upper-middle income, five in lower-middle income countries (LMICs), and one in low-income countries (LIC). Based on the regions: North America (n=16), Europe (n=5), South America (n=4), Australia (n=4), Asia (n=5), Middle East (n=2), and sub-Saharan Africa (n=1). The two-most observed diet-related exposures were dietary pattern (n=17) and dietary quality (n=12). The most assessed outcome was gestational diabetes mellitus (n=28) and fetal and newborn anthropometry (n=7). The average quality score±standard deviation was 70±18%.
-
Conclusions
- Research related to pre-pregnancy diet is still concentrated in HICs. The context of diet may vary; therefore, future research is encouraged in LMICs and LICs context, and Mediterranean, South-East Asia, Pacific, and African regions. Some maternal and child nutrition-related morbidity, such as anemia and micronutrient deficiencies, have not been discussed. Research on these aspects will benefit to fill in the gaps related to pre-pregnancy diet and maternal and child health.
- Pre-pregnancy or preconception health, not until recently, has come to attention as a window of opportunity to prepare for a healthy pregnancy. Pregnancy itself is not always a prepared event. In the United Kingdom, 45% of pregnancies were unplanned at the time of conception [1], and the rate may be even higher in developing countries with less access to family planning. Preconception health includes a wide range of nutrition and lifestyle aspects, one of which is diet. Healthy diets contribute to preventing malnutrition, and in the long term, reducing the risk of diet-related non-communicable diseases (NCDs) [2]. Studies have observed the associations between pre-pregnancy lifestyle and maternal and child health outcomes [3]. Evidence also suggests that women’s nutritional status before pregnancy is associated with maternal and child outcomes [4]. However, the role of diet before pregnancy in the development of maternal and child outcomes is not much discussed.
- Understanding the role of pre-pregnancy diet in maternal and child health will contribute to maternal and child morbidity and mortality as well as NCDs prevention. Nutritional status is directly influenced by dietary intake, whereas, a healthy diet contributes to macronutrient and micronutrient adequacy and balanced energy [5]. In high-income countries (HICs), child-bearing age women’s diet typically had a high intake of refined sugar and a high-fat diet, but low intakes of fruits, vegetables, and protein source food [3]. The national surveys in some HICs also revealed that the young adult age group have also been reported to have lower than recommended intakes for iodine, iron, and folate, which are important for pregnancy [3,6]. Therefore, it raises concerns about nutritional preparedness in pregnancy.
- Research related to the pre-pregnancy diet are highly diverse. The context of diet is widely affected by socio-cultural, geographical, and economy. The maternal and child health constraints also vary depending on the region and country’s socioeconomic level, leading to the possible differences in the evidence-based application based on regional context. Information related to what evidence is available, what outcomes already measured, and in what context, will support the demand for more evidence on pre-pregnancy diet’s role in future health. This scoping review aims to explore the current evidence of diet in the pre-pregnancy stage to the maternal and child health outcome. A preliminary search of PROSPERO, MEDLINE, the Cochrane Database of Systematic Reviews, and JBI Evidence Synthesis was conducted and no current or in-progress scoping reviews or systematic reviews on the topic were identified. To answer the question of: What have been done in the existing research of pre-pregnancy diet as exposure to maternal and child health outcome?, this scoping review systematically maps the available evidence and identify the gaps for further research.
INTRODUCTION
- This scoping review was structured according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guide for scoping review. The literature search was performed using PICOS (Population, Intervention, Comparison, Outcomes, and Study design) framework (Table 1). The use of PICOS was chosen as the framework includes the necessary observation and more sensitivity for a scoping review related to quantitative health research compared to other frameworks, such as PEOS, SPICE, SPIDER, and others. PICOS framework also provides a comprehensive search that benefits research with limited time and resources [7]. The topic to adhere to was pre-pregnancy or preconception diet and its relation to maternal and/or child health-related outcomes. Pre-pregnancy was defined as the time before conception or pregnancy, which includes the phase in preparing for pregnancy as well as the adolescent period. The diet variable may include nutritional content, food-based supplementation, dietary quality, dietary pattern, and other dietary-related variables, however, did not include non-food-based supplementation and nutritional status. Maternal health was defined as the health-related condition of the mother during the pregnancy, childbirth, and post-natal period [8], therefore did not include the fertility outcome variable. Child health was considered as all aspects of childhood illness starting from birth. Maternal and child health search were combined as a ‘health’ term due to the wider scope of search compared to the use of separated ‘maternal’ and ‘child’ terms. Further selection was conducted in the article identification process.
- The Article Identification
- We conducted a search through some potential bibliographic databases in July 2022. The systematic search was conducted in PubMed, the largest electronic medical bibliography. The search strategy based on the PICOS framework resulted in the use of the following concept filters: (1) pre-pregnancy or preconception; (2) diet; and (3) health. The final search strategy is available in Supplemental Material 1. An additional systematic search using keywords combination of “Pre-pregnancy diet”, “Prepregnancy diet”, “Pre-conception diet”, “Preconception diet”, and “maternal health” and “child health” was also conducted through PubMed to identify more related articles. Articles were filtered for publication in full text in Indonesian or English languages, involving human participants, and article type based on PubMed NCBI filters: reviews, case reports, clinical study, clinical trial, comparative study, controlled clinical trial, multicentre study, observational study, randomized controlled trial (RCT), systematic review, and meta-analysis. Another search attempt was conducted through Indonesia research bibliography; SINTA; Indonesian Scientific Journal Database; and Google Scholar using local keywords for pre-pregnancy diet; “Pola makan prahamil“; “Pola makan prakonsepsi”; and “Pola makan prakehamilan”. Only peer-reviewed articles were included.
- To be included, the article needed to observe pre-pregnancy diet as exposure and maternal and/or child health as the outcome. The article should be peer-reviewed original article, involving human participants, and available in full-text. Articles that are methodological paper, pre-prints, conference article, and in language that was not understood by the authors (aside from English and Bahasa Indonesia) were excluded. The list of inclusion and exclusion criteria can also be found in Supplemental Material 2.
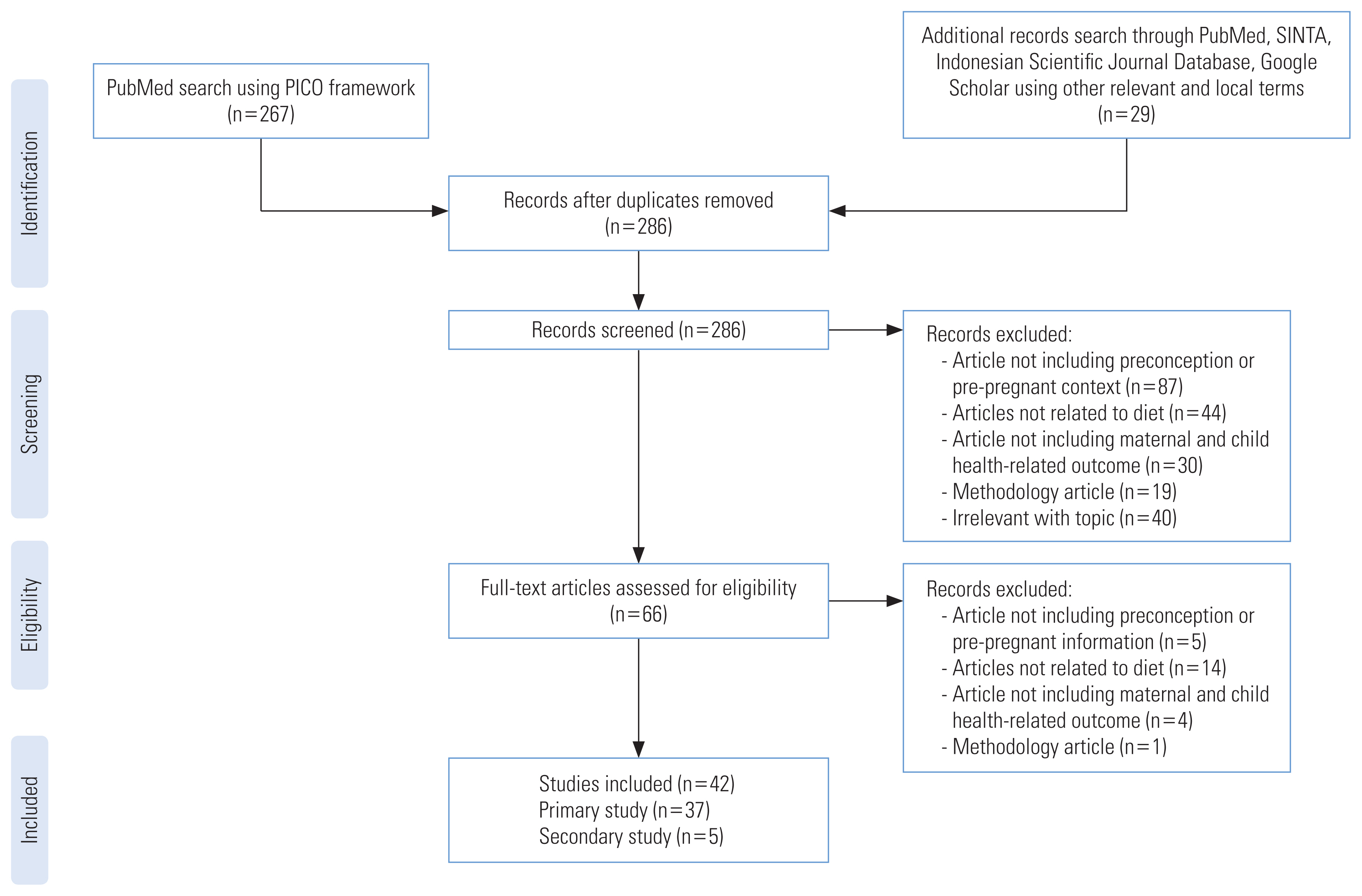
- The Selection of Relevant Articles
- After the articles were cleaned for duplicates, two authors (FW and DGAY), with sufficient capacity to understand English scientific article, each screened for the article separately. The articles were screened by title and abstract for adherence to the topic. The authors then converged their selection of articles to be assessed further for eligibility. Full-text articles were assessed separately by the authors. The final inclusion of the articles in the scoping review was based on the authors’ mutual agreement on the article’s adherence to the topic. In the condition when the authors did not reach a consensus, AG was consulted. The article selection flow was as presented in Figure 1.
- Data Extraction and Quality Appraisal
- After the final article selection, the studies were grouped into primary research (case reports, clinical study, clinical trial, comparative study, controlled clinical trial, multicentre study, observational study, and RCT) and secondary research (review, systematic review, and meta-analysis). The following information was recorded using a Microsoft Excel spreadsheet for primary research; author(s); year of publication; year of data collection; study design; study group (if any); population; sample size; subject’s age group; country; country’s income level; observed or intervention group; outcome variable; time of the assessed diet; dietary assessment method (if any); maternal health finding(s); and child health finding(s). The time of the assessed diet represents the time frame in which the participant is required to recall or report. As for secondary researchs, the following information were recorded; author(s); year of publication; study design; sample size; exposure variable; outcome variable; maternal health finding(s); and child health finding(s). We also summarized the observed maternal and child health outcome for each diet-related variable.
- To provide better insight in the currently available evidence, the quality of the articles were appraised based on the National Institute of Health study quality assessment tool [9] with the FW and DY as the Raters. The overall article’s quality was decided by the average percentage of ‘Yes’ answers on the study quality assessment tools given by the Raters. When no consensus reached by the Raters, AG was consulted. We grouped the article’s quality ratings into three groups; poor (fulfilling less than 33.3% of the criteria); fair (fulfilling 33.3 to 66.6% of the criteria); good (fulfilling more than 66.6% of the criteria). Quality assessment of articles were conducted to evaluate the current quality of evidence available in this review to map the currently available study’s quality, not as a basis of inclusion.
- Protocol Registration
- This scoping review protocol has been registered in the Open Science Framework Registries: https://doi.org/10.17605/OSF.IO/7F9C2.
- Ethics Statement
- This study does not include human subject involvement, therefore exempted for institutional review board approval.
METHODS
- The article identification and selection are presented in Figure 1. A search using the PICOS framework in the PubMed database was conducted and yielded 267 articles after filtering for full-text, language, and types of articles. An additional 29 articles were obtained from linked research, database, and the web. After cleaning for duplicates, 286 articles were screened for adherence to the topic. A total of 42 articles were included after the full-text screening, consisting of 37 primary research articles and five secondary research articles to be included in the current scoping review.
- The Characteristics of the Studies
- The extracted findings from the included primary research were as shown in Table 2 [10–46]. One study is cross-sectional, three are case-control, one is a post-hoc observational study, 27 are cohort, and five studies are RCT. All of the primary studies were quantitative. Out of 42 included studies, 27 of them are based on big projects, mostly based on the Nurses’ Health Study II cohort (13 studies). This scoping review did not use a limiter of date of publication in the search process. However, studies included in the final selection were published in 2009 to 2022.
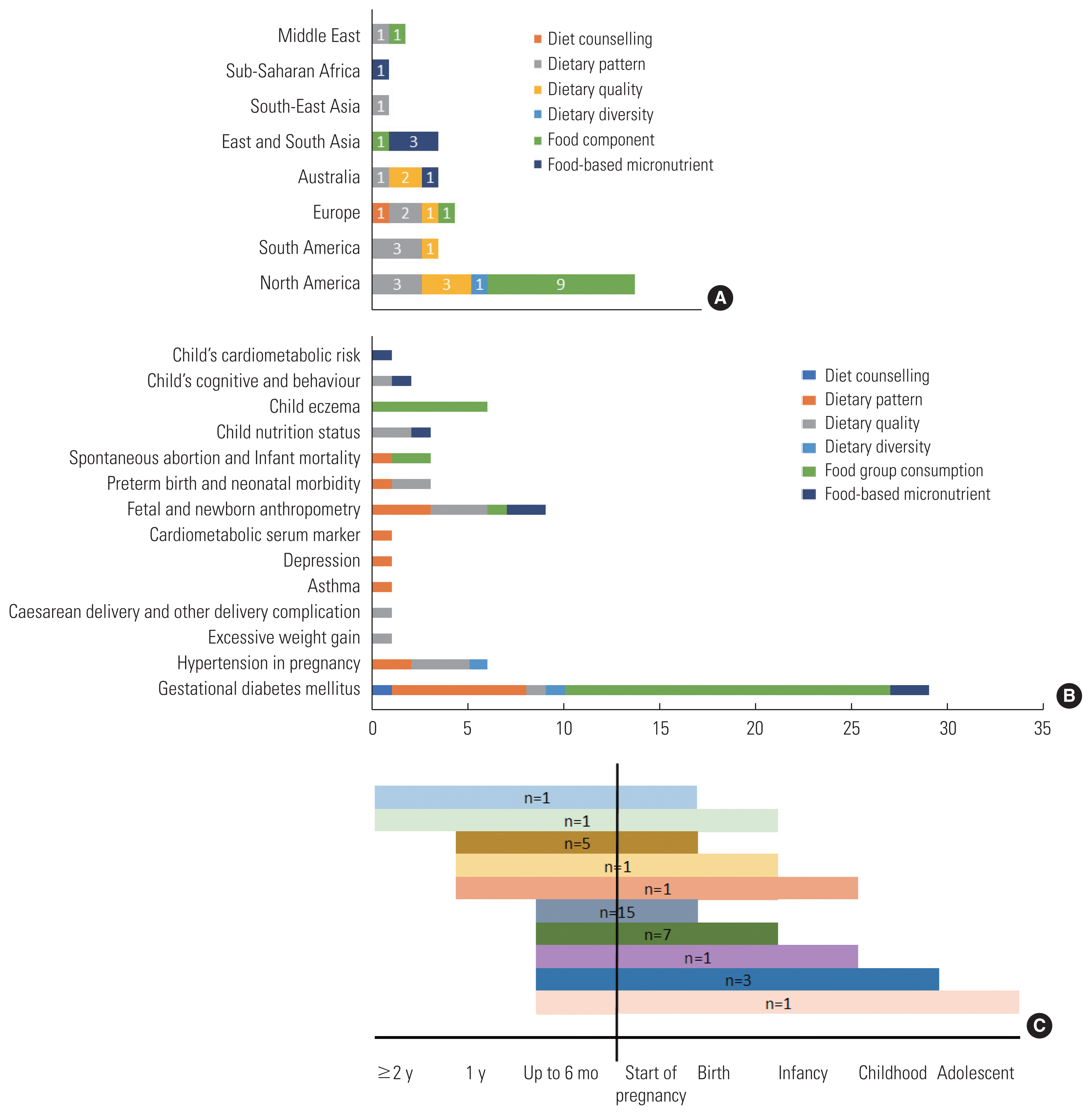
- Of the 42 studies included, 25 studies were conducted in high-income countries (HICs), six in upper-middle-income countries (UMICs), five in lower-middle-income countries (LMICs), and only one was conducted in low-income country (LIC). Based on the geographical areas, 16 were conducted in North America, five were in Europe, four were in South America, four were in Australia, four were in East and South Asia, two were in the Middle East, one in South-East Asia, and one was in sub-Saharan Africa. The proportion of observed pre-pregnancy diet variables based on region was presented in Figure 2A. The pre-pregnancy dietary patterns had been observed in almost all regions but sub-Saharan Africa and East and South Asia. Meanwhile, pre-pregnancy dietary quality research had only been brought up in regions with UMICs and HICs, without any known studies of pre-pregnancy dietary quality from Asia, Middle East, and sub-Saharan Africa. The diet variable as the exposure was mostly (30 studies) measured by food frequency questionnaire (FFQ), other methods used were 24-hour dietary recall, questionnaire, and interview. A total of 13 studies were conducted in the already pregnant population and rely on recall of the diet during the pre-pregnancy phase. Figure 2B shows the type of diet-related variables that were considered as exposures based on the included studies and its maternal and child health outcome variable. The duration of observation from pre-pregnancy to outcome were varied as seen in Figure 2C. The shortest and the most common observation, 15 studies were started no more than six months before pregnancy to observe the outcomes during pregnancy. The longest observation was until adolescent by only one study.
- Table 3 [47–51] presents the findings of secondary studies that are included in the current scoping review. One is meta-analysis, two are systematic reviews, and the other two are reviews. The publication year ranges from 2012 to 2022. One of the systematic reviews is without results because did not find any relevant intervention study related to preconception diet.
- Quality of the Studies
- The quality of the included studies was appraised (Supplemental Material 3) with an average quality score of 70±18%. Most of the observational studies were based on secondary data from a large cohort project. However, the quality assessment was made solely on how the authors’ reporting in the article. Three articles are considered poor, ten articles are fair, and 29 are good (marked in Table 4) [10–46]. Articles with poor quality were the two reviews and one RCT that did not provide enough information related to the study methods. Most of the studies that have fair quality did not mention the justification of the sample size, their study power and effect. The studies with fair quality also did not clearly explain whether the assessors were blinded to the exposure status, therefore, assumed as ‘No’ or ‘Not Clear’. The outcome in the fair studies was self-reported, and therefore considered to have a high risk of bias. Regardless of the rank of quality, most studies in use recall and only measured the exposure once.
- Assessed Diet-related Exposure and Outcomes
- We found 13 observations of dietary patterns and 16 observations of dietary quality (Figure 2B). The discussion of dietary pattern includes various known dietary patterns; Western diet; Prudent diet; Mediterranean diet; alternate Mediterranean diet; Nordic diet; and Diet to Stop Hypertension, and other defined dietary patterns; low caloric diet with controlled micronutrient; energy-dense poor-nutrient diet; and pre-defined healthy diet. Dietary quality includes observation for Healthy Eating Index, alternate Healthy Eating Index, and Prime Diet Quality Score. The mention of dietary pattern or quality score can be found in Table 1.
- Maternal gestational diabetes mellitus (GDM) was the most discussed topic for the maternal outcome, with 28 observations for different diet-related exposures. Hypertension disorder in pregnancy (preeclampsia) and asthma were the second observed maternal outcome (n=4). Meanwhile, fetal and newborn anthropometry was the most observed child health outcome to different diet-related exposures (n=7) followed by preterm birth and neonatal morbidity (n=3).
RESULTS
- The current scoping review observed that, to date, research related to pre-pregnancy diet was mostly conducted in the HIC population. The most observed area was North America (the United States and Canada) and the least observed based on the area was the African region. The dietary pattern and dietary quality were the two-most observed diet-related exposures. The most assessed outcome was GDM, hypertension disorder in pregnancy, and fetal and newborn anthropometry. FFQ was the most common dietary assessment tool used in research related to the pre-pregnancy diet.
- Pregnancy is, most of the time, an unpredictable event. Even in the case of intended pregnancy, the starting point of early pregnancy can be unknown. Therefore, research related to pre-pregnancy diet often requires a long longitudinal observation from exposure to outcome. The time constraint explains the high number of studies that extracted secondary data from big longitudinal study. However, in studies using such method, the exposure and outcome assessments were sometimes cannot be implemented consistently.
- The types of maternal morbidity are varying based on the region and types of economy. Hemorrhage, hypertension and preeclampsia, and sepsis were recognized as the leading cause of maternal mortality in high income countries. Hemorrhage, hypertension, dystocia, and sepsis in sub-Saharan Africa. Hypertension and hemorrhage in North Africa and Middle East. Hemorrhage, hypertension, anemia, and sepsis in Asia. Hypertension, hemorrhage, and infection in Latin America [10]. Hypertension, hemorrhage, and sepsis or infection are problems in all regions and economy, however, only three articles observed four dietary parameters to hypertensive disorder in pregnancy. Pre-pregnancy diet exposure to hemorrhage and infection were not found, but the nature of both etiologies was not directly related to diet and nutrition.
- Anemia is one of the most prevalent maternal morbidities in Asia [52] and globally in LMICs and LICs with global prevalence of 42% in pregnant women [53]. Anemia is highly affected by nutrition [54]. Iron, folic acid, vitamin B12, and vitamin A deficiency, as well as protein energy malnutrition are among the contributing factors of nutritional anemia [53]. A population study in Indonesia shows that pre-pregnancy anemia increased the risk of child anemia in under-5 years old [55]. However, we did not identify any study of pre-pregnancy diet and anemia.
- Malnourished mother’s nutrition is unlikely to suddenly improved during pregnancy due to even increasing nutritional demand. There are risk of insufficient weight gain and chronic energy and micronutrient deficiencies, that contribute to poor birth outcomes, neonatal mortality, and subsequent childhood malnutrition [56]. Newborn mortality incidence was reported the highest in sub-Saharan Africa, followed by Central and South Asia. Most neonatal deaths were related to preterm birth, childbirth-related complications, infections, and birth defects [57]. Malnutrition in children also contributes to under-5 death globally. Stunting and chronic protein-energy malnutrition are prevalent in Africa and Asia, while micronutrient deficiencies, mainly iron, vitamin A, iodine, and zinc, are prevalent in developing countries [56,58,59]. Referring to the burden of child mortality and morbidity, regions with high prevalence of child mortality still had the least number of available research in preconception diet and child health outcome. Micronutrient deficiencies in children are connected to maternal nutrition, such as iron storage in newborns that are affected by maternal iron [60]. In addition, evidence already supports the prevention of birth defects through adequate maternal nutrition, for example folate for neural tube defect prevention [61,62]. Maternal protein malnutrition also linked to hippocampal formation and neurobehavioral development [63,64]. But research related to preconception diet and child micronutrient deficiency, birth defect, and development were still scarce.
- Although the evidence level was still weak, maternal nutrition is associated with intergenerational effects on NCDs risk in adult offspring [65]. Study in epigenetics suggests the role of nutrition in the early phase of life in the development of allergy, metabolic disorders risk, and cancer in the future [66–69]. However, further study is still required, including maternal pre-pregnancy diet’s role in the future NCDs risk.
- Globally, there has been a shift in the diet not only in HICs but also in developing countries. The plant-based diet has been shifted to high-fat, energy-dense diet [70]. Adolescent diet practice is crucial that is likely to extend to adulthood and representative of pre-pregnancy diet [71]. Several research in adolescent dietary quality report the poor dietary habit in adolescent girls in LMICs [71,72]. Pre-pregnancy diet has not been attention in LMICs and LICs, although is recognized as a critical base for birth preparedness and health in the lower economy countries. Some experts agreed that pre-pregnancy care priority of urgency is high due to the remaining-high maternal and child mortality and morbidity in some regions. Research related to pre-pregnancy context also needs to consider different local circumstances and context [73]. The currently available studies were mostly in HICs, which may not be completely suitable for implementation in LMICs and LICs context.
- The current study used systematic search method and additional hand search to obtain more articles that engaged with the topic. The quality of included articles was also assessed by its methodology. The approach also conducted by two assessors, which, lowers the risk of bias. However, some studies related to pre-pregnancy may be missed during the search process. Studies in other language from English and Bahasa were also not included and may cause bias in selection process. The current scoping review also only included primary original research and did not include review and grey literature.
DISCUSSION
- Pre-pregnancy diet is a potential opportunity to prepare for the healthier next generation and stop intergenerational cycle of malnutrition. The current evidence related to pre-pregnancy diet is still limited. Future research is encouraged in LMICs and LICs contexts, as well as South-East Asia, Pacific, and African regions. Some maternal and child nutrition-related morbidity, such as anemia, micronutrient deficiencies, and birth defects have not much or at all discussed yet. More research on these aspects and the regional dietary context will benefit to fill in the gaps related to pre-pregnancy diet and maternal and child health.
CONCLUSION
SUPPLEMENTAL MATERIALS
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Wirawan F, Gayatri A. Data curation: Wirawan F, Yudhantari DGA, Gayatri A. Formal analysis: Wirawan F, Yudhantari DGA, Gayatri A. Funding acquisition: None. Methodology: Wirawan F, Yudhantari DGA, Gayatri A. Project administration: Wirawan F. Visualization: Wirawan F. Writing – original draft: Wirawan F, Yudhantari DGA, Gayatri A. Writing – review & editing: Wirawan F, Yudhantari DGA, Gayatri A.
Notes
ACKNOWLEDGEMENTS
| Study | Year of data collection | Study design | Study group | Population | Sample size | Subject’s age (y) | Country | Country’s income level1 | Exposure/intervention variable | Outcome variable | Time of the assessed diet | Dietary assessment method | Maternal health finding(s) | Child health finding(s) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alves-Santos et al., 2019 [16] | 2009–2012 | Cohort | NA | Pregnant women | 193 | 20–40 | Brazil | Upper-middle | Pre-pregnancy dietary pattern | LGA, birth length, Apgar score, and preterm birth | Recall 6 mo before pregnancy | Semi-quantitative FFQ | NA | Fast food and candies were associated with higher LGA; “beans, bread, and fat” was associated with lower Apgar score; and “vegetables and dairy” was associated with lower preterm birth |
| Asadi et al., 2019 [11] | 2014–2015 | Case-control | NA | Pregnant women | 296 | 19–40 | Iran | Lower-middle | Pre-pregnancy dietary pattern history | GDM | Recall of diet in the previous year | FFQ | Prudent diet was associated with lower risk of GDM | NA |
| Bao et al., 2013 [35] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 294 | 25–44 | USA | High | Protein intake | GDM | Before pregnant | Semi-quantitative FFQ | Red meat consumption was associated with GDM; Nut intake was associated with a lower risk of GDM | NA |
| Bao et al., 2014 [31] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 027 | 25–44 | USA | High | Fried-food consumption | GDM | Before pregnant | FFQ | Fried food consumption was associated with GDM risk | NA |
| Bao et al., 2014 [12] | 1989–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 21 411 | 25–44 | USA | High | Low-carbohydrate diet | GDM | Before pregnant | Semi-quantitative FFQ | Low-carbohydrate, high animal protein, and animal fat diet were associated with increased GDM risk | NA |
| Bao et al., 2016 [38] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 632 | 25–44 | USA | High | Potato intake | GDM | Before pregnant | Semi-quantitative FFQ | Higher potato consumption was significantly associated with an increased risk of GDM | NA |
| Bao et al., 2018 [43] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 225 | 24–44 | USA | High | Dietary vitamin D intake | GDM | Before pregnant | FFQ | Dietary and total vitamin D intakes were inversely associated with GDM risk | NA |
| Benaim et al., 2018 [19] | 2009–2011 | Cohort | NA | Pregnant women | 154 | 22–31 | Brazil | Upper-middle | Food intake 6 mo before pregnant | Changes of serum EPA and DHA, total n-3 PUFA, total n-6 PUFA, and omega-6/omega-3 ratio during pregnancy | Recall of diet 6 mo before pregnant | Semi-quantitative FFQ | Healthy dietary pattern was associated with serum fatty acids, however the effect was modified by BMI | NA |
| Bowers et al., 2012 [33] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 13 475 | 22–44 | USA | High | Fat intake | GDM | Before pregnant | Semi-quantitative FFQ | Higher consumption of dietary cholesterol and animal fat was associated with GDM | NA |
| Chen et al., 2009 [41] | 1992–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 13 475 | 24–44 | USA | High | Sugar-sweeetend beverage intake | GDM | Before pregnant | Semi-quantitative FFQ | Sugar-sweetened cola was associated with the risk of GDM | NA |
| Chen et al., 2012 [37] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 13 475 | 24–44 | USA | High | Fruit and fruit juice intake | GDM | Before pregnant | Semi-quantitative FFQ | Apple intake was associated with lower risk of GDM | NA |
| Chen et al., 2019 [39] | 2018 | Case-control | NA | Pregnant women | 260 | Child-bearing age | China | Upper-middle | Pre-pregnancy probiotic yogurt intake | GDM | Recall | Structured questionnaire | No association | NA |
| Dhana et al., 2018 [28] | 1989–2013 | Cohort | Nurses’ Health Study II | Non-pregnant women | 4698 | 25–42 | USA | High | Alternate HEI 2010 | BMI of offspring | Before pregnant | FFQ | NA | No association |
| Gaskins et al., 2014 [22] | 1992–2009 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 950 | 24–44 | USA | High | Alternate HEI 2010, alternate MeD, and fertility diet | Pregnancy loss | Before pregnant | Semi-quantitative FFQ | No association | |
| Gaskins et al., 2018 [40] | 1991–2009 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 590 | 24–44 | USA | High | Coffee intake | Spontaneous abortion | Before pregnant | FFQ | NA | High coffee consumption was associated with the increased risk of spontaneous abortion |
| Gete et al., 2021 [30] | 2003–2016 | Cohort | Australian Longitudinal Study in Women’s Health (ALSWH) and Mother and Their Children’s Health Study (MatCH) | Non-pregnant women | 1554 | 25–30 | Australia | High | HEI 2015 | Child behavioral problems using Strengths and Difficulties Questionnaire (SDQ) | Before pregnant | Semi-quantitative FFQ | NA | Better diet quality was associated with lower risk of offspring total behavioral difficulties, externalizing score, hyperactivity, and peer problems |
| Gete et al., 2021 [29] | 1996–2015 | Cohort | ALSWH and MatCH | Non-pregnant women | 1936 | 18–23 | Australia | High | HEI 2015 | Childhood BMI of the offspring | Before pregnant | Semi-quantitative FFQ | NA | High diet quality was associated with reduced risk of underweight and obesity |
| Gicevic et al., 2018 [25] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 41 229 | 24–44 | USA | High | Dietary diversity (FGI and MDD-W) and dietary quality (alternate HEI 2010 and PDQS) | GDM and hypertensive disorder in pregnancy | Before pregnant | Semi-quantitative FFQ | Alternate HEI-2010 and PDQS were associated with a lower risk of GDM | NA |
| Grieger et al., 2016 [17] | 2009–2013 | Cross-sectional | NA | Pregnant asthmatic women | 309 | >18 | Australia | High | Pre-pregnancy protein; fat and sugar; and vegetarian diet | Asthma control | Recall 12 mo before pregnancy | FFQ | High fat and sugar diet was associated with uncontrolled asthma | NA |
| Grieger et al., 2019 [32] | 2009–2013 | Cohort | NA | Pregnant women | 234 | >18 | Australia | High | Food intake 12 mo before pregnant | Allergies in children | Recall of diet 12 mo before pregnant | FFQ | NA | Dairy, fresh fruit, unsaturated and saturated spreads, takeaway foods, and non-oily fish were protective against some types of allergies. Poultry and fruit juice were adversely associated with allergy |
| Hillesund et al., 2018 [23] | 2009–2013 | Post-hoc observational study | Norwegian Fit for Delivery (NFFD) | Pregnant women | 591 | >18 | Norway | High | NFFD diet score pre-pregnancy recall | Gestational weight gain, preterm delivery, birth anthropometry, GDM, preeclampsia | Recall | FFQ | A higher diet score was associated with a lower risk of excessive weight gain | A higher diet score was associated with a lower risk of preterm delivery |
| Jarman et al., 2018 [24] | 2009–2012 | Cohort | Alberta Pregnancy Outcomes and Nutrition (APrON) study | Pregnant women | 1598 | >16 | Canada | High | Pre-pregnancy healthy eating pattern score | Gestational hypertension and GDM | Recall of diet 12 mo before pregnancy | FFQ | A higher healthy eating pattern score was associated with lower odds of gestational hypertension | NA |
| Lamyian et al., 2017 [34] | 2010–2011 | Cohort | NA | Pregnant women in prenatal clinic | 1054 | 18–45 | Iran | Lower-middle | Fast food consumption in the previous year | GDM | Recall of diet in previous year | Semi-quantitative FFQ | Fast food intake was significantly associated with increased risk of developing GDM | NA |
| Lawande et al., 2018 [44] | 2006–2012 | RCT | Mumbai Maternal Nutrition Project | Non-pregnant women | 6513 | 22–28 | India | Lower-middle | Food-based micronutrient-rich snack | Fetal size and growth | Before pregnant | NA | NA | No association |
| Van Lippevelde et al., 2021 [20] | 1995–2008 | Cohort | Young-HUNT study | Adolescent | 8980 | <19 | Norway | High | Dietary and meal patterns | Birth anthropometry | Before pregnant | Self-reported questionnaire | NA | Higher energy-dense food consumption was associated with the risk of LBW |
| Mari-Sanchis et al., 2018 [36] | 1999–2012 | Cohort | The SUN Project | Non-pregnant women | 3298 | Child-bearing age | Spain | High | Meat consumption and iron intake | GDM | Up to 2 y before pregnant | Semi-quantitative FFQ | Higher meat consumption associated with increased risk of GDM | NA |
| Mohammed et al., 2020 [42] | 2011–2014 | RCT | NA | Non-pregnant women | 1220 | ≥18 | Ethiopia | Low | Iodized salt intervention | Cognition of offspring | Before pregnant | 24-hr food frequency interview | NA | Offspring’s cognitive scores were better in intervention group compared to control |
| Olmedo-Requena et al., 2019 [13] | n/a | Case-control | NA | Pregnant women with GDM | 1466 | >18 | Spain | High | Pregnancy with GDM | Pre-pregnancy adherence to MeD | Recall of diet in previous year before pregnant | FFQ | Very high adherence to MeD was associated with reduced GDM case; Low consumption of meat and its derivatives were protective of GDM | NA |
| Potdar et al., 2014 [45] | 2006–2012 | RCT | Mumbai Maternal Nutrition Project | Non-pregnant women | 6513 | <40 | India | Lower-middle | Micronutrient-rich vegetarian snack | Birth weight | ≥90 day before last menstrual period | NA | NA | Micronutrient-rich snack was associated higher birth weight and lower low-birth weight outcome |
| Sahariah et al., 2022 [46] | 2006–2011 | RCT | Mumbai Maternal Nutrition Project | Non-pregnant women | 1255 | Child-bearing age | India | Lower-middle | Micronutrient-rich vegetarian snack | Cardiometabolic risk markers and body composition in offspring (5–10 y follow up after intervention) | Before pregnant | NA | NA | No association |
| Siega-Riz et al., 2021 [27] | 2008–2011 | Cohort | Hispanic Community Health Study | Non-pregnant women | 497 | 18–44 | USA | High | HEI 2010 | infant birth weight | Mean of 3.2 y before pregnancy | 24-hr food recall | NA | High dietary quality was associated with infant birth weight |
| Teixeira et al., 2021 [21] | 2011–2013 | Cohort | ProcriAr study | Pregnant women | 299 | Child-bearing age | Brazil | Upper-middle | Pre-pregnancy dietary pattern | Newborn anthropometry | Recall of diet in previous 12 mo | FFQ | NA | Energy-dense nutrient-poor pre-pregnancy diet was a risk factor for SGA newborn |
| Tobias et al., 2012 [14] | 1991–2001 | Cohort | Nurses’ Health Study II | Non-pregnant women | 15 254 | 24–44 | USA | High | MeD, DASH, and alternate HEI scores | GDM | Before pregnant | Semi-quantitative FFQ | Adherence to alternate MeD, DASH, and alternate HEI dietary patterns was associated with lower GDM risk | NA |
| Valkama et al., 2018 [10] | 2008–2014 | RCT | RADIEL Study | Non-pregnant women | 75 | ≥18 | Finland | High | Dietary counselling and diet | GDM | Before pregnant | FFQ | Low-fat cheese consumption was associated with lower GDM risk | NA |
| Vilela et al., 2014 [18] | 2009–2011 | Cohort | NA | Pregnant women | 248 | 20–40 | Brazil | Upper-middle | Pre-pregnancy dietary pattern | Depressive symptoms during pregnancy | Recall 6 mo before pregnancy | Semi-quantitative FFQ | Health dietary pattern was associated with lower risk of depressive symptoms | NA |
| Yee et al., 2020 [26] | 2010–2013 | Cohort | The Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-To-Be (nuMoM2b) | Pregnant women | 8259 | >13 | USA | High | Preconception HEI 2010 | Maternal pregnancy morbidities and child birth outcomes | Recall of diet 3 mo before conception | Semi-quantitative FFQ | Poor dietary quality was associated with postpartum hemorrhage, hypertensive disorder in pregnancy, and caesarean delivery | Poor dietary quality was associated with higher preterm birth, NICU admission, SGA, and LBW, however lower risk of macrosomia |
| Yong et al., 2020 [15] | Cohort | TheSeremban Cohort Study (SECOST) | Pregnant women | 737 | Child-bearing age | Malaysia | Upper-middle | Pre-pregnancy dietary pattern | GDM | Recall of diet before pregnancy in the first trimester | Semi-quantitative FFQ | High sugar and fat diet reduced the risk of GDM | NA |
RCT, randomized controlled trial; FFQ, Food-frequency questionnaire; HEI, Healthy Eating Index; MeD, Mediterranean diet; DASH, dietary approach to stop hypertension; NFFD, Norwegian fit for delivery diet; FGI, Food Groups Index; MDD-W, minimum dietary diversity for women; PDQS, Prime Diet Quality Score; GDM, gestational diabetes mellitus; NICU, neonatal intensive care unit; LGA, large-for-gestational age; SGA, small-for-gestational age; LBW, low birth weight; EPA, eicosapentaenoic acid; PUFA, polyunsaturated fatty acid; BMI, body mass index; NA, not available.
1 World Bank classification.
| Study | Study design | Sample size (study) | Exposure variable | Outcome variable | Maternal health finding(s) | Child health finding(s) |
|---|---|---|---|---|---|---|
| Cui et al., 2021 [47] | Meta-analysis | 38 | Pre-pregnancy diet | GDM | Higher pre-pregnancy consumption of fried food, fast food, red and processed meat, heme iron, and low-carbohydrate diet pattern were associated with increased risk of gestational diabetes mellitus; Higher intake of dietary fiber was associated with lower risk of gestational diabetes mellitus | High pre-pregnancy caffeine intake was associated with increased risk of small-for-gestational age. |
| Tieu et al., 2017 [48] | Systematic review | 0 | Interconception intervention | Maternal and child morbidity | NA | NA |
| Stephenson et al., 2018 [49] | Review | NA | Preconception diet | Maternal and child morbitdity | Diet before pregnancy may modify maternal outcomes through BMI status and micronutrient deficiency | Diet before pregnancy may modify prenatal outcomes through BMI status and micronutrient deficiency |
| Temel et al., 2014 [50] | Systematic review | 44 | Preconceptional nutrition support | Maternal and child health | NA | Long-term nutritional support was associated with a positive effect on birth weight |
| Hanson et al., 2012 [51] | Review | NA | Pre-pregnancy diet | NCD | NA | Maternal diet before pregnancy are related to phenotypic characteristics of the child, such as adiposity at birth and in childhood, and markers of cardiovascular risk |
| Pre-pregnancy diet variables | Observed outcome | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||||||
| Maternal outcome | Child outcome | ||||||||||||||
|
|
|
||||||||||||||
| GDM | Hypertension in pregnancy | Nutritional status | Type of delivery | Asthma | Depression | Cardiometabolic serum marker | Fetal and newborn anthropometry | Preterm birth and neonatal morbidity | Spontaneous abortion and Infant mortality | Child nutrition status | Allergy and eczema | Cognitive and behaviour | Cardiometabolic risk | Total (n) | |
| Diet counselling | [10] | 1 | |||||||||||||
|
|
|||||||||||||||
| Dietary pattern | [11]1, [12]1, [13]1, [14], [15]1 | [16]1 | [17] | [18] | [19]1 | [20]1, [21]1 | [16]1 | [22] | 13 | ||||||
|
|
|||||||||||||||
| Dietary quality | [23]1, [24]1, [25]1 | [23]1, [25]1, [26]1 | [23]1 | [26]1 | [23]1, [26]1, [27]1 | [23]1, [26]1 | [28]1, [29] | [30] | 16 | ||||||
|
|
|||||||||||||||
| Dietary diversity | [25]1 | [25]1 | 2 | ||||||||||||
|
|
|||||||||||||||
| Food component | |||||||||||||||
|
|
|||||||||||||||
| Fried food | [31]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| General food | [32] | 1 | |||||||||||||
|
|
|||||||||||||||
| Dietary fat | [33]1 | [17] | 2 | ||||||||||||
|
|
|||||||||||||||
| Fast food | [10], [34]1 | 2 | |||||||||||||
|
|
|||||||||||||||
| Dairy | [10] | 1 | |||||||||||||
|
|
|||||||||||||||
| Protein intake | [10], [35]1, | [17] | 3 | ||||||||||||
|
|
|||||||||||||||
| Meat | [36]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| Fish | [10] | 1 | |||||||||||||
|
|
|||||||||||||||
| Fruit | [10], [37] | 2 | |||||||||||||
|
|
|||||||||||||||
| Vegetables and legumes | [10] | 1 | |||||||||||||
|
|
|||||||||||||||
| Potato | [38]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| Bread, cereal, grains | [10] | 1 | |||||||||||||
|
|
|||||||||||||||
| Probiotic yogurt | [39]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| Caffeine | [40]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| Sugar-sweetened beverage and sugary snacks | [10], [41]1 | [17] | 3 | ||||||||||||
|
|
|||||||||||||||
| Food-based micronutrient | |||||||||||||||
|
|
|||||||||||||||
| Iodized salt intake | [42]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| Dietary vitamin D | [43]1 | 1 | |||||||||||||
|
|
|||||||||||||||
| Food-based micronutrient-rich snack | [44], [45] | [46] | 3 | ||||||||||||
|
|
|||||||||||||||
| Total (n) | 28 | 4 | 1 | 2 | 4 | 1 | 1 | 7 | 3 | 2 | 2 | 1 | 2 | 1 | |
- 1. Public Health England. Health matters: reproductive health and pregnancy planning; 2018 [cited 2022 Jul 23]. Available from: https://www.gov.uk/government/publications/health-matters-reproductive-health-and-pregnancy-planning/health-matters-reproductive-health-and-pregnancy-planning
- 2. World Health Organization. Sustainable healthy diets: guiding principles; 2019 [cited 2022 Jul 23]. Available from: https://www.who.int/publications/i/item/9789241516648
- 3. Stephenson J, Heslehurst N, Hall J, Schoenaker DA, Hutchinson J, Cade JE, et al. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018;391(10132):1830-1841ArticlePubMedPMC
- 4. Li C, Zhu N, Zeng L, Dang S, Zhou J, Pei L, et al. Effect of maternal pre-pregnancy underweight and average gestational weight gain on physical growth and intellectual development of early school-aged children. Sci Rep 2018;8(1):12014ArticlePubMedPMCPDF
- 5. National Research Council (US) Committee on Diet and Health. Diet and health: implications for reducing chronic disease risk. Washington, D.C: National Academies Press; 1989. p. 1-3
- 6. United Nations Children’s Fund (UNICEF). Maternal nutrition: preventing malnutrition in pregnant and breastfeeding women; [cited 2022 Jul 23]. Available from: https://www.unicef.org/nutrition/maternal
- 7. Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014;14: 579ArticlePubMedPMCPDF
- 8. World Health Organization. Maternal health; [cited 2022 Jul 30]. Available from: https://www.who.int/health-topics/maternal-health#tab=tab_1
- 9. National Heart, Lung, and Blood Institute. Study quality assessment tools; 2021 [cited 2022 Jul 30]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 10. Valkama AJ, Meinilä J, Koivusalo S, Lindström J, Rönö K, Stach-Lempinen B, et al. The effect of pre-pregnancy lifestyle counselling on food intakes and association between food intakes and gestational diabetes in high-risk women: results from a randomised controlled trial. J Hum Nutr Diet 2018;31(3):301-305ArticlePubMedPDF
- 11. Asadi M, Shahzeidi M, Nadjarzadeh A, Hashemi Yusefabad H, Mansoori A. The relationship between pre-pregnancy dietary patterns adherence and risk of gestational diabetes mellitus in Iran: a case-control study. Nutr Diet 2019;76(5):597-603ArticlePubMedPDF
- 12. Bao W, Bowers K, Tobias DK, Olsen SF, Chavarro J, Vaag A, et al. Prepregnancy low-carbohydrate dietary pattern and risk of gestational diabetes mellitus: a prospective cohort study. Am J Clin Nutr 2014;99(6):1378-1384ArticlePubMedPMC
- 13. Olmedo-Requena R, Gómez-Fernández J, Amezcua-Prieto C, Mozas-Moreno J, Khan KS, Jiménez-Moleón JJ. Pre-pregnancy adherence to the mediterranean diet and gestational diabetes mellitus: a case-control study. Nutrients 2019;11(5):1003ArticlePubMedPMC
- 14. Tobias DK, Zhang C, Chavarro J, Bowers K, Rich-Edwards J, Rosner B, et al. Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes mellitus. Am J Clin Nutr 2012;96(2):289-295ArticlePubMedPMC
- 15. Yong HY, Mohd Shariff Z, Mohd Yusof BN, Rejali Z, Appannah G, Bindels J, et al. The association between dietary patterns before and in early pregnancy and the risk of gestational diabetes mellitus (GDM): data from the Malaysian SECOST cohort. PLoS One 2020;15(1):e0227246ArticlePubMedPMC
- 16. Alves-Santos NH, Cocate PG, Benaim C, Farias DR, Emmett PM, Kac G. Prepregnancy dietary patterns and their association with perinatal outcomes: a prospective cohort study. J Acad Nutr Diet 2019;119(9):1439-1451ArticlePubMed
- 17. Grieger JA, Grzeskowiak LE, Wood LG, Clifton VL. Asthma control in pregnancy is associated with pre-conception dietary patterns. Public Health Nutr 2016;19(2):332-338ArticlePubMed
- 18. Vilela AA, Farias DR, Eshriqui I, Vaz Jdos S, Franco-Sena AB, Castro MB, et al. Prepregnancy healthy dietary pattern is inversely associated with depressive symptoms among pregnant Brazilian women. J Nutr 2014;144(10):1612-1618ArticlePubMed
- 19. Benaim C, Freitas-Vilela AA, Pinto TJ, Lepsch J, Farias DR, Dos Santos Vaz J, et al. Early pregnancy body mass index modifies the association of pre-pregnancy dietary patterns with serum polyunsaturated fatty acid concentrations throughout pregnancy in Brazilian women. Matern Child Nutr 2018;14(1):e12480ArticlePubMedPDF
- 20. Van Lippevelde W, Vik FN, Wills AK, Strömmer ST, Barker ME, Skreden M, et al. The impact of diet during adolescence on the neonatal health of offspring: evidence on the importance of preconception diet. The HUNT study. J Dev Orig Health Dis 2021;12(5):798-810ArticlePubMed
- 21. Teixeira JA, Hoffman DJ, Castro TG, Saldiva SR, Francisco RP, Vieira SE, et al. Pre-pregnancy dietary pattern is associated with newborn size: results from ProcriAr study. Br J Nutr 2021;126(6):903-912ArticlePubMed
- 22. Gaskins AJ, Rich-Edwards JW, Hauser R, Williams PL, Gillman MW, Penzias A, et al. Prepregnancy dietary patterns and risk of pregnancy loss. Am J Clin Nutr 2014;100(4):1166-1172ArticlePubMedPMC
- 23. Hillesund ER, Bere E, Sagedal LR, Vistad I, Seiler HL, Torstveit MK, et al. Pre-pregnancy and early pregnancy dietary behavior in relation to maternal and newborn health in the Norwegian Fit for Delivery study - a post hoc observational analysis. Food Nutr Res; 2018 doi:https://doi.org/10.29219/fnr.v62.1273 Article
- 24. Jarman M, Mathe N, Ramazani F, Pakseresht M, Robson PJ, Johnson ST, et al. Dietary patterns prior to pregnancy and associations with pregnancy complications. Nutrients 2018;10(7):914ArticlePubMedPMC
- 25. Gicevic S, Gaskins AJ, Fung TT, Rosner B, Tobias DK, Isanaka S, et al. Evaluating pre-pregnancy dietary diversity vs. dietary quality scores as predictors of gestational diabetes and hypertensive disorders of pregnancy. PLoS One 2018;13(4):e0195103ArticlePubMedPMC
- 26. Yee LM, Silver RM, Haas DM, Parry S, Mercer BM, Iams J, et al. Quality of periconceptional dietary intake and maternal and neonatal outcomes. Am J Obstet Gynecol 2020;223(1):121.e1-121.e8ArticlePubMedPMC
- 27. Siega-Riz AM, Vladutiu CJ, Butera NM, Daviglus M, Gellman M, Isasi CR, et al. Preconception diet quality is associated with birth weight for gestational age among women in the Hispanic community health study/study of Latinos. J Acad Nutr Diet 2021;121(3):458-466ArticlePubMed
- 28. Dhana K, Zong G, Yuan C, Schernhammer E, Zhang C, Wang X, et al. Lifestyle of women before pregnancy and the risk of offspring obesity during childhood through early adulthood. Int J Obes (Lond) 2018;42(7):1275-1284ArticlePubMedPMCPDF
- 29. Gete DG, Waller M, Mishra GD. Pre-pregnancy diet quality is associated with lowering the risk of offspring obesity and underweight: finding from a prospective cohort study. Nutrients 2021;13(4):1044ArticlePubMedPMC
- 30. Gete DG, Waller M, Mishra GD. Pre-pregnancy diet quality and its association with offspring behavioral problems. Eur J Nutr 2021;60(1):503-515ArticlePubMedPDF
- 31. Bao W, Tobias DK, Olsen SF, Zhang C. Pre-pregnancy fried food consumption and the risk of gestational diabetes mellitus: a prospective cohort study. Diabetologia 2014;57(12):2485-2491ArticlePubMedPMCPDF
- 32. Grieger JA, Pelecanos AM, Hurst C, Tai A, Clifton VL. Pre-conception maternal food intake and the association with childhood allergies. Nutrients 2019;11(8):1851ArticlePubMedPMC
- 33. Bowers K, Tobias DK, Yeung E, Hu FB, Zhang C. A prospective study of prepregnancy dietary fat intake and risk of gestational diabetes. Am J Clin Nutr 2012;95(2):446-453ArticlePubMedPMC
- 34. Lamyian M, Hosseinpour-Niazi S, Mirmiran P, Moghaddam Banaem L, Goshtasebi A, Azizi F. Pre-pregnancy fast food consumption is associated with gestational diabetes mellitus among Tehranian women. Nutrients 2017;9(3):216ArticlePubMedPMC
- 35. Bao W, Bowers K, Tobias DK, Hu FB, Zhang C. Prepregnancy dietary protein intake, major dietary protein sources, and the risk of gestational diabetes mellitus: a prospective cohort study. Diabetes Care 2013;36(7):2001-2008PubMedPMC
- 36. Marí-Sanchis A, Díaz-Jurado G, Basterra-Gortari FJ, de la Fuente-Arrillaga C, Martínez-González MA, Bes-Rastrollo M. Association between pre-pregnancy consumption of meat, iron intake, and the risk of gestational diabetes: the SUN project. Eur J Nutr 2018;57(3):939-949ArticlePubMedPDF
- 37. Chen L, Hu FB, Yeung E, Tobias DK, Willett WC, Zhang C. Prepregnancy consumption of fruits and fruit juices and the risk of gestational diabetes mellitus: a prospective cohort study. Diabetes Care 2012;35(5):1079-1082PubMedPMC
- 38. Bao W, Tobias DK, Hu FB, Chavarro JE, Zhang C. Pre-pregnancy potato consumption and risk of gestational diabetes mellitus: prospective cohort study. BMJ 2016;352: h6898ArticlePubMedPMC
- 39. Chen X, Jiang X, Huang X, He H, Zheng J. Association between probiotic yogurt intake and gestational diabetes mellitus: a case-control study. Iran J Public Health 2019;48(7):1248-1256ArticlePubMedPMCPDF
- 40. Gaskins AJ, Rich-Edwards JW, Williams PL, Toth TL, Missmer SA, Chavarro JE. Pre-pregnancy caffeine and caffeinated beverage intake and risk of spontaneous abortion. Eur J Nutr 2018;57(1):107-117ArticlePubMedPMCPDF
- 41. Chen L, Hu FB, Yeung E, Willett W, Zhang C. Prospective study of pre-gravid sugar-sweetened beverage consumption and the risk of gestational diabetes mellitus. Diabetes Care 2009;32(12):2236-2241ArticlePubMedPMCPDF
- 42. Mohammed H, Marquis GS, Aboud F, Bougma K, Samuel A. Pre-pregnancy iodized salt improved children’s cognitive development in randomized trial in Ethiopia. Matern Child Nutr 2020;16(3):e12943ArticlePubMedPMCPDF
- 43. Bao W, Song Y, Bertrand KA, Tobias DK, Olsen SF, Chavarro JE, et al. Prepregnancy habitual intake of vitamin D from diet and supplements in relation to risk of gestational diabetes mellitus: a prospective cohort study. J Diabetes 2018;10(5):373-379ArticlePubMedPMCPDF
- 44. Lawande A, Di Gravio C, Potdar RD, Sahariah SA, Gandhi M, Chopra H, et al. Effect of a micronutrient-rich snack taken preconceptionally and throughout pregnancy on ultrasound measures of fetal growth: the Mumbai Maternal Nutrition Project (MMNP). Matern Child Nutr 2018;14(1):e12441ArticlePubMedPMCPDF
- 45. Potdar RD, Sahariah SA, Gandhi M, Kehoe SH, Brown N, Sane H, et al. Improving women’s diet quality preconceptionally and during gestation: effects on birth weight and prevalence of low birth weight--a randomized controlled efficacy trial in India (Mumbai Maternal Nutrition Project). Am J Clin Nutr 2014;100(5):1257-1268ArticlePubMedPMC
- 46. Sahariah SA, Gandhi M, Chopra H, Kehoe SH, Johnson MJ, di Gravio C, et al. Body composition and cardiometabolic risk markers in children of women who took part in a randomized controlled trial of a preconceptional nutritional intervention in Mumbai, India. J Nutr 2022;152(4):1070-1081ArticlePubMedPMCPDF
- 47. Cui Y, Liao M, Xu A, Chen G, Liu J, Yu X, et al. Association of maternal pre-pregnancy dietary intake with adverse maternal and neonatal outcomes: a systematic review and meta-analysis of prospective studies. Crit Rev Food Sci Nutr; 2021 doi:https://doi.org/10.1080/10408398.2021.1989658 Article
- 48. Tieu J, Shepherd E, Middleton P, Crowther CA. Dietary advice interventions in pregnancy for preventing gestational diabetes mellitus. Cochrane Database Syst Rev 2017;1(1):CD006674ArticlePubMedPMC
- 49. Stephenson J, Heslehurst N, Hall J, Schoenaker DA, Hutchinson J, Cade JE, et al. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018;391(10132):1830-1841ArticlePubMedPMC
- 50. Temel S, van Voorst SF, Jack BW, Denktaş S, Steegers EA. Evidence-based preconceptional lifestyle interventions. Epidemiol Rev 2014;36: 19-30ArticlePubMed
- 51. Hanson MA, Gluckman PD, Ma RC, Matzen P, Biesma RG. Early life opportunities for prevention of diabetes in low and middle income countries. BMC Public Health 2012;12: 1025ArticlePubMedPMCPDF
- 52. Geller SE, Koch AR, Garland CE, MacDonald EJ, Storey F, Lawton B. A global view of severe maternal morbidity: moving beyond maternal mortality. Reprod Health 2018;15(Suppl 1):98ArticlePubMedPMCPDF
- 53. Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet 2011;378(9809):2123-2135ArticlePubMed
- 54. Ryan LM, Mahmood MA, Laurence CO. Incidence of concomitant illnesses in pregnancy in Indonesia: estimates from 1990–2019, with projections to 2030. Lancet Reg Health West Pac 2021;10: 100139ArticlePubMedPMC
- 55. Wirawan F, Nurrika D. Maternal pre-pregnancy anemia and childhood anemia in Indonesia: a risk assessment using a population-based prospective longitudinal study. Epidemiol Health 2022;44: e2022100ArticlePubMedPMCPDF
- 56. Ahmed T, Hossain M, Sanin KI. Global burden of maternal and child undernutrition and micronutrient deficiencies. Ann Nutr Metab 2012;61(Suppl 1):8-17ArticlePubMedPDF
- 57. World Health Organization. Infant mortality; [cited 2022 Sep 22]. Available from: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/infant-mortality
- 58. Dhaded SM, Hambidge KM, Ali SA, Somannavar M, Saleem S, Pasha O, et al. Preconception nutrition intervention improved birth length and reduced stunting and wasting in newborns in South Asia: the Women First Randomized Controlled Trial. PLoS One 2020;15(1):e0218960ArticlePubMedPMC
- 59. Young MF, Ramakrishnan U. Maternal undernutrition before and during pregnancy and offspring health and development. Ann Nutr Metab 2020;76(suppl 3):41-53ArticlePDF
- 60. Shukla AK, Srivastava S, Verma G. Effect of maternal anemia on the status of iron stores in infants: a cohort study. J Family Community Med 2019;26(2):118-122ArticlePubMedPMC
- 61. Yang J, Cheng Y, Zeng L, Dang S, Yan H. Maternal dietary diversity during pregnancy and congenital heart defects: a case-control study. Eur J Clin Nutr 2021;75(2):355-363ArticlePubMedPDF
- 62. Dean SV, Lassi ZS, Imam AM, Bhutta ZA. Preconception care: nutritional risks and interventions. Reprod Health 2014;11(Suppl 3):S3ArticlePubMedPMCPDF
- 63. Morgane PJ, Mokler DJ, Galler JR. Effects of prenatal protein malnutrition on the hippocampal formation. Neurosci Biobehav Rev 2002;26(4):471-483ArticlePubMed
- 64. Rizzo TA, Metzger BE, Dooley SL, Cho NH. Early malnutrition and child neurobehavioral development: insights from the study of children of diabetic mothers. Child Dev 1997;68(1):26-38ArticlePubMed
- 65. Wilkins E, Wickramasinghe K, Pullar J, Demaio AR, Roberts N, Perez-Blanco KM, et al. Maternal nutrition and its intergenerational links to non-communicable disease metabolic risk factors: a systematic review and narrative synthesis. J Health Popul Nutr 2021;40(1):20ArticlePubMedPMCPDF
- 66. Greco EA, Lenzi A, Migliaccio S, Gessani S. Epigenetic modifications induced by nutrients in early life phases: gender differences in metabolic alteration in adulthood. Front Genet 2019;10: 795ArticlePubMedPMC
- 67. Hardy TM, Tollefsbol TO. Epigenetic diet: impact on the epigenome and cancer. Epigenomics 2011;3(4):503-518ArticlePubMedPMC
- 68. Peral-Sanchez I, Hojeij B, Ojeda DA, Steegers-Theunissen RP, Willaime-Morawek S. Epigenetics in the uterine environment: how maternal diet and ART may influence the epigenome in the offspring with long-term health consequences. Genes (Basel) 2021;13(1):31ArticlePubMedPMC
- 69. Acevedo N, Alashkar Alhamwe B, Caraballo L, Ding M, Ferrante A, Garn H, et al. Perinatal and early-life nutrition, epigenetics, and allergy. Nutrients 2021;13(3):724ArticlePubMedPMC
- 70. World Health Organization. Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation; WHO technical report series 916. 2003 [cited 2022 Sep 22]. Available from: https://www.who.int/publications/i/item/924120916X
- 71. Keats EC, Rappaport AI, Shah S, Oh C, Jain R, Bhutta ZA. The dietary intake and practices of adolescent girls in low- and middle-income countries: a systematic review. Nutrients 2018;10(12):1978ArticlePubMedPMC
- 72. Agustina R, Nadiya K, Andini EA, Setianingsih AA, Sadariskar AA, Prafiantini E, et al. Associations of meal patterning, dietary quality and diversity with anemia and overweight-obesity among Indonesian school-going adolescent girls in West Java. PLoS One 2020;15(4):e0231519ArticlePubMedPMC
- 73. Dean S, Rudan I, Althabe F, Webb Girard A, Howson C, Langer A, et al. Setting research priorities for preconception care in low- and middle-income countries: aiming to reduce maternal and child mortality and morbidity. PLoS Med 2013;10(9):e1001508ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite



