Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 55(1); 2022 > Article
-
Original Article
Determinants of Depression in Indonesian Youth: Findings From a Community-based Survey -
Indri Yunita Suryaputri1
 , Rofingatul Mubasyiroh1
, Rofingatul Mubasyiroh1 , Sri Idaiani2
, Sri Idaiani2 , Lely Indrawati1
, Lely Indrawati1
-
Journal of Preventive Medicine and Public Health 2022;55(1):88-97.
DOI: https://doi.org/10.3961/jpmph.21.113
Published online: December 28, 2021
1Center for Research and Development of Public Health Efforts, National Institute of Health Research and Development (NIHRD), Jakarta, Indonesia
2Center for Research and Development of Health Resources and Services, National Institute of Health Research and Development, Ministry of Health, Republic Indonesia, Jakarta, Indonesia
- Corresponding author: Indri Yunita Suryaputri, Center for Research and Development of Public Health Efforts, National Institute of Health Research and Development (NIHRD), Jakarta 10560, Indonesia E-mail: indri.ysp@gmail.com
Copyright © 2022 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- This study investigated the determinants of depression in adolescents and young adults.
-
Methods
- The present study analyzed data from the 2018 Indonesia Basic Health Survey (Riset Kesehatan Dasar; RISKESDAS). The study subjects were adolescents (15-17 years old) and young adults (18-24 years old). In total, 64 179 subjects were included. Univariable, bivariable, and multivariable logistic regression analyses were performed to determine associations between youths’ characteristics, risky behavior, chronic disease, parents’ health, and youths’ depression.
-
Results
- The prevalence of depression was 5.1% in adolescents and 5.6% in young adults. The risk factors for depression in adolescents were being women (adjusted odds ratio [aOR], 3.53; 95% confidence interval [CI], 2.89 to 4.30; p<0.001), an ex-smoker (aOR, 2.99; 95% CI, 2.10 to 4.25; p<0.001), or a current smoker (aOR, 2.60; 95% CI, 1.97 to 3.44; p<0.001); consuming alcohol (aOR, 2.00; 95% CI, 1.33 to 3.01; p=0.001), having a chronic disease (aOR, 2.64; 95% CI, 1.41 to 4.96; p=0.002); maternal depression (aOR, 2.47; 95% CI, 1.97 to 3.09; p<0.001); and paternal depression (aOR, 2.63; 95% CI, 1.98 to 3.50; p<0.001). In young adults, the risk factors were being women (aOR, 2.23; 95% CI, 1.82 to 2.75; p<0.001) or an ex-smoker (aOR, 2.47; 95% CI, 1.67 to 3.67; p<0.001), consuming alcohol (aOR, 2.42; 95% CI, 1.89 to 3.09; p<0.001), maternal depression (aOR, 3.12; 95% CI, 2.54 to 3.84; p<0.001), and paternal depression (aOR, 2.80; 95% CI, 2.17 to 3.63; p<0.001).
-
Conclusions
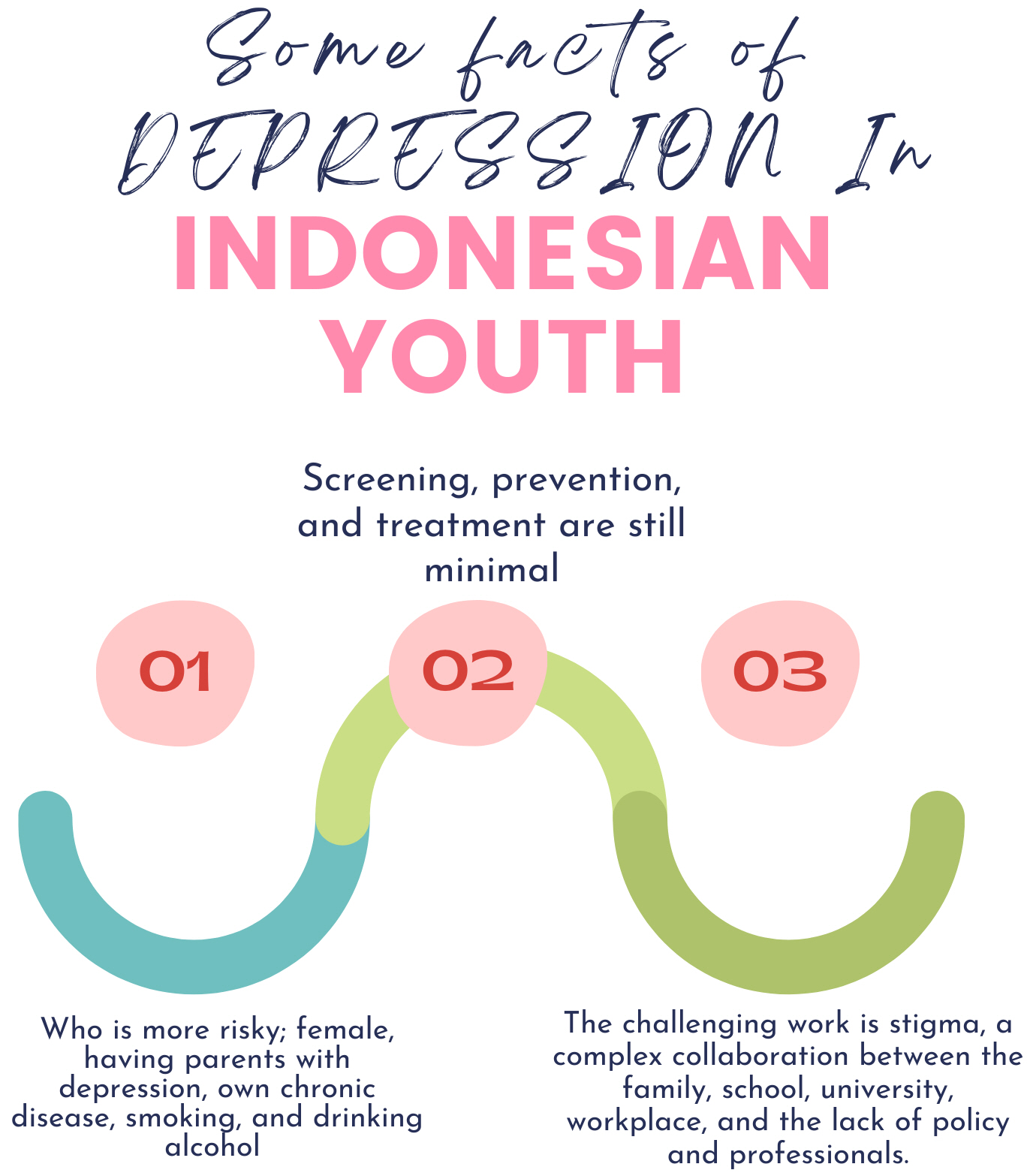
- Being women, smoking, drinking alcohol, having a chronic disease, and having a parent with depression were crucial factors associated with youth depression. Mental health screening, prevention, and treatment should involve collaboration among primary healthcare, schools, universities, professionals, and families.
- Mental health issues often emerge at a young age. Like other countries, youth mental health issues have become more prevalent in Indonesia. According to the Indonesia Basic Health Survey (Riset Kesehatan Dasar or RISKESDAS), the prevalence of depression in the 15-24-year-old population was 6.2% [1]. Another study showed that approximately 7.7% of students in Indonesia had mental/emotional problems [2]. Unfortunately, only 9.2% of youth aged 15-24 years who experienced depression accessed treatment at health facilities [3]. Therefore, it is crucial for Indonesia as a developing country to look more closely and take more action to address this problem because young people are essential for the nation’s future development.
- Depression can affect health conditions and productivity. A longitudinal study assessing depression and health conditions at the ages of 15 and 20 showed that depression was associated with low perceptions of respondents about their general health, more frequent use of health facilities, and increased work interruptions due to health conditions [4]. A meta-analysis revealed that depression in 10-19-year-olds was related to unaccomplished studies at secondary school, unemployment, low income, and loneliness in adulthood [5]. Another reason that depression is crucial is that it could lead to suicide. A study in 3 cities in Indonesia showed that people with depression were 11 times more likely to have suicidal thoughts [6].
- In Indonesia, actual data on the suicide rate do not yet exist on the national level [7]. Currently, the suicide data used in Indonesia are the World Health Organization (WHO) global health estimates, the Sample Registration System (SRS), police records, and information on the number of respondents with suicidal ideation from the Global School-based Student Health Survey (GSHS). Based on the WHO global estimates, the death rate due to suicide in Indonesia was 3.4 deaths per 100 000 population, while according to the SRS, it was 1.7 per 100 000 population, and from police records, there were 875 cases in 2016 and 789 cases in 2017 [8]. According to the GSHS, suicidal ideation and suicide attempts were reported by 4.75% and 2.46% of 13-18-year-old school-going adolescents, respectively [9].
- The government and related institutions should prioritize mental health interventions and promotional efforts in youth because the early onset of mental health issues could have effects in following years. The WHO suggests a multi-faceted approach to prevent mental illness and promote mental health [10]. One of the frameworks recommended for public mental health intervention and promotion is Bronfenbrenner’s ecological theory, according to which individual and environmental factors are related to health [11]. Bronfenbrenner’s theory views the mental health of youth in a context ranging from the individual level (age, sex, personal issues) to broader aspects of the environment (family, school, friends, work, community) and the most extensive system of norms, ideologies, and values [12].
- A qualitative study in South Sulawesi and Jakarta involving 16-18-year-old students found that parents were a crucial aspect of their mental health [13]. Studies showed that mothers with previous or current depression were risk factors for adolescent mental health [14], and paternal depression was also associated with depressive symptoms in adolescents [15]. Family conditions such as serious illnesses and depression in parents also influenced youth depression [16]. Previous studies showed that in Indonesians 15 years old and above, socio-demographic factors such as younger age, poor economic conditions, unemployment, having one or more chronic diseases, tobacco use, and soft drink consumption contributed to depression [17,18]. Other studies confirmed that lifestyle factors such as smoking and drinking alcohol were also risk factors for depression in youth [19].
- Community epidemiological data on correlates of youth depression make a fundamental contribution to policy planning for the development of effective preventive strategies, especially in Indonesia, where national data on parental and youth depression are limited. Therefore, this study aimed to identify the determinants of depression in youth, particularly in adolescents (15-17 years) and young adults (18-24 years), as a first step towards the implementation of adequate prevention, identification, and early treatment strategies for mental health issues in young persons.
INTRODUCTION
- Study Design
- The data used in this analysis were derived from the 2018 RISKESDAS. The RISKESDAS is a periodic community-based survey implemented since 2007 to collect primary data and health indicators regarding community health conditions at national, provincial, and district levels [1]. In 2018, the RISKESDAS consisted of 30 000 census blocks spread across all 34 provinces in Indonesia. The RISKESDAS study design was cross-sectional and non-interventional. Trained enumerators with at least a diploma from a health education program administered structured questionnaires to respondents.
- The subjects of the study were a sub-sample of youth (aged 15-24 years). The inclusion criteria were (1) respondents who answered depression questions themselves and could answer all the questions, and (2) youth who lived with parents. The exclusion criteria were respondents representing other family members answering the depression question. Therefore, the subjects analyzed were youth who also had complete data on their mothers and fathers. The total number of subjects aged 15-24 years was 81 836; however, all variables could only be analyzed for 64 179 respondents.
- The dependent variable in this research was youth depression. The depression variable originated from the Mini-International Neuropsychiatric Interview (MINI) translated into Bahasa [20]. The MINI is a short, structured questionnaire developed by psychiatrists and clinicians in the United States and Europe to be used for psychiatric screening. The questionnaire consists of 10 questions with “yes” or “no” answers; a sample of the questions includes: “In the past two weeks, have you been consistently sad, depressed or down, most of the day, nearly every day?”, “In the past two weeks, have you been most of the time less interested in most things or less able to enjoy the things you used to enjoy?”, and “In the past two weeks, did you feel tired or without energy, most of the time?” The respondents were categorized as having depression if they had at least 2 “yes” answers to questions 1-3 and a minimum of 2 “yes” answers to questions 4-10 [20]. The instrument also has been validated in the general population in Indonesia [21].
- The main independent variables in this study were respondents’ demographic characteristics: gender (men and women) and age (15-17 or 18-24 years old). According to developmental psychology, adolescence is divided into middle adolescence (15-17 years) and late adolescence (18 years to the mid20s) [22]. Other experts defined the age between 14-17 as adolescence and the range of 18-25 years as young adulthood due to differences in the groups based on physical, cognitive, emotional, social, sexual, moral, religious, and academic and legal capacity [23]. These age groups are also based on adolescence as a period of psychosocial development that includes increasing independence from parents and family [24]. Other variables were working status (working or not working); educational level, which corresponded to the highest degree completed with a certificate (less than high school or high school and above); marital status (unmarried or married); and area of residence (rural or urban). The socioeconomic level was determined based on the average per capita monthly income, divided into 5 quintiles, from 1 (poorest) to 5 (richest).
- Youths were categorized based on their smoking status as never smokers, ex-smokers, or current smokers. Never smokers were those who stated that they had not smoked at all in their lives, ex-smokers were those who answered that they “had quit smoking,” and current smokers were those who had smoked in the month before the interview [25]. Alcohol consumption was categorized as “no” consumption if study participants answered that they had not consumed alcohol in the month preceding the interview and as “yes” if participants had consumed alcohol in the previous month. This study also explored depression in parents as an independent variable related to youth depression. The measurement instrument used to determine youth depression was also used to assess depression in parents.
- Another independent variable was chronic disease in youth and parents, which was obtained by asking whether a medical doctor had diagnosed them with 6 chronic diseases: diabetes mellitus/diabetes, cancer, heart disease, hypertension/high blood pressure, stroke, and chronic kidney failure. The questions in this variable were “Has [NAME] been diagnosed with cancer by a doctor?”, “Has [NAME] ever been diagnosed with diabetes by a doctor?”, “Has [NAME] ever been diagnosed with heart disease by a doctor?”, “Has [NAME] been diagnosed with hypertension/high blood pressure disease by a doctor?”, “Has [NAME] ever been diagnosed with stroke by a doctor?”, “Has [NAME] been diagnosed by a doctor as suffering from chronic kidney failure (the kidney is sick for at least three consecutive months)?”. Youth and parents were classified as having a chronic disease if they answered “yes” to at least 1 question. Chronic disease history for parents was determined using the same questions as for the youth.
- Statistical Analysis
- All complete data research variables, both in youth as a whole and in specific age groups (15-17 and 18-24 years), were analyzed with descriptive, bivariate, and multivariate logistic regression models. Youth characteristics were described using descriptive statistics. The final multivariate logistic regression model carried out separately by age group was obtained by eliminating variables with large significance values that did not change the odds ratio (OR) values for other variables. All statistical analyses in this study were conducted in Stata SE version 15 (StataCorp., College Station, TX, USA).
- Ethics Statement
- The RISKESDAS 2018 study protocol was reviewed and approved by the National Ethics Commission for Health Research, National Institute of Health Research and Development (NIHRD), Ministry of Health of Indonesia (No. LB.02.01/2/KE.024/2018). In addition, respondents provided written approval for their involvement in the study. The data set used in this analysis did not contain the identities of the respondents.
METHODS
Indonesia Basic Health Survey (Riset Kesehatan Dasar or RISKESDAS)
Study subjects
Study variables
- Univariate Analysis
- The univariate analysis given in Table 1 showed that more than half of the respondents were boys (55.6%). The mean age of all respondents was 18.3 years. In total, 29.4% of the respondents were employed, more than half had less than a high school education, and only 7.9% of the respondents were married. More than half (56.7%) of youth lived in urban areas, and their families’ economic level was distributed evenly from the low to high quintiles. A quarter of the respondents smoked (26.2%), and the rate of alcohol consumption was low (4.6%). Chronic diseases affected only 0.9% of youth, while 6.5% of the respondents’ mothers had a chronic disease and 7.4% experienced depression. Furthermore, 6.1% of the respondents had fathers with chronic illnesses and 4.2% had fathers with depression.
- Depression in youth (aged 15-24 years) was more common in girls (6.8%) than in boys; this pattern was the same in the 15-17 and 18-24 age group. Young people who did not work had a higher proportion of depression (5.6%); this was also seen in the 18-24-year-old group, but it was different in the age group of 15-17 years, where almost the same values were found for did and did not work. Young people living in urban areas experienced more depression (6.1%) than those living in rural areas, with significantly higher rates in both age groups.
- Cigarette and alcohol consumption influenced the proportion of depression in youth. Ever smokers were significantly more likely to have experienced depression (8.4%) than youth who did not smoke or were current smokers; a similar pattern was found in both age groups. In addition, a significantly higher proportion of youth who consumed alcohol experienced depression (10.8%) than those who did not drink alcohol. The same pattern was found in both age groups.
- Youth who experienced chronic diseases had twice as high a proportion of depression (10.2%) than youth who did not have chronic illnesses. In particular, in adolescents 15-17 years of age, depression was also twice as common in adolescents who suffered from chronic diseases than in those with no chronic illnesses. The proportion was also higher in the older age group, but not to the same extent. Maternal and paternal physical and mental health significantly contributed to youth mental health. Chronic paternal and maternal illness, in particular, was positively associated with depression in young adults. However, this was not the case with adolescents, for whom parental chronic illness was not associated with depression. Maternal and paternal depression showed associations with youth depression, with the proportion of depression being 3 times higher in adolescents with depressed mothers or fathers.
- Multivariate Analysis
- The results of the multivariate analysis are presented in Table 2. Different factors contributed to depression in adolescents aged 15-17 years and 18-24 years. The factors with the highest ORs in adolescents were women (OR, 3.53; 95% CI, 2.89 to 4.30; p<0.001), ex-smoking status (OR, 2.99; 95% CI, 2.10 to 4.25; p<0.001), the presence of a chronic disease (OR, 2.64; 95% CI, 1.41 to 4.96; p=0.002), paternal depression (OR, 2.63; 95% CI, 1.98 to 3.50; p<0.001), current smoking (OR 2.60; 95% CI, 1.97 to 3.44; p<0.001), maternal depression (OR, 2.47; 95% CI, 1.97 to 3.09; p<0.001) and alcohol consumption (OR, 2.00; 95% CI, 1.33 to 3.01; p=0.001). In young adults, the most powerful factor influencing depression was maternal depression (OR, 3.12; 95% CI, 2.54 to 3.84; p<0.001), followed by paternal depression (OR, 2.80; 95% CI, 2.17 to 3.63; p<0.001), ex-smoking status (OR, 2.47; 95% CI, 1.67 to 3.67; p<0.001), alcohol consumption (OR, 2.42; 95% CI, 1.89 to 3.09; p<0.001), and women (OR, 2.23; 95% CI, 1.82 to 2.75; p<0.001).
RESULTS
- This study found that depression was present 5.1% of adolescents and in 5.6% of young adults. There were differences in the pattern of depression risk factors between adolescents and young adults. The risk factors for adolescent depression were gender, paternal and maternal depression, the presence of a chronic disease, smoking behavior, and alcohol consumption. Meanwhile, in young adults (18-24 years of age), the risk factors for depression were maternal and paternal depression, alcohol consumption, smoking behavior, and gender. The results of our study provide evidence that environmental and individual factors contribute to adolescent depression, as suggested by ecological theory.
- Gender
- Women were identified as an individual contributor to depression. Young women’s risk of depression was greater than that of men, whether in adolescence (OR, 3.53: 95% CI, 2.89 to 4.30; p<0.001) or in young adulthood (OR, 2.23: 95% CI, 1.82 to 2.75; p<0.001). This strengthens the findings of previous research, according to which women are more likely to have depression than men. In more detail, young adolescent girls showed more robust results than young adult women. The result is in line with a study showing that women had steeper increases in depression trajectory and an earlier peak of depressive symptoms than men, possibly because of puberty timing and status [26]. According to another study, differences in depression between genders reach their peak in adolescence [27]. As an explanation, it has been proposed that the higher likelihood of depression in girls is due to a combination of affective factors (e.g., emotional reactions to things), biological factors (e.g., genetics, hormones, and the development of puberty), cognitive factors (e.g., thinking style, awareness of judgments of other people towards themselves, and thoughts about feeling uneasy), and socio-cultural factors (including media and gender inequality) [28].
- Parental Depression
- Another vital factor that affects young people is parental depression. As mentioned before, the factor of parental history of depression (both maternal and paternal) appeared influential in youth depression in this study. Adolescents aged 15-17 years with depressed mothers had more than twice as high a risk for depression than their counterparts. Although its contribution was slightly lower than that of maternal depression, paternal depression was associated with a 2.63 times higher risk of depression in adolescents. In young adults aged 18-24 years, those who had a mother with depression were more than 3 times as likely to be depressed, and those who had a father with depression showed a slightly lower, but still substantial, risk elevation (OR, 2.80; 95% CI 2.17 to 3.63; p<0.001). Parental effects on their offspring’s psychological conditions are consistent with the findings of a previous study that parental depression increased the risk of mental disorders and depression in adolescents [29]. Depression runs in families, with a 3-fold to 4-fold increase of depression in the offspring of depressed parents [30]. In addition, poor parenting, poor communication, economic difficulties, and conflicts in depressed parents increase children’s risk of experiencing the same condition [31].
- Mothers and fathers have the opportunity to exert influence on their children when they are depressed. Specifically, maternal depression is often manifested through internalizing symptoms, such as feelings of worthlessness, which can influence other behaviors. This may explain why maternal depression significantly affected the warmth and monitoring aspects of adolescent depression. At the same time, depression in fathers often manifests in external actions (e.g., angry behavior, withdrawal, drug abuse, and acts of violence towards children). These conditions are more stressful at adolescence than in childhood because adolescents can recognize if their parents’ behavior has changed [32].
- Substance Use: Smoking and Alcohol Consumption
- Unhealthy behavior, such as smoking, also contributed to the mental health of youth in this study. Ex-smokers were more than twice as likely to have depression, and a >2-fold higher risk of depression was observed in adolescents with current smoking behavior in comparison to their non-smoking counterparts (OR, 2.60, 95% CI, 1.97 to 3.44; p<0.001). In young adults, ex-smokers were more than twice as likely to have depression than never-smokers (OR, 2.47; 95% CI, 1.67 to 3.67; p<0.001). Non-smokers and ex-smokers were at greater risk of experiencing depression than smokers, but this trend seemed more evident in ex-smokers. The findings are in line with those of another study in Indonesia, according to which youth who had quit smoking were more likely to be depressed than never-smokers [18]. Besides the significant increase in depression in current smokers, there was also a considerable escalation from non-smokers to former non-smokers [33]. Another study using National Survey on Drug Use and Health data in the United States from 2002-2016 with respondents who were former smokers showed increasing rates of depression, from 4.88% in 2005 to 6.04% in 2016 [34].
- Alcohol consumption was also found to be associated with depression. Studies have shown that alcohol consumption was associated with depression [19,35]. Another study in young people showed that weekly and excessive drinking behavior was related to depression [36]. Even light alcohol drinking has been found to be associated with depressive symptoms in youth [37].
- Physical Health: Chronic Illness
- Chronic disease in youth affects their mental health. A systematic review showed increased rates of psychiatric conditions such as depression in youth with chronic diseases, especially asthma and diabetes mellitus [38]. A qualitative study reported that chronic illness experienced by adolescents made them feel different, especially in their body and the world, and disturbed ‘normal’ life [39]. A cohort study found that activity limitation, an essential aspect in adolescents who are in the phase of achieving autonomy, developing identity, and establishing good relationships, explained the link between chronic disease and mental health [40].
- This study showed that women were associated with an increased vulnerability to depression. However, environmental factors such as parents’ psychological conditions also significantly impacted youths’ mental health. In addition, lifestyle factors such as smoking and drinking alcohol should be looked at seriously in youth because those are also associated with depression.
- In the future, the above factors are essential for policymakers, health professionals, educators, and social service providers to consider in making interventions. Screening, prevention, and treatment are necessary for mental health in youth. It is crucial to screen all adolescents and young adults for depression, especially those with risk factors and key symptoms associated with general youth functioning (e.g., in the academic, social, cognitive, and familial domains). The screening could be done in primary health care settings (in Indonesia, known as Puskesmas) that collaborate with school or university health centers. Screening in youth, particularly adolescents, must be a priority because depression often emerges at this age, and they do not readily communicate or articulate about what they feel. The other action is prevention. Strategies to prevent youth depression should recognize specific age and target groups. Mental health prevention programs should engage schools and parents since many affected individuals are of school age. Programs such as healthy schools, including developing personal skills, anti-bullying, stress management, and even parental involvement, should be encouraged. In young adults, prevention could take place in the college or workplace. Finally, in terms of depression as psychopathology, the treatment of youth depression should be incorporated with activities in school, college, or the office. Depression treatment should also consider including parents or family members since parental factors are fundamental for understanding depression in youth. In Indonesia, parents and family also play significant roles in the lives of young people.
- In Indonesia, some programs can be used to deliver services for youth mental health. Pelayanan Kesehatan Peduli Remaja (PKPR) – Youth Friendly Services must collaborate with mental health services available in primary health centers or Puskesmas to overcome young people’s problems. In school and university settings, the health unit or Upaya Kesehatan Sekolah (UKS) and primary healthcare centers in colleges should implement promotion, prevention, and curative activities for mental health in youth. The UKS and university health centers should provide counseling, training, and guidance for school and college residents. They should also detect mental health problems, intervene early when problems are detected, and refer affected individuals to health facilities. The Puskesmas should collaborate and accept references from UKS and primary health care centers at universities to further diagnose students since Puskesmas now has mental health services.
- Social media now constitutes a vital tool to promote mental health literacy and services. Social media must promote mental health and provide a broader range of mental health services through telemedicine. Family-based interventions involving parents and families are also important programs to provide better mental health in youth.
- Strengths and Limitations
- There are several limitations to our study. First, this study had a cross-sectional design that cannot explain causal relationships among the constructs. The other weakness is that the RISKESDAS was designed to represent a sample of the general population, not only youth, so there is a possibility of selection bias. Another limitation is that the variables in the study did not consider other factors contributing to youth depression, such as experiences of sadness or violence, parenting patterns, communication, and relationships with friends. Finally, our study did not analyze intercorrelations between variables, which would be valuable information.
- However, this study has some strengths, such as (1) involving a large number of nationally representative participants; (2) using specific mental health instruments to assess depression, which are rarely used but are very useful to identify mental health issues in the community setting; and (3) including youth and their biological parents who lived in the same house as participants.
- In the future, epidemiological research, such as cohort and case-control studies, are needed to expand upon these findings to identify patterns of associations and elaborate on other mediating and moderating factors in potential causal pathways between parental and individual characteristics to the onset of depression in young people. In addition, a study of mental health and related factors in young people with nationally representative participants should be considered so that Indonesia will have more accurate data on youth mental health as part of the country’s developmental capital.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Conceptualization: Suryaputri IY, Mubasyiroh R. Data curation: Idaiani S, Indrawati L. Formal analysis: Mubasyiroh R. Funding acquisition: None. Methodology: Suryaputri IY, Mubasyiroh R. Visualization: Mubasyiroh R. Writing – original draft: Suryaputri IY, Mubasyiroh R. Writing – review & editing: Suryaputri IY, Mubasyiroh R, Idaiani S, Indrawati L.
Notes
- 1. National Institute of Health Research and Development. Indonesia Basic Health Survey (RISKESDAS) 2018. Jakarta: National Institute of Health Research and Development; 2019. (Indonesian)
- 2. Suryaputri IY, Rosha BC, Sari K. Gender and other factors and risk of mental emotional problems among students in Indonesia. Health Sci J Indones 2013;4(2):98-102
- 3. Mubasyiroh R, Idaiani S, Suryaputri IY. Treatment- seeking behavior in populations with depression symptoms. Media Health Res Dev 2020;30(1):45-54. (Indonesian)
- 4. Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. J Adolesc Health 2007;41(3):256-262ArticlePubMedPMC
- 5. Clayborne ZM, Varin M, Colman I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry 2019;58(1):72-79ArticlePubMed
- 6. Mubasyiroh R, Pradono J, Nurkhotimah E, Kusumawardani N, Idaiani S. Depression as a strong prediction of suicide risk. Glob J Health Sci 2018;10(12):52-62Article
- 7. Ahmed HU, Hossain MD, Aftab A, Soron TR, Alam MT, Chowdhury MW, et al. Suicide and depression in the World Health Organization South-East Asia Region: a systematic review. WHO South East Asia J Public Health 2017;6(1):60-66Article
- 8. Ministry of Health Republic of Indonesia. Infodatin situation and suicide prevention. Jakarta: Ministry of Health Republic of Indonesia; 2019. p. 12 (Indonesian)
- 9. Putra IG, Karin PA, Ariastuti NL. Suicidal ideation and suicide attempt among Indonesian adolescent students. Int J Adolesc Med Health 2019;33(5):20190035Article
- 10. World Health Organization. Risks to mental health: an overview of vulnerabilities and risk factors. 2012 [cited 2021 Feb 1]. Available from: https://www.who.int/mental_health/mhgap/risks_to_mental_health_EN_27_08_12.pdf
- 11. Eriksson M, Ghazinour M, Hammarström A. Different uses of Bronfenbrenner’s ecological theory in public mental health research: what is their value for guiding public mental health policy and practice? Soc Theory Health 2018;16(4):414-433Article
- 12. Currie C, Morgan A. A bio-ecological framing of evidence on the determinants of adolescent mental health - a scoping review of the international Health Behaviour in School-Aged Children (HBSC) study 1983-2020. SSM Popul Health 2020;12: 100697ArticlePubMedPMC
- 13. Willenberg L, Wulan N, Medise BE, Devaera Y, Riyanti A, Ansariadi A, et al. Understanding mental health and its determinants from the perspective of adolescents: a qualitative study across diverse social settings in Indonesia. Asian J Psychiatr 2020;52: 102148ArticlePubMed
- 14. Henry LM, Steele EH, Watson KH, Bettis AH, Gruhn M, Dunbar J, et al. Stress exposure and maternal depression as risk factors for symptoms of anxiety and depression in adolescents. Child Psychiatry Hum Dev 2020;51(4):572-584ArticlePubMedPMC
- 15. Lewis G, Neary M, Polek E, Flouri E, Lewis G. The association between paternal and adolescent depressive symptoms: evidence from two population-based cohorts. Lancet Psychiatry 2017;4(12):920-926ArticlePubMed
- 16. Pederson S, Revenson TA. Parental illness, family functioning, and adolescent well-being: a family ecology framework to guide research. J Fam Psychol 2005;19(3):404-419ArticlePubMed
- 17. Peltzer K, Pengpid S. High prevalence of depressive symptoms in a national sample of adults in Indonesia: childhood adversity, sociodemographic factors and health risk behaviour. Asian J Psychiatr 2018;33: 52-59ArticlePubMed
- 18. Purborini N, Lee MB, Devi HM, Chang HJ. Associated factors of depression among young adults in Indonesia: a population-based longitudinal study. J Formos Med Assoc 2021;120(7):1434-1443ArticlePubMed
- 19. Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J Consult Clin Psychol 2008;76(2):173-183ArticlePubMedPMC
- 20. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59(Suppl 20):22-33
- 21. Idaiani S. Validity and reliability of depression, anxiety and psychosis questionnaire of mini international neuropsychiatric interview (MINI) in Indonesia. ASEAN J Psychiatr 2020;21(1
- 22. Gutgesell ME, Payne N. Issues of adolescent psychological development in the 21st century. Pediatr Rev 2004;25(3):79-85ArticlePubMed
- 23. Curtis AC. Defining adolescence. J Adolec Fam Health 2015;7(2):2
- 24. Flórez CE, Núñez J. Teenage childbearing in Latin American countries. In: Duryea S, Edwards CA, Ureta M, editors. Critical decisions at a critical age: adolescents and young adults in Latin America. Washington, DC: Inter-American Development Bank; 2003. p. 23-90
- 25. Kusumawardani N, Tarigan I, Schlotheuber A. Socioeconomic, demographic and geographic correlates of cigarette smoking among Indonesian adolescents: results from the 2013 Indonesian Basic Health Research (RISKESDAS) survey. Glob Health Action 2018;11(Suppl 1):1467605ArticlePubMedPMC
- 26. Kwong AS, Manley D, Timpson NJ, Pearson RM, Heron J, Sallis H, et al. Identifying critical points of trajectories of depressive symptoms from childhood to young adulthood. J Youth Adolesc 2019;48(4):815-827ArticlePubMedPMC
- 27. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull 2017;143(8):783-822ArticlePubMedPMC
- 28. Hyde JS, Mezulis AH. Gender differences in depression: biological, affective, cognitive, and sociocultural factors. Harv Rev Psychiatry 2020;28(1):4-13ArticlePubMed
- 29. Mars B, Collishaw S, Smith D, Thapar A, Potter R, Sellers R, et al. Offspring of parents with recurrent depression: which features of parent depression index risk for offspring psychopathology? J Affect Disord 2012;136(1-2):44-53ArticlePubMed
- 30. Maughan B, Collishaw S, Stringaris A. Depression in childhood and adolescence. J Can Acad Child Adolesc Psychiatry 2013;22(1):35-40PubMedPMC
- 31. Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. Am J Psychiatry 2006;163(6):1001-1008ArticlePubMed
- 32. Shafer K, Fielding B, Wendt D. Similarities and differences in the influence of paternal and maternal depression on adolescent well-being. Soc Work Res 2017;41(2):85-96Article
- 33. Goodwin RD, Wall MM, Garey L, Zvolensky MJ, Dierker L, Galea S, et al. Depression among current, former, and never smokers from 2005 to 2013: the hidden role of disparities in depression in the ongoing tobacco epidemic. Drug Alcohol Depend 2017;173: 191-199ArticlePubMedPMC
- 34. Cheslack-Postava K, Wall MM, Weinberger AH, Goodwin RD. Increasing depression and substance use among former smokers in the United States, 2002-2016. Am J Prev Med 2019;57(4):429-437ArticlePubMed
- 35. Michalis G, Bellos S, Politis S, Magklara K, Petrikis P, Skapinakis P. Epidemiology of alcohol use in late adolescence in Greece and comorbidity with depression and other common mental disorders. Depress Res Treat 2019;2019: 5871857ArticlePubMedPMC
- 36. Pedrelli P, Shapero B, Archibald A, Dale C. Alcohol use and depression during adolescence and young adulthood: a summary and interpretation of mixed findings. Curr Addict Rep 2016;3(1):91-97ArticlePubMedPMC
- 37. Zhang X, Huang R, Ho SY, Lo WS, Lam TH, Wang MP. Alcohol drinking, especially light drinking, and depressive symptoms in adolescents. Drug Alcohol Depend 2021;227: 108932ArticlePubMed
- 38. Brady AM, Deighton J, Stansfeld S. Psychiatric outcomes associated with chronic illness in adolescence: a systematic review. J Adolesc 2017;59: 112-123ArticlePubMed
- 39. Kirk S, Hinton D. “I’m not what I used to be”: a qualitative study exploring how young people experience being diagnosed with a chronic illness. Child Care Health Dev 2019;45(2):216-226ArticlePubMed
- 40. Adams JS, Chien AT, Wisk LE. Mental illness among youth with chronic physical conditions. Pediatrics 2019;144(1):e20181819ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Mental health issues and quality of life amongst school-based adolescents in Indonesia
Andry Juliansen, Rivaldo Steven Heriyanto, Michelle Patricia Muljono, Charista Lydia Budiputri, Yulita Delfia Sari Sagala, Gilbert Sterling Octavius
Journal of Medicine, Surgery, and Public Health.2024; 2: 100062. CrossRef - Social participation among individuals with depression is associated with the use of informal healthcare facilities: findings from the Indonesian family life survey-5
Sofa D. Alfian, Clara F. Kusuma, Imam A. Wicaksono, Irma M. Puspitasari, Martin Wawruch, Rizky Abdulah
Current Psychology.2024; 43(25): 21596. CrossRef - The Response of the Hormone Cortisol as a Biomarker of Stress and Its Influence on Blood Glucose Levels After 6 Weeks of Routine Tahajjud in Healthy Young Men
Yusni Yusni, Safrizal Rahman
Islamic Guidance and Counseling Journal.2024;[Epub] CrossRef - Barriers and facilitators to access mental health services among people with mental disorders in Indonesia: A qualitative study
Lafi Munira, Pranee Liamputtong, Pramon Viwattanakulvanid
Belitung Nursing Journal.2023; 9(2): 110. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


