Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 57(1); 2024 > Article
-
Systematic Review
Pre-exposure Prophylaxis Adherence Among Men Who Have Sex With Men: A Systematic Review and Meta-analysis -
Suchitra Hudrudchai1,2
 , Charin Suwanwong2
, Charin Suwanwong2 , Pitchada Prasittichok2
, Pitchada Prasittichok2 , Kanu Priya Mohan2
, Kanu Priya Mohan2 , Nopphadol Janeaim2
, Nopphadol Janeaim2

-
Journal of Preventive Medicine and Public Health 2024;57(1):8-17.
DOI: https://doi.org/10.3961/jpmph.23.345
Published online: December 12, 2023
- 2,601 Views
- 357 Download
1Faculty of Nursing, Rajamangala University of Technology Thanyaburi, Pathum Thani, Thailand
2Behavioral Science Research Institute, Srinakharinwirot University, Bangkok, Thailand
- Corresponding author: Nopphadol Janeaim, Behavioral Science Research Institute, Srinakharinwirot University, 114 Sukhumvit 23, Wattana, Bangkok 10110, Thailand E-mail: nopphadol.jan@g.swu.ac.th
Copyright © 2024 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives:
- The effectiveness and efficiency of pre-exposure prophylaxis (PrEP) in reducing the transmission of human immunodeficiency virus (HIV) among men who have sex with men (MSM) relies on how widely it is adopted and adhered to, particularly among high-risk groups of MSM. The meta-analysis aimed to collect and analyze existing evidence on various factors related to PrEP adherence in MSM, including demographic characteristics, sexual behaviors, substance use, and psychosocial factors.
-
Methods:
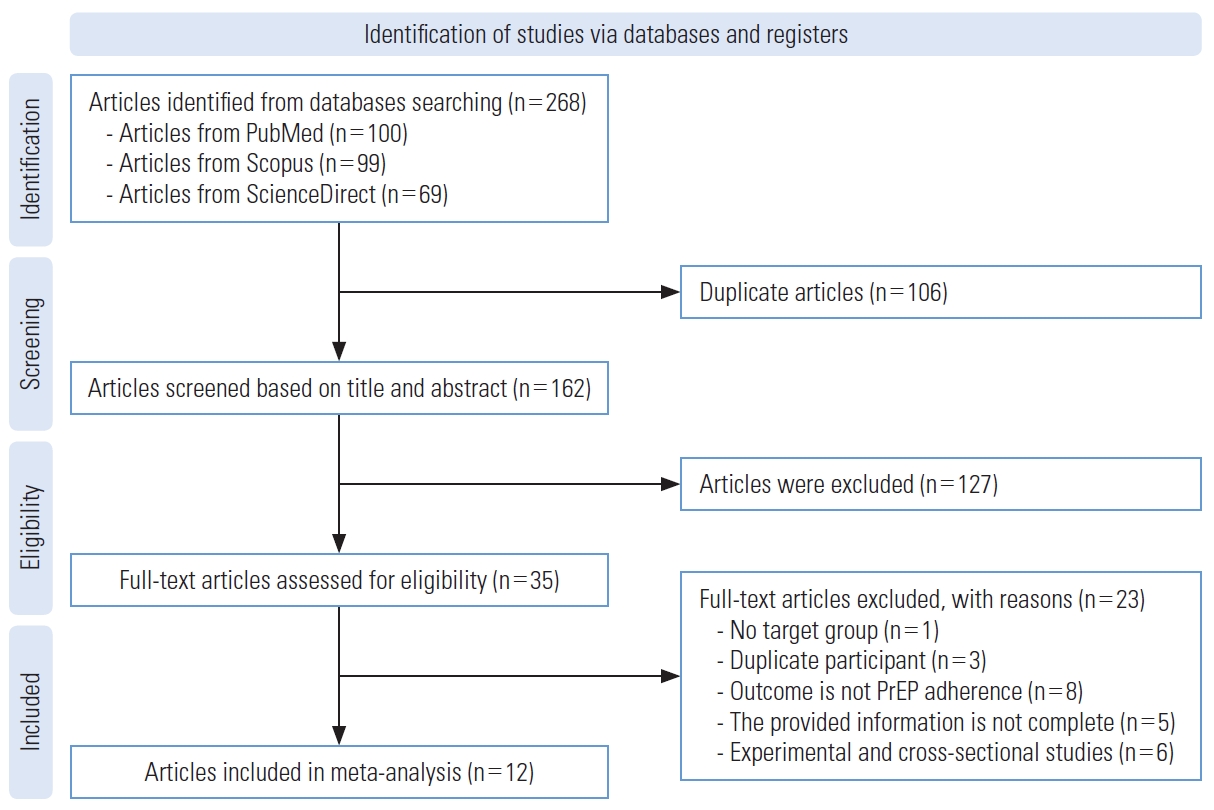
- The meta-analysis followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The search included articles published between January 2018 and December 2022, obtained from the PubMed, ScienceDirect, and Scopus databases. The studies that were included in the analysis reported the proportion of MSM who demonstrated adherence to PrEP and underwent quality appraisal using the Newcastle-Ottawa Scale.
-
Results:
- Of the 268 studies initially identified, only 12 met the inclusion criteria and were included in the final meta-analysis. The findings indicated that education (odds ratio [OR], 1.64; 95% confidence interval [CI], 1.12 to 2.40), number of sexual partners (OR, 1.16; 95% CI, 1.02 to 1.31), engaging in sexual activities with an human immunodeficiency virus-positive partner (OR, 1.59; 95% CI, 1.16 to 2.26), substance use (OR, 0.83; 95% CI, 0.70 to 0.99), and lower levels of depression (OR, 0.55; 95% CI, 0.37 to 0.82) were associated with higher rates of PrEP adherence among MSM.
-
Conclusions:
- Despite these findings, further research is necessary to investigate PrEP adherence more comprehensively. The findings of this meta-analysis can be utilized to inform interventions aimed at improving PrEP adherence among MSM and provide directions for future research in this area.
- In 2022, the World Health Organization (WHO) reported that approximately 650 000 individuals succumbed to human immunodeficiency virus (HIV)-related causes, and around 1.5 million people were newly infected with HIV. Currently, there is no cure for HIV infection [1]. The WHO has identified certain individuals who engage in high-risk behaviors as being particularly susceptible to HIV/AIDS. These behaviors include penile-anal sex, unprotected intercourse, having multiple sexual partners, and using alcohol and illicit drugs. Individuals engaging in these behaviors are categorized as key populations (KPs). Despite progress in reducing acquired immune deficiency syndrome-related mortality, the incidence of new HIV infections is on the rise, especially among KPs, which include men who have sex with men (MSM), female sex workers, and transgender women [2,3]. In 2017, the U.S. Public Health Service updated its guidelines to recommend pre-exposure prophylaxis (PrEP) for MSM who meet certain criteria. To qualify for PrEP, MSM must be at least 18 years old, HIV-negative, and have had anal intercourse in the previous 6 months. They should also not be in a mutually monogamous relationship with a recently tested HIV-negative man. Additionally, they must meet at least 1 of the following criteria: (1) having had condomless anal intercourse in the past 6 months, or (2) having been diagnosed with a bacterial sexually transmitted infection, such as gonorrhea, chlamydia, or syphilis, in the last 6 months. It is important to note that the previous indication for those in an ongoing relationship with an HIV-positive partner has been removed from the list of recommended indications [4].
- PrEP has proven to be highly effective in reducing the risk of HIV acquisition and has contributed to significant decreases in new HIV infections when integrated into a comprehensive prevention strategy [5]. For gay and bisexual men (GBM), 2 primary dosing strategies are recommended. The first is a daily regimen, which requires taking PrEP consistently every day. The second is an event-based regimen, in which PrEP is taken intermittently, specifically before and after sexual activity. This involves taking 2 doses of PrEP between 2 hours to 24 hours before sex, followed by a dose 24 hours later and another 48 hours after the initial doses. Furthermore, a thorough analysis of the data has verified that GBM who adhere to PrEP at least 4 times per week can attain a level of HIV risk reduction (96-99%) that is comparable to that of the daily or event-based regimens [6].
- The study of PrEP implementation is a complex task that requires a careful evaluation of both the usage of PrEP and individuals’ sexual activities [7]. The effectiveness and efficiency of PrEP in reducing HIV transmission among MSM is highly dependent on the adoption and adherence to PrEP by those who are at the highest risk [8]. Unfortunately, PrEP adherence rates are frequently suboptimal, resulting in improper usage due to factors such as forgetting to take the medicine, being too busy, or concerns about potential side effects [9]. However, there may be additional factors that influence PrEP adherence among MSM. Currently, there is a lack of comprehensive systematic reviews that synthesize existing knowledge regarding demographic characteristics, sexual behaviors, substance use, and psychosocial factors associated with PrEP adherence specifically among MSM. Therefore, the objective of this systematic review and meta-analysis was to identify factors that are linked to PrEP adherence among MSM. These factors include demographic characteristics, sexual behaviors, substance use, and psychosocial factors that influence the adherence to PrEP among MSM.
INTRODUCTION
- Search Strategy and Data Sources
- Our systematic review was conducted and reported following the guidelines outlined in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) framework [10]. In order to obtain a comprehensive range of relevant literature, 3 databases were utilized: PubMed, Scopus, and ScienceDirect. These databases were chosen because they cover a wide array of disciplines, including medicine, nursing, health professions, psychology, and sociology. The search strategy utilized a combination of PICO (population, intervention, comparison, outcome) terms to target specific aspects of the study. The population term focused on MSM, while the intervention term included relevant factors. The comparison term was not applicable in this case, and the outcome term focused on PrEP adherence. Various combinations of terms, along with the utilization of headings (MeSH [Medical Subject Headings]), keywords, and phrases, were employed to ensure a comprehensive search. The search was conducted in January 2023.
- Eligibility Criteria and Study Selection
- We initially screened the titles and abstracts to determine the eligibility of studies for inclusion in the meta-analysis. Specifically, we sought studies that reported on the adherence of MSM to PrEP. To meet the inclusion criteria for the meta-analysis, studies were required to meet the following criteria: (1) focus on MSM as the target population, (2) assess the behavior of PrEP adherence using methods such as self-reporting or laboratory testing, (3) provide sufficient data on factors correlated with PrEP adherence, (4) be fully published in peer-reviewed journals, (5) employ a cohort study design, (6) be published in English between January 2018 and December 2022, and (7) provide an odds ratio (OR) estimate. We excluded experimental studies, cross-sectional studies, systematic reviews, and meta-analyses from our analysis. The articles were subjected to a review by 2 reviewers to establish eligibility, and any discrepancies were resolved through team discussion.
- Data Extraction and Quality Assessment
- Two authors independently extracted data from each included study, including information on the first authors’ names, publication years, study locations, samples, types of PrEP utilized, and the quality assessment. Any disagreements were resolved through team discussion. The methodological quality of the studies was evaluated using the Newcastle-Ottawa Scale (NOS) [11]. This tool can be used either as a checklist or a scale. A separate NOS scale was developed for cohort studies. The NOS contains 8 items, categorized into 3 dimensions: selection, comparability, and depending on the study type, the outcome. For each item, a series of response options is provided. A star system is used to allow a semi-quantitative assessment of study quality. The NOS ranges between 0 stars and 9 stars. The scores are categorized as good (7-9 stars and all 3 domains complete), fair (4-6 stars and all domains complete), or poor (0-3 stars or not all domains evaluated).
- Statistical Analysis
- We examined the associations of demographic characteristics, sexual behaviors, substance use, and psychosocial factors with PrEP adherence by calculating ORs with 95% confidence intervals (CIs). In the meta-analysis, we employed either fixed-effects or random-effects models to estimate the OR with 95% CIs, and we utilized the I2 statistic to assess heterogeneity across the included studies [12]. If the I2 statistic indicated significant heterogeneity, we opted for a random-effects model. In cases where there was no significant heterogeneity, we utilized a fixed-effects model. To explore potential sources of heterogeneity, a subgroup meta-analysis was performed to assess differences according to study location. Finally, the Egger test was adopted to evaluate publication bias. All statistical analyses were performed using Stata version 17 (StataCorp., College Station, TX, USA).
- Ethics Statement
- As the current investigation involved a systematic review and meta-analysis, the data extraction was conducted exclusively from published articles.
- Consequently, there was no need for institutional review board approval.
METHODS
- Included Studies and Their Characteristics
- In this systematic review, we initially identified 268 articles through database searches. Upon assessing the eligibility of 35 full-text articles, we ultimately included 12 studies in both the systematic review and meta-analysis, as depicted in Figure 1. Table 1 [13-24] provides a summary of the characteristics of these studies. The selected studies, published between 2018 and 2022, collectively involved 5578 participants. All studies employed a cohort study design. Five were conducted in Eastern countries and 7 in Western countries. The participants’ ages ranged from 18 years to 65 years, with a mean age of 25.2 years. Based on the NOS, 5 studies were rated as good quality, while the remaining 7 were considered to have fair quality.
- Demographic Characteristics
- As presented in Table 2, the pooled effect results demonstrated a significant association between education and PrEP adherence (OR, 1.64; 95% CI, 1.12 to 2.40; p = 0.012; I2 = 73.9%). However, no significant associations were found between PrEP adherence and the following factors: age <25 years (OR, 1.01; 95% CI, 0.43 to 2.41; p = 0.979; I2 = 76.6%), age >25 years (OR, 1.01; 95% CI, 0.78 to 1.32; p = 0.106; I2 = 75.5%), and financial situation (OR, 1.78; 95% CI, 0.91 to 3.49; p <0.05; I2 = 92.8%) (Supplemental Material 1).
- Sexual Behaviors
- As shown in Table 2, the pooled effect results demonstrated a significant association between PrEP adherence and the number of partners (OR, 1.16; 95% CI, 1.02 to 1.31; p <0.05; I2 = 38.5%), as well as having sexual encounters with an HIV-positive partner (OR, 1.59; 95% CI, 1.11 to 2.26; p<0.05; I2 =0.0%). However, there were no significant associations found between PrEP adherence and the following factors: having regular partners (OR, 0.74; 95% CI, 0.42 to 1.30; p = 0.301; I2 = 76.8%), engaging with casual partners (OR, 1.10; 95% CI, 0.92 to 1.30; p = 0.287; I2 = 0.0%), having sexually transmitted infections (OR, 0.92; 95% CI, 0.68 to 1.23; p = 0.564; I2 = 0.0%), and condom use (OR, 1.02; 95% CI, 0.78 to 1.33; p = 0.912; I2 = 53.8%) (Supplemental Materials 2 and 3).
- Substance Use
- As shown in Table 2, the pooled effect results demonstrated a significant association between substance use and PrEP adherence (OR, 0.83; 95% CI, 0.70 to 0.99; p = 0.037; I2 = 46.1%) (Supplemental Material 4).
- Psychosocial Factors
- As shown in Table 2, the pooled effect results indicated a significant association between depression and PrEP adherence (OR, 0.55; 95% CI, 0.37 to 0.82; p<0.01; I2 = 18.9%). However, there was no significant association between perception of HIV prevention and PrEP adherence (OR, 0.96; 95% CI, 0.88 to 1.06; p = 0.457; I2 = 79.0%) (Supplemental Material 5).
- Subgroup Analysis
- Age >25 years, education, financial situation, having a regular partner, and perception of HIV prevention showed a high degree of heterogeneity (I2>50%). To investigate the sources of this heterogeneity, we performed a meta-regression analysis. The study location explained a significant amount of variance in the effects of these factors on PrEP adherence. Subsequently, we conducted a subgroup analysis based on study location (Table 3). The results from this analysis revealed that in the Eastern population, education (OR, 1.79; 95% CI, 1.20 to 2.66; p<0.01; I2 = 75.1%) and perception of HIV prevention (OR, 0.75; 95% CI, 0.65 to 0.87; p<0.001; I2 = 0.0%) was associated with PrEP adherence. In contrast, in the Western population, financial situation showed an association with PrEP adherence (OR, 2.34; 95% CI, 1.25 to 4.38; p<0.01; I2 = 82.7%).
- Publication Bias
- The findings from the Egger test (age >25, p = 0.619; education, p=0.377; financial situation, p=0.601; number of partners, p = 0.076; having a regular partner, p = 0.769; condom use, p = 0.476; sexually transmitted infections, p = 0.574; depression, p = 0.468; perception of HIV prevention, p = 0.649; substance use, p = 0.550) suggest that statistical methods may not effectively identify publication bias due to the limited number of studies, particularly in relation to age <25, casual partners, and sex with HIV-positive partners.
RESULTS
- This systematic review and meta-analysis investigated factors affecting PrEP adherence among MSM. The analysis of 12 included studies revealed that 1 demographic characteristic (education) and 2 sexual behaviors (number of partners and sex with HIV-positive partners), along with 1 psychosocial factor (depression), were associated with PrEP adherence among MSM. Conversely, age, financial situation, having regular partners, having casual partners, experiencing sexually transmitted infections, condom use, perception of HIV prevention, and substance use demonstrated no significant relationships with PrEP adherence. A subgroup analysis based on study location indicated that education and perception of HIV prevention were associated with PrEP adherence in the Eastern population, while financial situation was linked to PrEP adherence in the Western population. Additionally, based on the Egger test, there was no evidence of publication bias in the included studies.
- Educational attainment was found to be associated with PrEP adherence among MSM, consistent with several previous studies [15,21]. These studies consistently reported a positive relationship between higher education levels and improved PrEP adherence. Conversely, some studies indicated that individuals with lower education levels, including those with limited HIV knowledge, exhibited poorer PrEP adherence [17,25]. These findings underscore the potential impact of education on PrEP adherence and emphasize the importance of considering individuals’ educational backgrounds and HIV knowledge in understanding adherence behaviors. These results highlight the significant role of education in shaping attitudes and behaviors related to PrEP among MSM. Therefore, interventions aimed at improving PrEP adherence should consider the educational context and target programs to address specific knowledge gaps, thereby improving adherence outcomes across diverse populations.
- Sexual behaviors, including the number of partners and engaging in sexual encounters with an HIV-positive partner, have been linked to PrEP adherence among MSM. Consistent with previous studies, the number of partners was significantly associated with PrEP adherence among MSM [14,20]. This suggests that those with multiple sexual partners tend to demonstrate better adherence to PrEP. The positive correlation may indicate that individuals who engage in higher-risk sexual activities recognize the value of PrEP in mitigating their risk of HIV transmission, which in turn leads to more consistent use of the prophylactic treatment. Additionally, this observation is consistent with earlier studies that advocate for the use of PrEP among HIV serodiscordant couples [26,27], underscoring that individuals with HIV-positive partners are more likely to maintain PrEP adherence. These insights underscore the necessity of taking into account individual sexual behaviors and partner dynamics when promoting PrEP adherence. The relationships between the number of partners and encounters with HIV-positive partners call for targeted interventions and personalized counseling for those who partake in higher-risk sexual activities. Healthcare providers must cater to the unique needs of these individuals by offering the requisite support, education, and information to optimize PrEP adherence and minimize the risk of HIV transmission.
- Substance use was found to be associated with lower PrEP adherence among MSM, which aligns with the results of several previous studies [21,28]. This suggests that individuals who engage in substance use are less likely to adhere to their PrEP regimens effectively. The negative association between substance use and PrEP adherence raises concerns about the potential impact of substance use on HIV prevention efforts. Substance use may lead to decreased motivation, impaired decision-making, and increased forgetfulness [29,30], hindering individuals’ ability to consistently adhere to PrEP [31]. Moreover, substance use may also be linked to risky sexual behaviors, which could further increase the risk of HIV transmission among this population. However, it is worth noting that some studies [19,20] have reported no significant association between substance use and PrEP adherence. This contrasting finding suggests that the relationship between substance use and PrEP adherence may not be universally consistent across all populations or settings. Factors such as variations in substance use patterns, cultural norms, and access to healthcare services may contribute to these discrepancies [28,32,33]. These conflicting results highlight the complexity of the relationship between substance use and PrEP adherence. It is essential to consider these factors when interpreting the findings and developing interventions to improve PrEP adherence among MSM. Substance use should be approached with sensitivity and understanding, recognizing that addressing substance use issues may be crucial in promoting optimal PrEP adherence.
- Psychosocial factors, such as depression, were found to be associated with PrEP adherence among MSM. Consistent with previous studies, the presence of depressive symptoms was negatively associated with PrEP adherence [34,35]. This finding suggests that individuals experiencing depression are less likely to adhere to PrEP regimens effectively. The negative association implies that individuals with depression may face unique challenges or barriers that hinder their ability to consistently adhere to PrEP. Depression can impact one’s motivation, self-care practices, and overall mental well-being [36,37], subsequently affecting adherence behaviors. These findings emphasize the importance of addressing mental health concerns in the context of HIV prevention and care. Healthcare providers and support services should recognize the potential impact of depression on PrEP adherence and tailor interventions accordingly. Integrating mental health support and counseling as part of PrEP programs may prove beneficial in improving adherence outcomes among individuals with depression.
- The findings from the subgroup analysis based on study location revealed that different factors were associated with PrEP adherence in Eastern and Western populations. In the Eastern population, 2 factors were found to be associated with PrEP adherence: education and perception of HIV prevention. The pooled effect for education indicates that individuals with higher levels of education in this region were more likely to adhere to PrEP. This finding aligns with previous studies [17,20,24] that have reported a positive association between education and PrEP adherence, suggesting that better-educated individuals may have a greater understanding of the benefits and importance of PrEP in preventing HIV transmission. In contrast, the perception of HIV prevention was negatively associated with PrEP adherence in the Eastern population. This finding—namely, that individuals with a more positive perception of HIV prevention measures, including PrEP, were less likely to adhere to the medication—may seem counterintuitive and requires careful consideration. A possible explanation for this observation could be that individuals who perceive themselves to be at low risk of acquiring HIV may believe that they do not need to adhere to PrEP as rigorously [38,39]. They may feel confident in their ability to avoid HIV transmission through preventive methods, leading to lower adherence to PrEP. In the Western population, the financial situation was significantly associated with PrEP adherence. This indicates that individuals with better financial circumstances in this region were more likely to adhere to PrEP. Financial barriers may influence access to healthcare and preventive services, including PrEP [13,40]. Therefore, individuals with better financial situations may find it easier to access and afford PrEP medication, leading to higher adherence rates. The differences in the factors associated with PrEP adherence between the Eastern and Western populations highlight the importance of considering regional contexts and cultural factors in HIV prevention efforts. Tailoring interventions to address the specific needs and challenges faced by different populations can enhance PrEP uptake and adherence.
- The study had several limitations. First, it relied on data from only 3 databases, which, although covering a broad range of disciplines, might not have included all relevant studies on the subject. To enhance the comprehensiveness of the literature review and reduce potential bias, future research could broaden the search by incorporating additional databases like Embase, CINAHL, and regional databases. Second, certain factors showed high heterogeneity, which could impact the robustness and generalizability of the meta-analysis findings. For improved insights, future studies could conduct sensitivity and subgroup analyses considering various factors, such as study design, participant demographics, and healthcare settings, to explore their contributions to heterogeneity. Third, the study primarily included research from Eastern and Western countries, potentially limiting the generalizability of the findings to the global MSM population. Future research should incorporate studies from diverse regions, including low- and middle-income countries, to gain a more comprehensive understanding of the factors influencing PrEP adherence across varied cultural contexts and healthcare systems. Finally, the nature of prospective cohort studies among the included studies may be susceptible to loss to follow-up. Cross-sectional studies are better suited to determining prevalence (i.e., the number of cases in a population at a given point in time) and are useful for identifying associations with factors related to PrEP adherence.
DISCUSSION
- This systematic review and meta-analysis aimed to uncover the factors influencing PrEP adherence in MSM. The study identified several potential factors associated with PrEP adherence among MSM, including education level, the number of sexual partners, engaging in sexual encounters with HIV-positive partners, substance use, and experiencing depression. The findings offer valuable insights into the factors affecting PrEP adherence in this population, emphasizing the importance of personalized interventions to address unique challenges and enhance PrEP adherence across diverse populations. Understanding these factors is essential in developing effective strategies to prevent HIV transmission and improve the overall health outcomes of MSM.
CONCLUSION
Supplemental Materials
Supplementary Figure 1.
Supplementary Figure 2.
Supplementary Figure 3.
Supplementary Figure 4.
Supplementary Figure 5.
-
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
-
Funding
None.
-
Author Contributions
Conceptualization: Hudrudchai S. Data curation: Hudrudchai S, Suwanwong C. Formal analysis: Hudrudchai S, Suwanwong C. Funding acquisition: None. Methodology: Hudrudchai S, Suwanwong C, Prasittichok P. Project administration: Janeaim N, Hudrudchai S. Visualization: Hudrudchai S, Suwanwong C, Prasittichok P, Mohan KP, Janeaim N. Writing - original draft: Hudrudchai S, Suwanwong C, Prasittichok P, Mohan KP. Writing - review & editing: Hudrudchai S, Suwanwong C, Prasittichok P, Mohan KP, Janeaim N.
Notes
Acknowledgements
| Study | Country | Sample (n; age; median age) | Type of PrEP | Outcome measure | Quality rating |
|---|---|---|---|---|---|
| Eubanks et al. (2022) [13] | West Africa | n = 520 MSM; age ≥18 y; median age 25.6 y | Daily tablet | Self-report | Good |
| TDF/FTC and ED | |||||
| Gao et al. (2022) [14] | China | n = 791 MSM; aged 16-65 y; median age 30 y | Daily tablet | Self-report | Fair |
| TDF/FTC and ED | |||||
| Grinsztejn et al. (2018) [15] | Brazil | n = 354 MSM; ages ≥18 y | Daily tablet | Self-report, Laboratory test | Fair |
| TDF/FTC | |||||
| Hojilla et al. (2018) [16] | USA | n = 330 MSM; at least 18 y age; median age 29 y | Tablet TFV-DP | Laboratory test | Fair |
| Liu et al. (2021) [17] | China | n = 496 MSM; ages 18-65 y; median age 28 y | Daily tablet | Self-report | Good |
| TDF and on-demand | |||||
| Monteiro Spindola Marins et al. (2021) [18] | Brazil | n = 338 MSM and TGW; age ≥18 y; median age 30 y | Daily tablet | Self-report | Fair |
| TDF/FTC | |||||
| Okafor et al. (2020) [19] | USA | n = 226 Black MSM; age ≥18 y; median age 25 y | Daily tablet | Laboratory test | Good |
| TDF/FTC | |||||
| Seekaew et al. (2019) [20] | Thailand | n = 564 MSM; ages ≥18 y; median age 28.9 y | Daily tablet | Self-report | Fair |
| TDF/FTC | |||||
| Wang et al. (2020) [21] | China | n = 1023 MSM; aged 18-65 y; median age 29 y | Daily tablet | Self-report | Fair |
| TDF/FTC and ED | |||||
| Wheeler et al. (2019) [22] | USA | n = 226 Black MSM; ages ≥18 y; median age 26 y | Daily tablet | Laboratory test | Good |
| FTC/TDF | |||||
| TFV-DP | |||||
| Whitfield et al. (2021) [23] | USA | n = 226 Black MSM; ages ≥25 y; median age 26 y | Daily tablet | Laboratory test | Fair |
| FTC/TP, TFV-DP | |||||
| Wu et al. (2021) [24] | Taiwan | n = 374 MSM; ages ≥18 y | Daily tablet | Self-report | Good |
| TDF/FTC and ED |
- 1. World Health Organization. HIV and AIDS; 2018 [cited 2023 Jun 15]. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids
- 2. Ochonye B, Folayan MO, Fatusi AO, Bello BM, Ajidagba B, Emmanuel G, et al. Sexual practices, sexual behavior and HIV risk profile of key populations in Nigeria. BMC Public Health 2019;19(1):1210. https://doi.org/10.1186/s12889-019-7553-zArticlePubMedPMC
- 3. Risher K, Mayer KH, Beyrer C. HIV treatment cascade in MSM, people who inject drugs, and sex workers. Curr Opin HIV AIDS 2015;10(6):420-429. https://doi.org/10.1097/COH.0000000000000200ArticlePubMedPMC
- 4. Centers for Disease Control and Prevention, US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline; 2018 [cited 2023 Jul 14]. Available from: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf
- 5. Grulich AE, Guy R, Amin J, Jin F, Selvey C, Holden J, et al. Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW prospective cohort study. Lancet HIV 2018;5(11):e629-e637. https://doi.org/10.1016/S2352-3018(18)30215-7ArticlePubMed
- 6. Buchbinder SP. Maximizing the benefits of HIV preexposure prophylaxis. Top Antivir Med 2018;25(4):138-142PubMedPMC
- 7. Gillespie D, Couzens Z, de Bruin M, Hughes DA, Jones A, Ma R, et al. PrEP use, sexual behaviour, and PrEP adherence among men who have sex with men living in Wales prior to and during the COVID-19 pandemic. AIDS Behav 2022;26(8):2746-2757. https://doi.org/10.1007/s10461-022-03618-4ArticlePubMedPMC
- 8. Vuylsteke B, Reyniers T, De Baetselier I, Nöstlinger C, Crucitti T, Buyze J, et al. Daily and event-driven pre-exposure prophylaxis for men who have sex with men in Belgium: results of a prospective cohort measuring adherence, sexual behaviour and STI incidence. J Int AIDS Soc 2019;22(10):e25407. https://doi.org/10.1002/jia2.25407ArticlePubMedPMC
- 9. Qu D, Zhong X, Xiao G, Dai J, Liang H, Huang A. Adherence to pre-exposure prophylaxis among men who have sex with men: a prospective cohort study. Int J Infect Dis 2018;75: 52-59. https://doi.org/10.1016/j.ijid.2018.08.006ArticlePubMed
- 10. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88: 105906. https://doi.org/10.1016/j.ijsu.2021.105906ArticlePubMed
- 11. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25(9):603-605. https://doi.org/10.1007/s10654-010-9491-zArticlePubMed
- 12. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-560. https://doi.org/10.1136/bmj.327.7414.557ArticlePubMedPMC
- 13. Eubanks A, Coulibaly B, Dembélé Keita B, Anoma C, Dah TT, Mensah E, et al. Socio-behavioral correlates of pre-exposure prophylaxis use and correct adherence in men who have sex with men in West Africa. BMC Public Health 2022;22(1):1832. https://doi.org/10.1186/s12889-022-14211-8ArticlePubMedPMC
- 14. Gao Y, Hu Q, Leuba SI, Jia L, Wang H, Huang X, et al. Medication non-adherence and condomless anal intercourse increased substantially during the COVID-19 pandemic among MSM PrEP users: a retrospective cohort study in four Chinese metropolises. Front Med (Lausanne) 2022;9: 738541. https://doi.org/10.3389/fmed.2022.738541ArticlePubMedPMC
- 15. Grinsztejn B, Hoagland B, Moreira RI, Kallas EG, Madruga JV, Goulart S, et al. Retention, engagement, and adherence to pre-exposure prophylaxis for men who have sex with men and transgender women in PrEP Brasil: 48 week results of a demonstration study. Lancet HIV 2018;5(3):e136-e145. https://doi.org/10.1016/S2352-3018(18)30008-0ArticlePubMed
- 16. Hojilla JC, Vlahov D, Glidden DV, Amico KR, Mehrotra M, Hance R, et al. Skating on thin ice: stimulant use and sub-optimal adherence to HIV pre-exposure prophylaxis. J Int AIDS Soc 2018;21(3):e25103. https://doi.org/10.1002/jia2.25103ArticlePubMedPMC
- 17. Liu J, Deng R, Lin B, Pan H, Gao Y, Dai J, et al. Risk management on pre-exposure prophylaxis adherence of men who have sex with multiple men: a multicenter prospective cohort study. Risk Manag Healthc Policy 2021;14: 1749-1761. https://doi.org/10.2147/RMHP.S295114ArticlePubMedPMC
- 18. Monteiro Spindola Marins L, Silva Torres T, Luz PM, Moreira RI, Leite IC, Hoagland B, et al. Factors associated with self-reported adherence to daily oral pre-exposure prophylaxis among men who have sex with man and transgender women: PrEP Brasil study. Int J STD AIDS 2021;32(13):1231-1241. https://doi.org/10.1177/09564624211031787ArticlePubMed
- 19. Okafor CN, Hucks-Ortiz C, Hightow-Weidman LB, Magnus M, Emel L, Beauchamp G, et al. Brief report: associations between self-reported substance use behaviors and PrEP acceptance and adherence among black MSM in the HPTN 073 study. J Acquir Immune Defic Syndr 2020;85(1):23-29. https://doi.org/10.1097/QAI.0000000000002407ArticlePubMedPMC
- 20. Seekaew P, Nguyen E, Sungsing T, Jantarapakde J, Pengnonyang S, Trachunthong D, et al. Correlates of nonadherence to key population-led HIV pre-exposure prophylaxis services among Thai men who have sex with men and transgender women. BMC Public Health 2019;19(1):328. https://doi.org/10.1186/s12889-019-6645-0ArticlePubMedPMC
- 21. Wang H, Zhang J, Chu Z, Hu Q, Dong W, Huang X, et al. Risk-taking behaviors and adherence to HIV pre-exposure prophylaxis in users of geosocial networking apps: real-world, multicenter study. J Med Internet Res 2020;22(10):e22388. https://doi.org/10.2196/22388ArticlePubMedPMC
- 22. Wheeler DP, Fields SD, Beauchamp G, Chen YQ, Emel LM, Hightow-Weidman L, et al. Pre-exposure prophylaxis initiation and adherence among Black men who have sex with men (MSM) in three US cities: results from the HPTN 073 study. J Int AIDS Soc 2019;22(2):e25223. https://doi.org/10.1002/jia2.25223ArticlePubMedPMC
- 23. Whitfield DL, Beauchamp G, Fields S, Nelson L, Magnus M, Dācus JD, et al. Risk compensation in HIV PrEP adherence among Black men who have sex with men in HPTN 073 study. AIDS Care 2021;33(5):633-638. https://doi.org/10.1080/09540121.2020.1810618ArticlePubMed
- 24. Wu HJ, Wen-Wei Ku S, Chang HH, Li CW, Ko NY, Strong C. Imperfect adherence in real life: a prevention-effective perspective on adherence to daily and event-driven HIV pre-exposure prophylaxis among men who have sex with men - a prospective cohort study in Taiwan. J Int AIDS Soc 2021;24(5):e25733. https://doi.org/10.1002/jia2.25733ArticlePubMedPMC
- 25. Aderemi-Williams RI, Razaq AR, Abah IO, Opanuga OO, Akanmu AS. Adolescents and young adults knowledge, adherence and experiences while on antiretroviral therapy in a tertiary hospital in Lagos, Nigeria: a mixed-method study. J Int Assoc Provid AIDS Care 2021;20: 23259582211062754. https://doi.org/10.1177/23259582211062754ArticlePubMedPMC
- 26. Musinguzi N, Kidoguchi L, Mugo NR, Ngure K, Katabira E, Celum CL, et al. Adherence to recommendations for ART and targeted PrEP use among HIV serodiscordant couples in East Africa: the “PrEP as a bridge to ART” strategy. BMC Public Health 2020;20(1):1621. https://doi.org/10.1186/s12889-020-09712-3ArticlePubMedPMC
- 27. Sack DE, De Schacht C, Paulo P, Graves E, Emílio AM, Matino A, et al. Pre-exposure prophylaxis use among HIV serodiscordant couples: a qualitative study in Mozambique. Glob Health Action 2021;14(1):1940764. https://doi.org/10.1080/16549716.2021.1940764ArticlePubMedPMC
- 28. Gebru NM, Canidate SS, Liu Y, Schaefer SE, Pavila E, Cook RL, et al. Substance use and adherence to HIV pre-exposure prophylaxis in studies enrolling men who have sex with men and transgender women: a systematic review. AIDS Behav 2023;27(7):2131-2162. https://doi.org/10.1007/s10461-022-03948-3ArticlePubMed
- 29. Smith R, Schwartenbeck P, Stewart JL, Kuplicki R, Ekhtiari H, Paulus MP, et al. Imprecise action selection in substance use disorder: evidence for active learning impairments when solving the explore-exploit dilemma. Drug Alcohol Depend 2020;215: 108208. https://doi.org/10.1016/j.drugalcdep.2020.108208ArticlePubMedPMC
- 30. Pasipanodya EC, Li MJ, Jain S, Sun X, Tobin J, Ellorin E, et al. Greater levels of self-reported adherence to pre-exposure prophylaxis (PrEP) are associated with increased condomless sex among men who have sex with men. AIDS Behav 2020;24(11):3192-3204. https://doi.org/10.1007/s10461-020-02881-7ArticlePubMedPMC
- 31. Viamonte M, Ghanooni D, Reynolds JM, Grov C, Carrico AW. Running with scissors: a systematic review of substance use and the pre-exposure prophylaxis care continuum among sexual minority men. Curr HIV/AIDS Rep 2022;19(4):235-250. https://doi.org/10.1007/s11904-022-00608-yArticlePubMedPMC
- 32. Hillis A, Germain J, Hope V, McVeigh J, Van Hout MC. Pre-exposure prophylaxis (PrEP) for HIV prevention among men who have sex with men (MSM): a scoping review on PrEP service delivery and programming. AIDS Behav 2020;24(11):3056-3070. https://doi.org/10.1007/s10461-020-02855-9ArticlePubMedPMC
- 33. Westmoreland DA, Patel VV, D’Angelo AB, Nash D, Grov C. Sociocultural influences on attitudes towards pre-exposure prophylaxis (PrEP), history of PrEP use, and future PrEP use in HIV-vulnerable cisgender men who have sex with men across the U.S. Ann LGBTQ Public Popul Health 2020;1(2):128-158. https://doi.org/10.1891/lgbtq-2020-0005ArticlePubMedPMC
- 34. Shuper PA, Joharchi N, Bogoch II, Loutfy M, Crouzat F, El-Helou P, et al. Alcohol consumption, substance use, and depression in relation to HIV pre-exposure prophylaxis (PrEP) nonadherence among gay, bisexual, and other men-who-have-sex-with-men. BMC Public Health 2020;20(1):1782. https://doi.org/10.1186/s12889-020-09883-zArticlePubMedPMC
- 35. Colson PW, Franks J, Wu Y, Winterhalter FS, Knox J, Ortega H, et al. Adherence to pre-exposure prophylaxis in black men who have sex with men and transgender women in a community setting in Harlem, NY. AIDS Behav 2020;24(12):3436-3455. https://doi.org/10.1007/s10461-020-02901-6ArticlePubMed
- 36. Velloza J, Baeten JM, Haberer J, Ngure K, Irungu E, Mugo NR, et al. Effect of depression on adherence to oral PrEP among men and women in East Africa. J Acquir Immune Defic Syndr 2018;79(3):330-338. https://doi.org/10.1097/QAI.0000000000001821ArticlePubMedPMC
- 37. Velloza J, Heffron R, Amico KR, Rowhani-Rahbar A, Hughes JP, Li M, et al. The effect of depression on adherence to HIV pre-exposure prophylaxis among high-risk South African women in HPTN 067/ADAPT. AIDS Behav 2020;24(7):2178-2187. https://doi.org/10.1007/s10461-020-02783-8ArticlePubMedPMC
- 38. Peng L, Cao W, Gu J, Hao C, Li J, Wei D, et al. Willingness to use and adhere to HIV pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in China. Int J Environ Res Public Health 2019;16(14):2620. https://doi.org/10.3390/ijerph 6142620ArticlePubMedPMC
- 39. Soares F, Magno L, da Silva LA, Guimarães MD, Leal AF, Knauth D, et al. Perceived risk of HIV infection and acceptability of PrEP among men who have sex with men in Brazil. Arch Sex Behav 2023;52(2):773-782. https://doi.org/10.1007/s10508-022-02342-3ArticlePubMed
- 40. Mayer KH, Agwu A, Malebranche D. Barriers to the wider use of pre-exposure prophylaxis in the United States: a narrative review. Adv Ther 2020;37(5):1778-1811. https://doi.org/10.1007/s12325-020-01295-0ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


