Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(5); 2023 > Article
-
Original Article
Health-related Quality of Life of Patients With Diabetes Mellitus Measured With the Bahasa Indonesia Version of EQ-5D in Primary Care Settings in Indonesia -
Muhammad Husen Prabowo1
 , Ratih Puspita Febrinasari2
, Ratih Puspita Febrinasari2 , Eti Poncorini Pamungkasari3
, Eti Poncorini Pamungkasari3 , Yodi Mahendradhata4
, Yodi Mahendradhata4 , Anni-Maria Pulkki-Brännström5
, Anni-Maria Pulkki-Brännström5 , Ari Probandari3
, Ari Probandari3
-
Journal of Preventive Medicine and Public Health 2023;56(5):467-474.
DOI: https://doi.org/10.3961/jpmph.23.229
Published online: September 26, 2023
- 1,356 Views
- 96 Download
- 1 Crossref
1Doctoral Program of Public Health, School of Graduate, Universitas Sebelas Maret, Surakarta, Indonesia
2Department of Pharmacology, Faculty of Medicine, Universitas Sebelas Maret, Surakarta, Indonesia
3Department of Public Health, Faculty of Medicine, Universitas Sebelas Maret, Surakarta, Indonesia
4Department of Health Policy and Management, Faculty of Medicine, Nursing and Public Health, Universitas Gadjah Mada, Yogyakarta, Indonesia
5Department of Epidemiology and Global Health, Umea University, Umea, Sweden
- Corresponding author: Ratih Puspita Febrinasari, Department of Pharmacology, Faculty of Medicine, Universitas Sebelas Maret, Tamtaman 4 No 125, Rt 01/10, Surakarta 57126, Indonesia, E-mail: ratihpuspita@staff.uns.ac.id
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- Diabetes mellitus (DM) is a serious public health issue that places a heavy financial, social, and health-related burden on individuals, families, and healthcare systems. Self-reported health-related quality of life (HRQoL) is extensively used for monitoring the general population’s health conditions and measuring the effectiveness of interventions. Therefore, this study investigated HRQoL and associated factors among patients with type 2 DM at a primary healthcare center in Indonesia.
-
Methods
- A cross-sectional study was conducted in Klaten District, Central Java, Indonesia, from May 2019 to July 2019. In total, 260 patients with DM registered with National Health Insurance were interviewed. HRQoL was measured with the EuroQol Group’s validated Bahasa Indonesia version of the EuroQoL 5-Dimension 5-Level (EQ-5D-5L) with the Indonesian value set. Multivariate regression models were used to identify factors influencing HRQoL.
-
Results
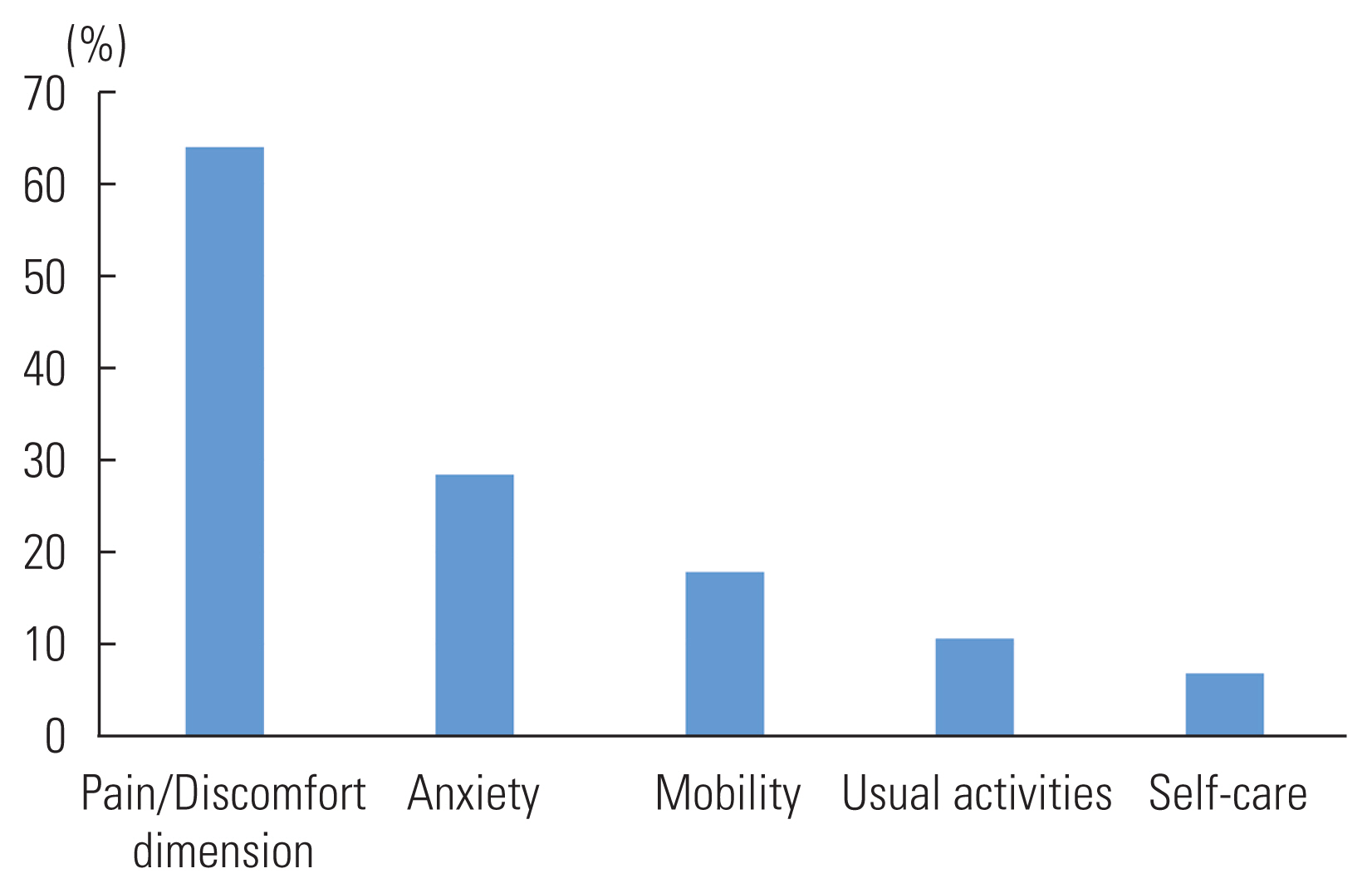
- Data from 24 patients were excluded due to incomplete information. Most participants were men (60.6%), were aged above 50 years (91.5%), had less than a senior high school education (75.0%), and were unemployed (85.6%). The most frequent health problems were reported for the pain/discomfort dimension (64.0%) followed by anxiety (28.4%), mobility (17.8%), usual activities (10.6%), and self-care (6.8%). The average EuroQoL 5-Dimension (EQ-5D) index score was 0.86 (95% confidence interval [CI], 0.83 to 0.88). In the multivariate ordinal regression model, a higher education level (coefficient, 0.08; 95% CI, 0.02 to 0.14) was a significant predictor of the EQ-5D-5L utility score.
-
Conclusions
- Patients with diabetes had poorer EQ-5D-5L utility values than the general population. DM patients experienced pain/discomfort and anxiety. There was a substantial positive relationship between education level and HRQoL.
- Diabetes mellitus (DM) is a major public health concern that imposes significant health, social, and economic burdens worldwide [1,2]. The International Diabetes Federation estimates that 90 million individuals (20–79) in the South-East Asia (SEA) region will have diabetes in 2021, translating to a regional prevalence of 3.9% [2]. The number of people with diabetes in Indonesia exceeds 19.5 million (10.6%), placing it among the highest-prevalence countries in the SEA region [1,2]. Diabetes is a global epidemic that is associated with an aging population, urbanization, poor dietary habits, sedentary lifestyles, and insufficient physical activity [3].
- Health-related quality of life (HRQoL) is a patient-reported outcome measure that is widely utilized to monitor the health status of the general population and to evaluate the efficacy of intervention programs designed by policymakers. This concept encompasses physical, functional, psychological, and emotional functioning [4,5]. It can provide a comprehensive view of an individual’s health condition because it examines both physical and mental health [6]. Therefore, healthcare professionals and researchers not only assess clinical outcomes in patients with diabetes, but also evaluate the disease’s burden and the impact of therapies using self-reported HRQoL measures [7,8]. Furthermore, HRQoL serves as a valuable tool in identifying the most cost-effective interventions, thereby optimizing the return on investment when resources are limited [9].
- Many studies have shown that people with diabetes have impaired HRQoL [10–12]. Furthermore, research has revealed a relationship between poor HRQoL and long-term diabetes and insulin use [8,13,14]. correlation also exists between the prevalence of comorbidities and worse HRQoL among people who have diabetes [15–18]. In addition, age is closely correlated with a decline in HRQoL [9,19], making demographic considerations a significant independent driver of HRQoL in patients with diabetes. Patients with diabetes may also have diminished HRQoL due to poor glycemic management and diabetes-related comorbidities [6,20,21].
- Numerous generic and disease-specific measures have been developed to assess the HRQoL of people who have diabetes [22–25]. The EuroQoL 5-Dimension 5-Level (EQ–5D-5L) questionnaire, a preference-based, multi-attribute utility HRQoL measure, has been validated for use in both clinical and economic evaluations. This utility score, which can be derived from various health conditions, serves as a useful summary. Health technology assessments (HTAs) and other economic analyses that utilize the EQ-5D-5L are being implemented in many countries to guide decisions regarding resource allocation [13,14,26,27]. At present, the Indonesian EuroQoL 5-Dimension (EQ-5D) value set is available for calculating quality-adjusted life years.
- A previous study conducted in Indonesia on patients with type 2 DM revealed that the overall EQ-5D index score was 0.77 (95% confidence interval, 0.75 to 0.79). Men participants had a higher EQ-5D index score compared to their women counterparts. Furthermore, the highest percentage of self-reported health problems (61%) was in the pain/discomfort dimension [14]. However, there have been no previous studies on the HRQoL of patients with type 1 and type 2 DM using the EQ-5D-5L at primary care facilities in Indonesia. Such findings would provide generic EQ-5D-5L index scores based on socio-demographic parameters and clinical state, enabling an analysis of their multivariable relationships. Therefore, the aim of this study was to evaluate the HRQoL and its associated factors among patients with type 2 DM at a primary healthcare center in Indonesia.
INTRODUCTION
- Study Design and Setting
- A cross-sectional study was carried out from May 2019 to July 2019, focusing on patients with DM in the Klaten District of Central Java, Indonesia. Klaten is a district in Central Java where over 83% of the population are members of the National Health Insurance (NHI), and 1% are patients with DM. Patients with DM who are enrolled in the NHI have the opportunity to participate in a diabetes management program known as Prolanis. The goal of this program is to manage complications and enhance the quality of life for these patients.
- Instrument
- We utilized the Bahasa Indonesia version of the EQ-5D-5L, developed by the EuroQol Group (EUROQoL-Group, 2016). The EQ-5D-5L comprises 5 elements: mobility, self-care, regular activities, pain or discomfort, and anxiety or depression. This instrument includes a concise descriptive system questionnaire and an EuroQoL visual analogue scale (EQ-VAS). Initially, patients self-assess their health status across 5 dimensions: mobility, self-care, regular activities, pain/discomfort, and anxiety/depression. Each dimension is rated on a 5-level scale: no problems, slight problems, moderate problems, severe problems, and extreme problems. Participants were requested to evaluate their current health on a 5-point scale. The second component of the instrument is the EQ-VAS, a patient-reported measure of their physical and emotional well-being [28]. Using this method, patients rated their health on a scale from 0 (very poor) to 100 (excellent).
- We also collected socio-demographic (gender, age, working status, and education, primary care facilities frequently visited, type of healthcare services, and participation in the social support group for people with diabetes) and clinical data (duration of diabetes diagnosis and family history).
- Sample and Data Collection Procedure
- The samples in this study consisted of individuals with DM who were registered with the NHI and received primary care services. Prolanis is a management program designed for patients with non-communicable diseases, particularly diabetes and hypertension. The criteria for inclusion in the study were as follows: being 18 years of age or older, having a diagnosis of DM at least six months prior to data collection, being registered in the NHI database before January 1, 2017, and regularly using primary healthcare services. Patients with gestational diabetes or documented cognitive or mental health disorders were excluded from the study. The sample size was calculated using the simple proportion population calculation [28], with a Z-value of 1.96, 95% confidence, and a 5% margin of error. The proportion (P) used for estimating the sample size was set at 50% of patients with type 2 DM who reported a satisfactory overall perceived HRQoL, in order to generate the largest possible sample size. The populations under study were fewer than 10 000 individuals, so the sample sizes were adjusted accordingly. The final determined sample size was 250 [28].
- Due to the short duration of the study and the small sample size, we were unable to employ a random sampling method. Instead, we sequentially recruited participants until we reached an adequate number. Research assistants, who had undergone standard training, were responsible for data collection. To ensure consistency and reduce discrepancies in interpretation among observers, we provided intensive half-day training to all contributors to this study. Participants were recruited through primary healthcare centers. Prior to data collection, all participants were briefed on the objectives and procedures of the study. Assistance was provided by data collectors to any patients who had queries regarding the questionnaire during the information gathering process. The self-reported data collected included health and socio-demographic factors such as age, gender, employment status, education level, duration of illness, and family medical history. Furthermore, self-reporting was utilized for data collection on the visual analogue scale.
- Statistical Analysis
- The demographic data of the study participants were presented using descriptive statistics. The chi-square test was used to examine differences in the proportions of reported issues in relation to patient characteristics. The Indonesian general population time-trade-off value set was utilized to calculate EQ-5D index scores [29]. Given that the EQ-5D-5L utility and EQ-VAS ratings were normally distributed (as confirmed by the Kolmogorov–Smirnov test, p>0.05), we reported the mean and standard deviation. The independent t-test and the analysis of variance were used to compare the EQ-5D-5L utility and EQ-VAS scores of the participants. Logistic regression models were employed to explore potential predictors of HRQoL. The EQ-5D-5L scores were computed using the Indonesian value set [29]. A p-value <0.05 was considered statistically significant. All statistical analyses were conducted using Stata version 14 (StataCorp., College Station, TX, USA).
- Ethics Statement
- The study was approved by the Ethics Review Board of the Medical Ethics Committee of Universitas Sebelas Maret in Surakarta. All study participants who were literate provided written consent prior to any data collection. For those participants who were illiterate, we obtained verbal informed consent. Data were compiled without any personal identifiers. Access to the data was restricted to the research team, and the data were protected with a password.
METHODS
- Socio-demographic Characteristics of the Patients
- A total of 260 patients with DM were interviewed, but due to incomplete information, data from 24 patients were excluded. Consequently, 236 patients were included in the final analyses. The majority of the participants were men (61.0%), over 50 years old (91.5%), had an education level below senior high school (75.0%), and were retired (85.6%). Most sought their routine DM check-up from a private primary healthcare provider (77.1%). More than half of the patients with diabetes participated in a diabetes management program group (50.9%). The duration of their illness ranged from 5 years to 10 years (37.3%). Most respondents reported no family history of DM (61.9%) (Table 1).
- EuroQoL 5-Dimension 5-Level Dimensions
- The self-reported health status of parrelations were observed between the level of education and the mobility, pain/discomfort, and anxiety/depression dimensions (p<0.05). The type of healthcare facility was also found to be associated with the self-care dimension (p<0.05).
- Univariable Association Between EuroQoL 5-Dimension 5-Level Index Scores and Participants’ Characteristics
- The average EQ-5D index score of the study members was 0.86 (95% CI, 0.83 to 0.88) [29]. Women participants showed higher EQ-5D-5L index scores than their men counterparts (Table 2). Participants under the age of 50 and those with higher education levels exhbited better EQ-5D index scores than those aged 50 and over, and those with lower levels of education. Unemployed participants had lower EQ-5D-5L index scores than those who were employed. Participants who utilized private health facilities reported higher EQ-5D index scores than those who used public facilities. Participants who engaged in diabetes management program activities had higher EQ-5D index scores than those who did not participate. The lowest EQ-5D index scores were observed in participants with the longest duration of DM, specifically more than 10 years, compared to those with durations of 5–10 years and less than 5 years. Participants with no family history of DM had lower EQ-5D index scores than those with a family history of the condition.
- Multivariable Associations Between EuroQoL 5-Dimension Index Scores and Participants’ Characteristics
- In the multivariable ordinal regression model, a higher level of education (coefficient, 0.08; 95% CI, 0.02 to 1.14) was a significant predictor of the EQ-5D-5L utility score (Table 3). Factors such as age, gender, employment status, type of healthcare facilities, diabetes management program activities, duration of DM, and family history did not show a significant association with the EQ-5D-5L utility.
RESULTS
- This study investigated HRQoL and its determinants among patients with DM in a primary care setting in Indonesia, using the EQ-5D-5L instrument. Overall, patients with DM reported problems with all dimensions, with percentages ranging from 6.8% to 64.0%. We found that the mean score for patients with DM was 0.86 (95% CI, 0.83 to 0.88), which is higher than the utility score of 0.77 for patients with type 2 DM in Indonesia [14] and also higher than reported by Perwitasari et al. [13] in a study of Indonesia type 2 DM outpatients (n=86), where the mean EQ-5D index score was 0.75 (standard deviation, 0.22). However, compared to the general population, the utility score was lower than that reported for the Indonesian general population (0.91) [29].
- The most frequent health problems were reported in the pain/discomfort dimension (64.0%), followed by anxiety (28.4%), mobility (17.8%), usual activities (10.6%), and self-care (6.8%) (Figure 1). In comparison, a study of the general Indonesian population found a similar pattern, with the most frequent problem being pain/discomfort (39.7%), followed by anxiety/depression (34.2%), usual activities (10.8%), mobility (8.0%), and self-care (1.9%). However, the prevalence was higher in patients with DM than in the general population, indicating that DM significantly impacts HRQoL. Despite this, our findings suggest that most individuals with DM reported fewer problems with mobility and usual activities, implying that the majority of people with DM are able to perform daily routine activities such as work, study, family responsibilities, and leisure activities.
- This study found a correlation between education level and the utility score of the EQ-5D-5L, a finding that aligns with studies conducted in Switzerland [15], Japan [24], and Korea [25]. It is generally understood that a higher level of education can be broadly conceptualized to influence socialization, allocation, economic production, and legitimation, all of which can affect perceptions of quality of life [23]. In line with previous studies [16,17], our findings indicate that women with DM had higher EQ-5D-5L scores than men, and that older individuals had lower EQ-5D-5L scores than their younger counterparts. A possible explanation for this could be that older individuals are more likely to report discomfort and anxiety, express less satisfaction with their condition, and have a reduced capacity for daily activity [14]. Patients with a higher level of education may have a better understanding of their condition, treatment plans, and the complications associated with diabetes. This increased awareness could lead them to take better care of their health, thereby improving their HRQoL [30]. A previous study found that participation in a diabetes management program support group effectively controlled fasting blood sugar levels, hemoglobin A1c, and total cholesterol in patients with DM [31,32]. However, in our study, participation in these groups did not have a significant impact on the EQ-5D index score.
- This study also demonstrated that variables such as women gender, unemployment, lack of participation in diabetes management activities, and a longer duration of diabetes all have a negative coefficient direction. This could potentially be explained by the fact that woman participants are more likely to report issues with anxiety or depression, as they have been found to have more diabetes-related worries and a reduced ability to cope with their disease [14]. Unemployment can lead to numerous negative health consequences, and the long-term stress associated with job loss can result in a diminished quality of life and a worsening of mental conditions [33]. Patients who do not actively participate in diabetes management programs may experience severe complications from their chronic condition. Self-management behavior in individuals with DM encompasses a range of actions, including taking medication, independently monitoring blood sugar levels, regular exercise, and dietary management, along with problem-solving and risk reduction. Participants who were not actively engaged in diabetes self-management exhibited lower health outcomes, including quality of life [34]. A study conducted among type 2 diabetes patients in Ethiopia indicated that a longer duration of DM negatively impacted patients’ quality of life, which may have been related to the discomfort of insulin injections or the pain associated with diabetes complications [35].
- There are some limitations to our study. Since this was a cross-sectional study, it is not possible to establish a causal relationship between HRQoL and its predictors. The study was conducted at a single primary health care center, where the majority of patients had minimal medical comorbidities and issues related to diabetes. Therefore, our findings may not be representative of all diabetes patients throughout Indonesia. Additionally, the study was conducted over a brief period, so potential changes in the severity of health problems over time were not considered. Furthermore, variables such as diabetic foot and diabetic neuropathy were not investigated in this study. Lastly, we did not examine comorbidity variables and the different types of comorbidities.
- Therefore, we recommend conducting longitudinal investigations to identify any potential differences. We also suggest incorporating variables that can evaluate the severity of diabetes, such as complications, diabetic foot, and diabetic neuropathy, as well as comorbidity variables and types of comorbidities. Despite certain limitations, our study established utility values based on an Indonesia-specific value set, thereby eliminating potential bias since preference-based HRQoL measurements differ among populations. Our findings can be leveraged by clinicians and policymakers to develop and implement various initiatives aimed at improving diabetes care. Furthermore, these study results can provide a benchmark for routinely monitoring the impact of therapy or intervention on individuals with diabetes. EQ-5D-5L and other general preference-based measures are commonly used for global health assessments [36]. However, due to their lower sensitivity, we also recommend the use of disease-specific tools for capturing vital signs and symptoms unique to the condition.
- HTA guidelines are currently absent in Indonesia, making the selection of preference-based metrics unclear. This lack of clarity is further complicated by the fact that different preference-based measurements often yield varied results, which can pose a challenge for the ministry in making consistent decisions. In many countries, the EQ-5D-5L is utilized for the evaluation of health technologies [29,37]. The popularity of the EQ-5D-5L stems from its ease of administration, its ability to allow comparisons across different interventions and conditions, and the fact that its data accurately represents the average value for the population of interest [14,26]. The utility values derived from our EQ-5D-5L could be employed to inform future cost-benefit analyses and guide the prioritization of initiatives, programs, and policies aimed at improving the health outcomes of diabetic patients in Indonesia.
DISCUSSION
DATA AVAILABILITY
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Prabowo MH, Probandari A. Data curation: Prabowo MH, Probandari A. Formal analysis: Prabowo MH, Probandari A. Funding acquisition: None. Methodology: Prabowo MH, Febrinasari RP, Pamungkasari EP, Probandari A. Writing – original draft: Prabowo MH, Febrinasari RP, Pamungkasari EP, Mahendradhata Y, Probandari A. Writing – review & editing: Prabowo MH, Febrinasari RP, Pamungkasari EP, Mahendradhata Y, Pulkki-Brännström AM, Probandari A.
Notes
ACKNOWLEDGEMENTS
- 1. Tran BX, Ohinmaa A, Nguyen LT, Nguyen TA, Nguyen TH. Determinants of health-related quality of life in adults living with HIV in Vietnam. AIDS Care 2011;23(10):1236-1245ArticlePubMed
- 2. Kruk ME, Freedman LP. Assessing health system performance in developing countries: a review of the literature. Health Policy 2008;85(3):263-276ArticlePubMed
- 3. Kularatna S, Whitty JA, Johnson NW, Jayasinghe R, Scuffham PA. EQ-5D-3L derived population norms for health related quality of life in Sri Lanka. PLoS One 2014;9(11):e108434ArticlePubMedPMC
- 4. World Health Organization. Global action plan for the prevention and control of NCDs 2013–2020; 2013 [cited 2023 Mar 10]. Available from: https://www.who.int/publications/i/item/9789241506236
- 5. International Diabetes Federation. IDF diabetes atlas eighth edition; 2017 [cited 2023 Mar 10]. Available from: https://diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN-final.pdf
- 6. Ministry of Health of the Republic of Indonesia. In the year 2030, the prevalence of diabetes mellitus in Indonesia reaches 21,3 million people; 2009 [cited 2023 Mar 10]. Available from: https://www.kemkes.go.id/downloads/resources/download/pusdatin/profil-kesehatan-indonesia/Profil-Kesehatan-2021.pdf (Indonesian)
- 7. Prajapati VB, Blake R, Acharya LD, Seshadri S. Assessment of quality of life in type II diabetic patients using the modified diabetes quality of life (MDQoL)-17 questionnaire. Braz J Pharm Sci 2017;53(4):e17144Article
- 8. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317(7160):703-713ArticlePubMedPMC
- 9. Gold MR, Muennig P. Measure-dependent variation in burden of disease estimates: implications for policy. Med Care 2002;40(3):260-266PubMed
- 10. Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes 2018;16(1):189ArticlePubMedPMCPDF
- 11. Rabin R, Gudex C, Selai C, Herdman M. From translation to version management: a history and review of methods for the cultural adaptation of the EuroQol five-dimensional questionnaire. Value Health 2014;17(1):70-76ArticlePubMed
- 12. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20(10):1727-1736ArticlePubMedPMCPDF
- 13. Perwitasari DA, Urbayatun S, Faridah IN, Masyithah N. Relationship of therapeutic outcome with quality of life on type 2 diabetes mellitus patients in Abdul Azis Singkawang hospital. IOP Conf Ser Mater Sci Eng 2017;259: 012023ArticlePDF
- 14. Arifin B, Idrus LR, van Asselt AD, Purba FD, Perwitasari DA, Thobari JA, et al. Health-related quality of life in Indonesian type 2 diabetes mellitus outpatients measured with the Bahasa version of EQ-5D. Qual Life Res 2019;28(5):1179-1190ArticlePubMedPMCPDF
- 15. Flatz A, Casillas A, Stringhini S, Zuercher E, Burnand B, Peytremann-Bridevaux I. Association between education and quality of diabetes care in Switzerland. Int J Gen Med 2015;8: 87-92ArticlePubMedPMC
- 16. Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, et al. Valuing health-related quality of life in diabetes. Diabetes Care 2002;25(12):2238-2243ArticlePubMedPDF
- 17. Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care 2002;25(3):458-463ArticlePubMedPDF
- 18. Lung TW, Hayes AJ, Hayen A, Farmer A, Clarke PM. A meta-analysis of health state valuations for people with diabetes: explaining the variation across methods and implications for economic evaluation. Qual Life Res 2011;20(10):1669-1678ArticlePubMedPDF
- 19. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2015. p. 9
- 20. Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diabetes 2017;8(4):120-129ArticlePubMedPMC
- 21. Centers for Disease Control and Prevention. Measuring healthy days: population assessment of health-related quality of life; 2000 [cited 2023 Mar 10]. Available from: https://stacks.cdc.gov/view/cdc/6406
- 22. Ruževičius J. Quality of life and of working life: conceptions and research. 17th Toulon-Verona International Conference. Liverpool: John Moores University; 2014. 317-334
- 23. Edgerton JD, Roberts LW, von Below S. Education and quality of life. In: Land K, Michalos A, Sirgy M, editors. Handbook of social indicators and quality of life research. Dordrecht: Springer; 2012. p. 265-296Article
- 24. Sakamaki H, Ikeda S, Ikegami N, Uchigata Y, Iwamoto Y, Origasa H, et al. Measurement of HRQL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value Health 2006;9(1):47-53ArticlePubMed
- 25. Lee WJ, Song KH, Noh JH, Choi YJ, Jo MW. Health-related quality of life using the EuroQol 5D questionnaire in Korean patients with type 2 diabetes. J Korean Med Sci 2012;27(3):255-260ArticlePubMedPMCPDF
- 26. Mehring M, Donnachie E, Bonke FC, Werner C, Schneider A. Disease management programs for patients with type 2 diabetes mellitus in Germany: a longitudinal population-based descriptive study. Diabetol Metab Syndr 2017;9: 37ArticlePubMedPMCPDF
- 27. Sutisna MA, Sutisna MA. Prolanis (Chronic Disease Management Program) practical guide; 2014 [cited 2023 Mar 10]. Available from: https://www.academia.edu/36584774/PROLANIS_Program_Pengelolaan_Penyakit_Kronis_panduan_praktis(Indonesian)
- 28. Israel GD. Determining sample size; 2012 [cited 2023 Mar 10]. Available from: https://www.psycholosphere.com/Determining%20sample%20size%20by%20Glen%20Israel.pdf
- 29. Purba FD, Hunfeld JA, Iskandarsyah A, Fitriana TS, Sadarjoen SS, Ramos-Goñi JM, et al. The Indonesian EQ-5D-5L value set. Pharmacoeconomics 2017;35(11):1153-1165ArticlePubMedPMCPDF
- 30. Saleh F, Ara F, Mumu SJ, Hafez MA. Assessment of health-related quality of life of Bangladeshi patients with type 2 diabetes using the EQ-5D: a cross-sectional study. BMC Res Notes 2015;8: 497ArticlePubMedPMC
- 31. Ahmad M, Rachmawaty R, Sjattar EL, Yusuf S. Prolanis implementation effective to control fasting blood sugar, HBA1C and total cholesterol levels in patients with type 2 diabetes. J Ners 2017;12(1):88-98ArticlePDF
- 32. Raraswati A, Heryaman H, Soetedjo NN. Role of Prolanis program in decreasing fasting blood glucose on type 2 diabetic patient in Puskesmas Kecamatan Jatinangor. J Health Syst 2018;4(2):65-70. (Indonesian)
- 33. Worach-Kardas H, Kostrzewski S. Quality of life and health state of long-term unemployed in older production age. Appl Res Qual Life 2014;9(2):335-353ArticlePubMedPMCPDF
- 34. American Association of Diabetes Educators. An effective model of diabetes care and education: revising the aade7 self-care behaviors®. Diabetes Educ 2020;46(2):139-160ArticlePubMedPDF
- 35. Sendekie AK, Dagnew EM, Tefera BB, Belachew EA. Health-related quality of life and its determinants among patients with diabetes mellitus: a multicentre cross-sectional study in Northwest Ethiopia. BMJ Open 2023;13(1):e068518ArticlePubMedPMC
- 36. Sparring V, Nyström L, Wahlström R, Jonsson PM, Ostman J, Burström K. Diabetes duration and health-related quality of life in individuals with onset of diabetes in the age group 15–34 years - a Swedish population-based study using EQ-5D. BMC Public Health 2013;13: 377ArticlePubMedPMCPDF
- 37. Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27(1):7-22ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- Genetic CYP2A6 Polymorphism May Worsen Glycohemoglobin Levels: Study among Javanese Indonesian Smokers
Christine Patramurti, Dita Maria Virginia
Borneo Journal of Pharmacy.2024; 7(1): 29. CrossRef
 KSPM
KSPM


 PubReader
PubReader ePub Link
ePub Link Cite
Cite