Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 55(6); 2022 > Article
-
Original Article
Associations Between Conventional Healthy Behaviors and Social Distancing During the COVID-19 Pandemic: Evidence From the 2020 Community Health Survey in Korea -
Rang Hee Kwon1
 , Minsoo Jung1,2
, Minsoo Jung1,2
-
Journal of Preventive Medicine and Public Health 2022;55(6):568-577.
DOI: https://doi.org/10.3961/jpmph.22.351
Published online: October 14, 2022
1Department of Health Science, Dongduk Women’s University College of Natural Science, Seoul, Korea
2Center for Community-Based Research, Dana-Farber Cancer Institute, Boston, MA, USA
- Corresponding author: Minsoo Jung, Department of Health Science, Dongduk Women’s University College of Natural Science, 60 Hwarang-ro 13-gil, Seongbuk-gu, Seoul 02748, Korea E-mail: mins.jung@gmail.com
Copyright © 2022 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives:
- Many studies have shown that social distancing, as a non-pharmaceutical intervention (NPI) that is one of the various measures against coronavirus disease 2019 (COVID-19), is an effective preventive measure to suppress the spread of infectious diseases. This study explored the relationships between traditional health-related behaviors in Korea and social distancing practices during the COVID-19 pandemic.
-
Methods:
- Data were obtained from the 2020 Community Health Survey conducted by the Korea Disease Control and Prevention Agency (n=98 149). The dependent variable was the degree of social distancing practice to cope with the COVID-19 epidemic. Independent variables included health-risk behaviors and health-promoting behaviors. The moderators were vaccination and unmet medical needs. Predictors affecting the practice of social distancing were identified through hierarchical multiple logistic regression analysis.
-
Results:
- Smokers (adjusted odds ratio [aOR], 0.924) and frequent drinkers (aOR, 0.933) were more likely not to practice social distancing. A greater degree of physical activity was associated with a higher likelihood of practicing social distancing (aOR, 1.029). People who were vaccinated against influenza were more likely to practice social distancing than those who were not (aOR, 1.150). However, people with unmet medical needs were less likely to practice social distancing than those who did not experience unmet medical needs (aOR, 0.757).
-
Conclusions:
- Social distancing practices were related to traditional health behaviors such as smoking, drinking, and physical activity. Their patterns showed a clustering effect of health inequality. Therefore, when establishing a strategy to strengthen social distancing, a strategy to protect the vulnerable should be considered concomitantly.
- As of April 18, 2022, 504 million people worldwide have been infected with coronavirus disease 2019 (COVID-19) and 6.2 million have died [1]. Although about 53% of the world’s population has been vaccinated, it will take a considerable amount of time to end COVID-19 due to the spread of the Omicron variant [2]. Non-pharmaceutical interventions (NPIs) are very important in order to suppress the spread of infection in a situation where the COVID-19 pandemic continues for a long time. NPIs are practical strategies that can protect individuals or communities from contracting diseases independent of vaccination [3]. NPIs include hand washing, mask wearing, ventilation, social distancing, isolation, and school closure. They are relatively simple and cost-effective methods [4]. Of course, in order to end a new infectious disease such as COVID-19, pharmaceutical interventions, such as vaccination, are absolutely necessary. However, since vaccine development and dissemination take a considerable amount of time, NPIs are also needed to slow the spread of the disease as much as possible. Most countries have introduced quarantine measures centered on NPIs in response to COVID-19 [5]. However, there is substantial variation in the practice rate of NPIs among different population groups, and insufficient studies have been conducted on this issue [6,7].
- Social distancing consists of maintaining a 2-m distance from others and avoiding social gatherings [2]. Among NPIs, social distancing is an action that can minimize contact by maintaining distance between people, which can reduce the number of deaths from infection [8]. It has been reported that social distancing, as an NPI that is one of various countermeasures against COVID-19, is an effective preventive measure to suppress the spread of infectious diseases [9]. Moreover, social distancing not only can prevent COVID-19 spread, but can also prevent the spread of infectious respiratory diseases such as influenza, insofar as COVID-19 is mainly spread through droplets emitted from an infected person through actions such as coughing or sneezing [10,11]. Although governments around the world recommend or enforce social distancing as part of quarantine measures, some people do not follow it. Very few studies have focused on people who do not observe social distancing, although many studies have focused on those who do not wear masks.
- Factors that can predict social distancing practices need to be studied in order to prepare for the post-COVID-19 era. Is social distancing a conventional health practice like smoking cessation and physical exercise? Health promotion behaviors are self-directed practices that can help people maintain a higher level of health through regular activities in daily life [12]. Representative health-promoting behaviors include smoking cessation, abstinence from alcohol, and physical activity. These health behaviors have been mainly explained by the health belief model, a cognitive model of the relationship between an individual’s health beliefs and health behaviors [13]. According to the health belief model, higher levels of perceived sensitivity, severity, and benefit are associated with a higher likelihood of healthy behavior. Human behavior is influenced not only by an individual’s cognitive level, but also by social relationships and norms. Therefore, the unhealthy effects and negative social perceptions that can result from not practicing NPIs during the COVID-19 pandemic situation can affect an individual’s participation in preventive behavior [14]. A health promotion behavior is an action that a person practices to manage health and prevent infection, and practicing health promotion behavior can strengthen the immune system and reduce negative impacts on health [15]. Therefore, we need to determine whether social distancing can also be considered a health-promoting action. If so, according to previous studies showing that health behavior can affect other health behaviors [16,17], it is possible to predict whether social distancing is practiced using traditional health promotion behavioral variables.
- It is known that there are disparities in the practice of health behavior according to socioeconomic status, which influences access to medical services [18]. Furthermore, lower socioeconomic status is associated with a higher risk of smoking and drinking and a lower amount of physical activity [19]. Therefore, if social distancing is analogous to conventional health behavior, it is also necessary to examine how it is associated with an individual’s socioeconomic status. It is known that socially and economically vulnerable groups have a higher risk of infection with COVID-19 and lower access to medical care [20-23]. In addition, as medical resources are concentrated on confirmed COVID-19 patients, unmet medical needs for existing patients with underlying diseases is also a serious issue [24]. Therefore, we need to understand the relationship between individual access to medical care and the practice of social distancing.
- Korea has been a model country for quarantine. It responded to COVID-19 with high acceptance of NPIs by the people without the need for a major lockdown. However, in March 2022, the daily number of confirmed COVID-19 cases reached 200 000, the highest in the world [25]. Based on the high vaccination rate of nearly 90%, the Korean government is lifting quarantine measures and requesting individuals to voluntarily practice NPIs. In this study, we explored the relationship between traditional health promotion practices in Korea and social distancing practices during the COVID-19 pandemic. We also examined whether individuals’ pre-COVID-19 medical use behaviors were related to current social distancing practices. In particular, it is important to identify the determinants of social distancing practice in that social distancing is a relatively novel behavior among NPIs. Moreover, in order to promote the practice of social distancing, it is necessary to identify determinants that can be targeted in messages or campaigns for behavioral interventions. Through this study, we intend to develop an NPI strategy to prepare for the post-COVID-19 era.
INTRODUCTION
- Sample
- We used secondary national datasets from the 2020 Community Health Survey conducted by the Korea Disease Control and Prevention Agency (previously known as the Korea Centers for Disease Control and Prevention). Samples were collected using probability proportional cluster sampling. The sample size was 900 people each from 253 public health centers nationwide, and had ±3% desired sampling error with a 95% confidence level. At the sampling point, 5 households on average were selected as samples, and all household members aged ≥19 years in the sample household were interviewed. According to the stratification of the surveyed population, the first stratum was dong/eup/myeon (small administrative units), where 253 community health centers are located across the country; the second one was made up of housing units (apartments and houses). The sample design aimed to produce accurate statistics with a small-scale sample survey, with the help of the stratification of the surveyed population [26]. Thus, the Community Health Survey used a multistage, stratified, random sampling method to be representative of the wider Korean population [27]. In the stratification of the survey population, dong/eup/myeon units located in the jurisdictions of 253 health centers nationwide were divided into primary sampling units (tiers), and housing type (apartments, general houses) units were divided into secondary sampling units [26]. We used 2020 data in which 45-item modules related to COVID-19 were added for the analysis, except for participants with missing information and individuals who responded “not applicable” to medical questions and social distancing (n=98 149).
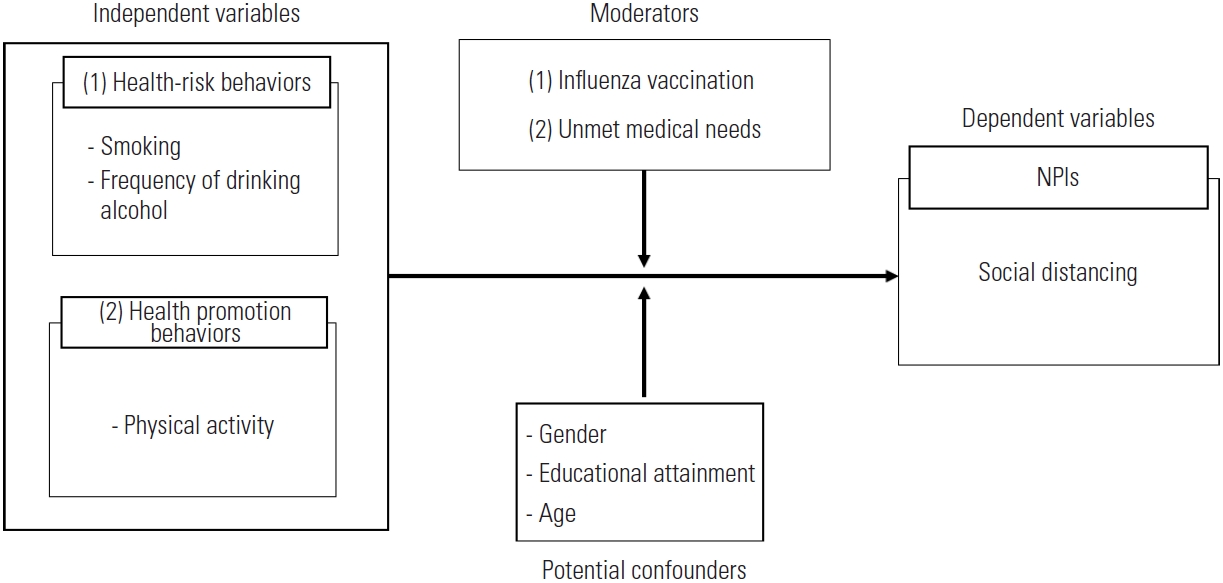
- Analytical Framework
- We designed a research model based on the theoretical basis that positive health behaviors could influence other healthy behaviors [15,16]. Positive health behavior is a lifestyle wherein a person predicts health risks and actively responds to such risks. Therefore, it can be assumed that the practice of social distancing, which is a health behavior to protect oneself from infectious diseases during the COVID-19 pandemic, is also positively related to health behavior. Conversely, it can be assumed that unhealthy behaviors are negatively related to social distancing practices. The integrated behavior model is a model developed by combining the theories of reasoned action and planned behavior. According to the integrated behavior model, the most important determinant of an individual’s behavior is the intention to perform it [28]. Knowledge and skills are also required to perform actions. A person is highly likely to practice behavior when there are no environmental restrictions on behavioral performance, when the behavior is salient, and when he or she has previous experience of performing the behavior. In addition, the intention to act is determined by attitude, perceived norms, perceived control, and self-efficacy. Past behavior can also be a determinant of behavior [29]. Therefore, it is necessary to consider all these components and their interactions when designing interventions to promote health behavior. Based on this theoretical framework that explains traditional health behavior, exploring the effect of individuals’ traditional health behavior on social distancing—a health behavior that is practiced to prevent infections in infectious disease situations—can help to prepare effective interventions to promote social distancing. Through the results of this study, we intend to contribute to preparing an intervention plan to promote social distancing by examining the specific behaviors of people who do not practice social distancing. Meanwhile, since existing health behaviors are associated with socioeconomic status, influenza vaccination experience and unmet medical needs should be considered as potential confounders to reflect health inequalities (Figure 1).
- Measures
- The dependent variable was the degree to which an individual practiced social distancing to cope with the epidemic of COVID-19. In response to the question “Have you practiced the following social distancing during the past week?”, respondents provided information about 4 specific items (“maintain a 2-m healthy distance between people,” “refrain from visits,” “refrain from going out, gatherings, and events,” and “even if we don’t meet, keep in contact with family and close people frequently”), for each of which they responded on a 3-point scale. For each sub-item, answers of “not applicable” were excluded from the analysis. Responses were quantified from “disagree” (1 point) to “strongly agree” (3 points). They were then summed and converted into a continuous variable. Since the distribution of responses appeared to be bimodal, we reclassified social distancing into a binary variable of “non-compliance” (0) and “compliance” (1) and used it for statistical analysis (Cronbach α=0.803).
- The independent variables were health-risk behavior and health-promoting behavior. Respondents answered the following 3 questions: “How many cigarettes have you smoked in your lifetime?”, “Have you ever smoked an e-cigarette?”, and “Have you ever used a heated tobacco products?” We categorized respondents as smokers if they answered “yes” to any of these 3 questions or non-smokers if they answered “no” to all three questions. For the frequency of drinking, when asked, “How often have you drank alcohol in the past year?”, respondents who had never drunk in their lives or who had not drunk alcohol in the past year were classified as “not at all.” Other categories for the frequency of drinking were less than once a month, 2-3 times a month, 2-3 times a week, and more than 4 times a week.
- Regarding health promotion activities, the degree of physical activity was measured with the following 2 questions: “In the past week, how many days did you engage in vigorous physical activity for more than 10 minutes that made you feel very tired or out of breath?” and “How many days did you engage in more than 10 minutes of moderate-intensity physical activity that made you a little tired or out of breath?” In the Community Health Survey, physical activity was measured in 3 areas: vigorous physical activity, moderate physical activity, and walking exercise. However, considering the statistical characteristics of overlapping response tendencies for vigorous and moderate physical activity, we summed up days of physical activity for these 2 types of physical activity and reclassified them into 5 groups: best, upper, middle, lower, and lowest.
- The moderators were vaccination and unmet medical needs. Respondents were asked, “Have you been vaccinated against influenza in the past year?” They answered either “yes” or “no.” Unmet medical needs were measured by the following question: “Did you ever need treatment (exam or treatment) at a hospital (except dentistry) in the past year without receiving it?” Respondents answered either “yes” or “no.”
- Respondents’ gender, education level, and age as potential confounding variables were controlled in the model.
- Statistical Analysis
- First, descriptive statistical analysis was conducted for respondents’ general characteristics. Second, the chi-square test was used to examine the relationship between social distancing practice and the major variables of this study. Third, predictors affecting the practice of social distancing were identified through hierarchical multiple logistic regression analysis. All statistical analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
- Ethics Statement
- This study was deemed exempt by the Korea Disease Control and Prevention Agency Institutional Review Board, because of the anonymous sample.
METHODS
Dependent variables
Independent variables
Moderators
Potential confounders
- Descriptive Statistics of the Sample
- Respondents’ general characteristics are summarized in Table 1. Regarding gender, men and women accounted for 45.2% and 54.8%, respectively. The most common category of education level comprised high school graduates at 34.2%. The age group with the highest frequency was 50-59 years (20.5%). Non-smokers accounted for 66.0% of the sample and smokers accounted for 34.0%. Slightly fewer than half (42.2%) of the respondents did not drink at all. Most respondents (70.5%) rarely exercised. Those who had been vaccinated against influenza in the last year accounted for 58.5% of total subjects. The proportion of people who had experienced unmet medical needs in the past year was 4.8%.
- Associations Between Health-related Behaviors and Practicing Social Distancing
- The results of examining the associations between health-related behaviors and social distancing practice are shown in Table 2. Women practiced social distancing better than men (χ2=220.402, p<0.001). A higher education level was associated with better practice of social distancing (χ2=89.956, p<0.001). Those in their 30s practiced social distancing more than other age groups (χ2=79.975, p<0.001). Non-smokers (χ2=227.500, p<0.001) and those with lower drinking frequency (χ2=239.649, p<0.001) were more likely to practice social distancing than their counterparts. The group with the most physical activity practiced social distancing well (χ2=18.716, p<0.01). Meanwhile, people who had been vaccinated against influenza practiced social distancing relatively well (χ2=81.496, p<0.001). In contrast, the group with unmet medical needs did not practice social distancing relatively well (χ2=85.874, p<0.001).
- Predictors of Social Distancing Practice
- Hierarchical multiple logistic regression analysis was performed for factors affecting the practice of social distancing of all respondents (Table 3). As a result, in model I, women were more likely to practice social distancing than men (odds ratio [OR], 0.801; 95% CI, 0.780 to 0.822). A higher education level (OR, 1.099; 95% CI, 1.083 to 1.115) and older age (OR, 1.029; 95% CI, 1.019 to 1.040) were associated with a higher likelihood of practicing social distancing. In model II, smokers (adjusted odds ratio [aOR], 0.924; 95% CI, 0.891 to 0.959) and frequent drinkers (aOR, 0.933; 95% CI, 0.922 to 0.944) were more likely not to practice social distancing. In model III, a greater degree of physical activity was associated with a higher likelihood of practicing social distancing (aOR, 1.029; 95% CI, 1.015 to 1.043). Next, in model IV, people who were vaccinated against influenza, adjusting for socio-demographic characteristics and health behaviors, were more likely to practice social distancing than those who were not (aOR, 1.150; 95% CI, 1.118 to 1.183). In contrast, people with unmet medical needs were less likely to practice social distancing than those who had not experienced unmet medical needs (aOR, 0.757; 95% CI, 0.712 to 0.803). Thus, influenza vaccination showed a positive moderating effect on practicing social distancing, whereas unsatisfactory medical experiences showed a negative moderating effect.
RESULTS
- Health-promoting behaviors such as smoking cessation, abstinence from alcohol, and physical activity are important disease-preventing behaviors that can prevent chronic diseases and prolong life [30]. Practicing social distancing, one of the NPIs in the COVID-19 situation, is an important action to prevent infection. This study investigated how conventional health-related behaviors such as smoking, drinking alcohol, and physical activity were associated with prevention behaviors against new infectious diseases, such as the practice of social distancing.
- The major findings of this study are as follows. Results showed that women gender, a higher education level, and older age were positively correlated with practicing social distancing. Smokers and frequent drinkers were more likely not to practice social distancing. A greater degree of physical activity was associated with a higher likelihood of practicing social distancing. After controlling for potential confounding variables, people who were vaccinated against influenza were more likely to practice social distancing than those who were not. However, people with unmet medical needs were less likely to practice social distancing than those without such experience. A previous study revealed associations between conventional health behaviors and social distancing practices at the community level [31]. However, it did not identify individuals’ actual practices or intentions because social distancing was measured using global positioning system-enabled devices. Compared to previous studies, this study was significant in that it used data that could grasp the actual degree of social distancing carried out by individuals. The results of this study are similar to those of previous studies showing that smoking negatively affects COVID-19 prevention behavior [32], and this study confirmed that in addition to smoking, other health-related behaviors such as drinking and physical activity were related to COVID-19 prevention behavior. Therefore, practicing health-promoting behavior can increase the ability to promote infection prevention behavior. Because healthy behavior has a clustering characteristic, non-smokers are more likely to drink less and exercise regularly [17,33]. It is necessary to examine the clustering phenomenon of health behaviors because several health-risk behaviors show a synergistic effect on individual health rather than a simple sum of effects [34]. In this study, we determined whether population groups with this cluster characteristic would practice social distancing. The findings could help us design intervention measures to suppress the spread of viruses by understanding the relationship between health-promoting and health-risk behaviors.
- The results of this study indicate that social distancing practices are also closely related to health promotion behaviors systematically based on an empirical dataset. Social distancing is not a conventional disease prevention practice. It is distinct from other NPIs, such as handwashing and wearing a mask, which are primarily health behaviors of individuals themselves. Instead, social distancing is a matter of interpersonal relationships and social norms, as it is an action for the community. This fact shows that whether or not to practice social distancing might be a matter of social structure or health inequality, not an individual’s choice. Therefore, this study attempted to explore the social context that might affect social distancing. This study also examined social distancing as an act of preventing diseases by focusing on socioeconomic inequality. In this study, the effect of unmet medical needs or influenza vaccination, which we added as moderators, showed health inequalities during COVID-19. That is, according to this study, the group with no influenza vaccination experience or unmet medical needs was statistically significantly less likely to practice social distancing than their counterparts. These results showed that social structural factors such as access to medical care were obstacles to the practice of social distancing. In addition, as existing health inequalities are intensified in the COVID-19 situation, vulnerability is also intensified due to complex interactions with other social health determinants such as access to medical care. Therefore, there is a need for a policy approach that can alleviate these discriminatory effects and improve the fundamental social structure.
- Health behaviors are influenced by social networks and individual cognition. For example, people have a tendency to smoke with others rather than alone [35]. Thus, we can conclude that smoking is an important social context that hinders the practice of social distancing. In particular, collectivist tendencies are strong in East Asian cultures, and reference groups are important. People’s behaviors are strongly influenced by social norms [36]. Targeting these reference groups could help us slow the spread of infection because doing so can disseminate positive interventions such as social distancing to a wide range of people [37]. However, social norms can also work the other way around. Just as smoking and drinking alcohol are problems of socioeconomic status and class, the structural problem of inequality can intervene in the practice of social distancing. In other words, there might be people who do not practice social distancing at their own will. There are also people for whom it is structurally impossible to practice social distancing. For example, people with low socioeconomic status who work in essential industries are relatively vulnerable to chronic diseases [38]. Because the pandemic might have amplified inequity in society, people with low income might not have a practical choice to stay at home. In the midst of this situation, as the COVID-19 pandemic prolongs, health-risk behaviors such as alcohol consumption, smoking, and reduced physical activity have increased overall [39,40]. In addition, restrictions on medical use and an increase in unmet medical needs due to COVID-19 have had negative impacts on existing underlying diseases such as cancer [24]. Just as various existing inequality problems in the education and medical fields have been exacerbated through COVID-19, health inequalities are also expected to increase. Social distancing is a policy that suspends daily life and economic activities. It can be a great damage and burden to vulnerable socioeconomic groups. Therefore, we need to check these inequalities through indicators that can predict whether social distancing is practiced. Based on such findings, measures to protect the vulnerable should be considered together when social distancing is enforced.
- This study has several limitations. First, it could not examine all variables that revealed conventional health behaviors. Therefore, more follow-up studies are necessary to understand this mechanism. Second, social distancing is a governmental policy that has been implemented since June 2020. It has been subdivided step-by-step according to the severity of the COVID-19 epidemic and the intensity of quarantine measures. During the COVID-19 pandemic, because the government enforced social distancing, the responses about practicing social distancing could be affected by the timing of the survey. Thus, future studies are necessary to apply a multilevel model. Third, social distancing is a new rule implemented in the COVID-19 situation. It was impossible to compare with previous behaviors because there was no existing social distancing practice rate. Therefore, follow-up studies are needed for ongoing monitoring of social distancing in the future.
- Many studies have shown that social distancing in NPIs is an effective preventive measure to suppress the spread of infectious diseases among various countermeasures against COVID-19. However, there is a large variation in the practice rate of NPIs by population group, and related studies are insufficient. We explored the relationship between traditional health promotion practices in Korea and social distancing practices during the COVID-19 pandemic. We also examined whether individuals’ pre-COVID-19 medical use behaviors were related to current social distancing practices. This study revealed that social distancing practices were related to traditional health behaviors such as smoking, drinking, and physical activity and that their patterns showed a clustering effect of health inequality. Therefore, when establishing a strategy to strengthen social distancing, a strategy to protect the vulnerable should be considered concomitantly, and governments need to identify groups that tend to avoid complying with recommendations.
DISCUSSION
- Participant-level data are available from the corresponding author.
DATA AVAILABILITY
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Both authors contributed equally to conceiving the study, analyzing the data, and writing this paper.
Notes
| Variables | Non-compliance | Compliance | Total |
|---|---|---|---|
| Socio-demographic characteristics | |||
| Gender | |||
| Men | 24 889 (56.2) | 19 429 (43.8) | 44 318 (100) |
| Women | 27 675 (51.4) | 26 156 (48.6) | 53 831 (100) |
| χ² = 220.402*** | |||
| Educational attainment | |||
| Elementary school or less | 11 902 (56.2) | 9258 (43.8) | 21 160 (100) |
| Middle school | 5849 (53.6) | 5069 (46.4) | 10 918 (100) |
| High school | 17 883 (53.2) | 15 704 (46.8) | 33 587 (100) |
| College or post-graduate | 16 930 (52.1) | 15 554 (47.9) | 32 484 (100) |
| χ² = 89.956*** | |||
| Age (y) | |||
| 19-29 | 5859 (55.0) | 4795 (45.0) | 10 654 (100) |
| 30-39 | 5597 (51.4) | 5297 (48.6) | 10 894 (100) |
| 40-49 | 8601 (53.5) | 7476 (46.5) | 16 077 (100) |
| 50-59 | 10 703 (53.1) | 9459 (46.9) | 20 162 (100) |
| 60-69 | 10 297 (52.4) | 9343 (47.6) | 19 640 (100) |
| ≥70 | 11 507 (55.5) | 9215 (44.5) | 20 722 (100) |
| χ² = 73.975*** | |||
| Health-risk behaviors | |||
| Smoking | |||
| Non-smokers | 33 586 (51.8) | 31 211 (48.2) | 64 797 (100) |
| Smokers | 18 978 (56.9) | 14 374 (43.1) | 33 352 (100) |
| χ² = 227.500*** | |||
| Frequency of drinking alcohol | |||
| None | 21 183 (51.2) | 20 224 (48.8) | 41 407 (100) |
| <1/mo | 11 448 (53.3) | 10 047 (46.7) | 21 495 (100) |
| 2-3 times/mo | 9935 (55.7) | 7909 (44.3) | 17 844 (100) |
| 2-3 times/wk | 6992 (56.9) | 5293 (43.1) | 12 285 (100) |
| ≥4 times/wk | 3006 (58.7) | 2112 (41.3) | 5118 (100) |
| χ² = 239.649*** | |||
| Health promotion behaviors | |||
| Degree of physical activity | |||
| Lowest | 37 159 (53.7) | 32 082 (46.3) | 69 241 (100) |
| Lower | 8061 (54.2) | 6803 (45.8) | 14 864 (100) |
| Middle | 4889 (51.9) | 4529 (48.1) | 9418 (100) |
| Upper | 1375 (54.6) | 1145 (45.4) | 2520 (100) |
| Best | 1080 (51.3) | 1026 (48.7) | 2106 (100) |
| χ² = 18.716*** | |||
| Influenza vaccination | |||
| Not vaccinated | 22 500 (55.3) | 18 215 (44.7) | 40 715 (100) |
| Vaccinated | 30 064 (52.3) | 27 370 (47.7) | 57 434 (100) |
| χ² = 81.496*** | |||
| Unmet medical needs | |||
| Experienced | 49 740 (53.2) | 43 713 (46.8) | 93 453 (100) |
| Did not experience | 2824 (60.1) | 1872 (39.9) | 4696 (100) |
| χ² = 85.874*** |
| Variables | Model I | Model II | Model III | Model IV |
|---|---|---|---|---|
| Socio-demographic characteristics | ||||
| Gender (Ref: women) | 0.801 (0.780, 0.822)*** | 0.888 (0.858, 0.920)*** | 0.882 (0.852, 0.914)*** | 0.876 (0.846, 0.908)*** |
| Educational attainment | 1.099 (1.083, 1.115)*** | 1.106 (1.090, 1.123)*** | 1.106 (1.090, 1.123)*** | 1.113 (1.097, 1.129)*** |
| Age | 1.029 (1.019, 1.040)*** | 1.021 (1.010, 1.031)*** | 1.022 (1.012, 1.032)*** | 1.007 (0.996, 1.018) |
| Health-risk behaviors | ||||
| Smoking (Ref: non-smokers) | 0.924 (0.891, 0.959)*** | 0.925 (0.892, 0.960)*** | 0.938 (0.904, 0.973)** | |
| Frequency of drinking alcohol | 0.933 (0.922, 0.944)*** | 0.932 (0.922, 0.943)*** | 0.936 (0.926, 0.947)*** | |
| Health promotion behaviors | ||||
| Degree of physical activity | 1.029 (1.015, 1.043)*** | 1.030 (1.016, 1.044)*** | ||
| Influenza vaccination (Ref: not vaccinated) | 1.150 (1.118, 1.183)*** | |||
| Unmet medical needs (Ref: did not experience) | 0.757 (0.712, 0.803)*** |
- 1. Worldometer. COVID-19 coronavirus pandemic [cited 2022 Apr 18]. Available from: https://www.worldometers.info/coronavirus/#countries
- 2. CDC COVID-19 Response Team. SARS-CoV-2 B.1.1.529 (Omicron) variant - United States, December 1-8, 2021. MMWR Morb Mortal Wkly Rep 2021;70(50):1731-1734ArticlePubMedPMC
- 3. Centers for Disease Control and Prevention. Nonpharmaceutical interventions (NPIs) [cited 2020 Apr 27]. Available from: https://www.cdc.gov/nonpharmaceutical-interventions/
- 4. Imai N, Gaythorpe KA, Abbott S, Bhatia S, van Elsland S, Prem K, et al. Adoption and impact of non-pharmaceutical interventions for COVID-19. Wellcome Open Res 2020;5: 59ArticlePubMedPMCPDF
- 5. Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, et al. COVID-19: towards controlling of a pandemic. Lancet 2020;395(10229):1015-1018ArticlePubMedPMC
- 6. Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-control study of use of personal protective measures and risk for SARS-CoV 2 infection, Thailand. Emerg Infect Dis 2020;26(11):2607-2616ArticlePubMedPMC
- 7. McGrail DJ, Dai J, McAndrews KM, Kalluri R. Enacting national social distancing policies corresponds with dramatic reduction in COVID19 infection rates. PLoS One 2020;15(7):e0236619ArticlePubMedPMC
- 8. Piovani D, Christodoulou MN, Hadjidemetriou A, Pantavou K, Zaza P, Bagos PG, et al. Effect of early application of social distancing interventions on COVID-19 mortality over the first pandemic wave: an analysis of longitudinal data from 37 countries. J Infect 2021;82(1):133-142ArticlePubMed
- 9. Bo Y, Guo C, Lin C, Zeng Y, Li HB, Zhang Y, et al. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int J Infect Dis 2021;102: 247-253ArticlePubMed
- 10. Choe YJ, Lee JK. The impact of social distancing on the transmission of influenza virus, South Korea, 2020. Osong Public Health Res Perspect 2020;11(3):91-92ArticlePubMedPMCPDF
- 11. Lee H, Lee H, Song KH, Kim ES, Park JS, Jung J, et al. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin Infect Dis 2021;73(1):e132-e140ArticlePubMedPDF
- 12. Alpar SE, Senturan L, Karabacak U, Sabuncu N. Change in the health promoting lifestyle behaviour of Turkish University nursing students from beginning to end of nurse training. Nurse Educ Pract 2008;8(6):382-388ArticlePubMed
- 13. Jo HU, Choi EH. The impact of COVID-19 on health prevention behaviors in college students: focusing on the health belief model. J Korean Soc Sch Health 2021;34(2):115-122. (Korean)
- 14. Hong DY, Jeon MA, Cho CH. Predicting preventive behavior intention in COVID-19 pandemic context: application of social variables to health belief model. J Korea Contents Assoc 2021;21(5):22-35. (Korean)
- 15. Xu Y, Chen HF, Yeung WK, Hsieh CW, Yuan HY, Chang LY. Health-promoting behaviors, risk perceptions, and attention to COVID-19-related information: comparing people’s responses to the COVID-19 pandemic across times of Chinese new year and summer 2020 in Hong Kong. Front Public Health 2021;9: 688300ArticlePubMedPMC
- 16. Mechanic D, Cleary PD. Factors associated with the maintenance of positive health behavior. Prev Med 1980;9(6):805-814ArticlePubMed
- 17. Kang E. Clustering of lifestyle behaviors of Korean adults using smoking, drinking, and physical activity. Health Soc Welf Rev 2007;27(2):44-66. (Korean)Article
- 18. Kim HR. Implication of health behaviors in socioeconomic health inequalities and policy directions. Health Welf Policy Forum 2009;149: 36-47. (Korean)
- 19. Nandi A, Glymour MM, Subramanian SV. Association among socioeconomic status, health behaviors, and all-cause mortality in the United States. Epidemiology 2014;25(2):170-177ArticlePubMed
- 20. Clouston SA, Natale G, Link BG. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc Sci Med 2021;268: 113554ArticlePubMed
- 21. Goyal MK, Simpson JN, Boyle MD, Badolato GM, Delaney M, McCarter R, et al. Racial and/or ethnic and socioeconomic disparities of SARS-CoV-2 infection among children. Pediatrics 2020;146(4):e2020009951ArticlePubMedPDF
- 22. Rozenfeld Y, Beam J, Maier H, Haggerson W, Boudreau K, Carlson J, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health 2020;19(1):126ArticlePubMedPMCPDF
- 23. Kim J. Implications of the COVID-19 pandemic on health equity and healthy cities. Korean J Health Educ Promot 2020;37(4):81-89. (Korean)Article
- 24. Balogun OD, Bea VJ, Phillips E. Disparities in cancer outcomes due to COVID-19-A tale of 2 cities. JAMA Oncol 2020;6(10):1531-1532ArticlePubMed
- 25. Lee JH, Park MS, Lee S. The transmission dynamics of SARS-CoV-2 by setting in three waves in the Seoul metropolitan area in South Korea. Health Soc Welf Rev 2021;41(2):7-26. (Korean)
- 26. Kim YT, Choi BY, Lee KO, Kim H, Chun JH, Kim SY, et al. Overview of Korean community health survey. J Korean Med Assoc 2012;55(1):74-83. (Korean)Article
- 27. Kang YW, Ko YS, Kim YJ, Sung KM, Kim HJ, Choi HY, et al. Korea community health survey data profiles. Osong Public Health Res Perspect 2015;6(3):211-217ArticlePubMedPMC
- 28. Montano DE, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior: theory, research, and practice. 5th ed. San Francisco: Jossey-Bass; 2015. p. 95-124
- 29. Hagger MS, Smith SR, Keech JJ, Moyers SA, Hamilton K. Predicting social distancing intention and behavior during the COVID-19 pandemic: an integrated social cognition model. Ann Behav Med 2020;54(10):713-727ArticlePubMedPDF
- 30. Alamian A, Paradis G. Clustering of chronic disease behavioral risk factors in Canadian children and adolescents. Prev Med 2009;48(5):493-499ArticlePubMed
- 31. Bourassa KJ, Sbarra DA, Caspi A, Moffitt TE. Social distancing as a health behavior: county-level movement in the United States during the COVID-19 pandemic is associated with conventional health behaviors. Ann Behav Med 2020;54(8):548-556ArticlePubMedPMC
- 32. de Vries H, van ‘t Riet J, Spigt M, Metsemakers J, van den Akker M, Vermunt JK, et al. Clusters of lifestyle behaviors: results from the Dutch SMILE study. Prev Med 2008;46(3):203-208ArticlePubMed
- 33. Uddin S, Imam T, Khushi M, Khan A, Ali M. How did socio-demographic status and personal attributes influence compliance to COVID-19 preventive behaviours during the early outbreak in Japan? Lessons for pandemic management. Pers Individ Dif 2021;175: 110692ArticlePubMedPMC
- 34. Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Prev Med 2003;36(5):615-623ArticlePubMed
- 35. Ho LL, Li WH, Cheung AT, Xia W, Wang MP, Cheung DY, et al. Impact of COVID-19 on the Hong Kong youth quitline service and quitting behaviors of its users. Int J Environ Res Public Health 2020;17(22):8397ArticlePubMedPMC
- 36. Han J, Choi HS. The relationship between individuals’ collectivistic orientation and social distancing during the COVID-19 crisis in Korea: the mediating role of subjective norm. Korean J Cult Soc Issues 2021;27(3):217-236. (Korean)Article
- 37. Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 2020;4(5):460-471ArticlePubMedPDF
- 38. Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol 2010;36: 349-370ArticlePubMedPMC
- 39. Zajacova A, Jehn A, Stackhouse M, Denice P, Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Can J Public Health 2020;111(6):953-962ArticlePubMedPMCPDF
- 40. Lesser IA, Nienhuis CP. The Impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health 2020;17(11):3899ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- Behavioral Predictors Associated With COVID-19 Vaccination and Infection Among Men Who Have Sex With Men in Korea
Minsoo Jung
Journal of Preventive Medicine and Public Health.2024; 57(1): 28. CrossRef - Physical Distancing for Gay Men from People Living with HIV During the COVID-19 Pandemic
Minsoo Jung
Journal of Homosexuality.2024; : 1. CrossRef - Factors Affecting Adherence to Social Distancing among Adults Aged 19–44 Years: Insights from a Nationwide Survey during COVID-19 Pandemic
Eun Jung Kim, Mikyong Byun
Medicina.2024; 60(5): 827. CrossRef - Non-rigorous versus rigorous home confinement differently impacts mental health, quality of life and behaviors. Which one was better? A cross-sectional study with older Brazilian adults during covid-19 first wave
Lucimere Bohn, Pedro Pugliesi Abdalla, Euripedes Barsanulfo Gonçalves Gomide, Leonardo Santos Lopes da Silva, André Pereira dos Santos
Archives of Public Health.2023;[Epub] CrossRef
- Figure
- Related articles
-
- Changes in Adolescent Health Behavior and the Exacerbation of Economic Hardship During the COVID-19 Pandemic: A Cross-sectional Study From the Korea Youth Risk Behavior Survey
- Gender Inequalities in Mental Health During the COVID-19 Pandemic: A Population-based Study in Korea
- Associations of Socioeconomic Status With Depression and Quality of Life in Patients With Hypertension: An Analysis of Data From the 2019 Community Health Survey in Korea
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


