Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 51(6); 2018 > Article
-
Original Article
Trends in the Prevalence of Childhood Asthma in Seoul Metropolitan City, Korea: The Seoul Atopy ∙ Asthma-friendly School Project -
Yong Min Cho1
 , Chea-Bong Kim2
, Chea-Bong Kim2 , Kyung Nam Yeon3
, Kyung Nam Yeon3 , Eun Sun Lee3
, Eun Sun Lee3 , KyooSang Kim3
, KyooSang Kim3
-
Journal of Preventive Medicine and Public Health 2018;51(6):275-280.
DOI: https://doi.org/10.3961/jpmph.18.090
Published online: October 8, 2018
1Institute for Life and Environment, SMARTIVE Co., Seoul, Korea
2Environmental Health Center for Asthma, Korea University Medical Center, Seoul, Korea
3Department of Environmental Health Research, Seoul Medical Center, Seoul, Korea
- Corresponding author: KyooSang Kim, MD. PhD Department of Environmental Health Research, Seoul Medical Center, 156 Sinnae-ro, Jungnang-gu, Seoul 02053, Korea E-mail: kyoosang@daum.net
• Received: April 18, 2018 • Accepted: October 8, 2018
Copyright © 2018 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- The project Seoul Atopy ∙ Asthma-friendly School investigated the current status of childhood asthma to enable formulation of a preventative policy. We evaluated the current prevalence of childhood asthma in Seoul and its trends and related factors.
-
Methods
- The project was conducted annually from 2011 to 2016 and involved around 35 000 children aged 1-13 years. Based on the International Study of Asthma and Allergies in Childhood guidelines, the survey involved parents. The associations of the particulate matter (PM10) concentration, and the number of days on which the daily air quality guidance level was exceeded in the 25 districts of Seoul, with the prevalence of asthma were assessed.
-
Results
- The age-standardized asthma prevalence in 2011 and 2016 was 6.74 and 4.02%, respectively. The prevalence of lifetime asthma treatment and treatment during the last 12 months tended to decrease from 2011 to 2016. Asthma treatment was significantly correlated with the number of days on which the daily air quality guidance level was exceeded, but not with the PM10 concentration.
-
Conclusions
- This study reports the prevalence of asthma among children in Seoul and confirmed the relationship between childhood asthma and known risk factors in a large-scale survey.
- The repeated exacerbations experienced by children with asthma reduce their quality of life. Asthma treatment is costly, interferes with learning, and has a high disease burden [1]. While genetic factors are related to the incidence of childhood asthma, environmental factors and daily habits are also important [2,3]. Thus, early diagnosis and treatment are necessary to prevent asthma and its exacerbations [4].
- The large social burden of childhood asthma, and the roles of environmental and social factors, suggest that the social component is important for prevention and control of the disease. Prevention rather than follow-up management should be prioritized to reduce the social burden of childhood asthma. To this end, the disease status, and trends therein over time according to various factors, should be monitored. Also, identifying and controlling factors related to the incidence and exacerbations of childhood asthma are important.
- The Seoul Atopy ∙Asthma-friendly School project was designed as a public service supported by the Seoul Government to prevent atopy and asthma in children from 2008 to the present. The project involves medical screening tests for atopy dermatitis; education programs for children, parents, and teachers; environmental management of kindergartens and primary schools; and regular monitoring of risk factors.
- The prevalence of childhood asthma in Korea and other countries has been investigated extensively. The International Study of Asthma and Allergies in Childhood (ISAAC) assessed the prevalence of childhood asthma without the need for a medical examination [5,6] and reported values at the country and city level [7-9]. Some studies compared the prevalence of asthma and allergic diseases by locality or population, while others identified related factors, such as genetics, ambient and/or indoor air quality, secondhand smoking, lifestyle, and socioeconomic status [10,11]. Epidemiological studies using ISSAC have assessed the risk of development and exacerbation of childhood asthma. Attempts should be made to routinely identify already-known risk factors, and to report prevalence at the community level.
- In Seoul, particulate matter (PM10) has recently emerged as an important environmental issue. For this reason, regular monitoring of environmental exposure levels and health effects has been implemented. The efficacy of these measures in terms of reducing the prevalence of childhood asthma needs to be evaluated.
- Regular surveys of a representative population of local communities would allow assessment of the prevalence, trends, and risk factors of childhood asthma, as well as the effects of prevention policies.
- The present study arose from the Seoul Atopy∙Asthma-friendly School project and aimed to provide large-scale data that can be used in the formulation of environmental health policies in local communities. Therefore, we assessed the prevalence of childhood asthma and verified relationship between childhood asthma and its risk factors already known via previous studies such as parents’ history, average income, parents’ education and PM10.
INTRODUCTION
- Sampling
- The Seoul Atopy∙Asthma-friendly School project investigated the prevalence of childhood asthma, provided screening free of charge, educated people regarding prevention of the disease, and supported schools and children in low income families. A total of 30 000 subjects were surveyed annually in preschools, kindergartens, and elementary schools, which were equally supported by the local government. Also, a questionnaire was distributed in community health centers. The data are from a cross-sectional study conducted from 2011 to 2016. The investigation took place from May to November, during which time a questionnaire was sent to parents in the form of a school newsletter. Parents who refused to participate were not included in the survey. This study was approved by the institutional review board of Seoul Medical Center (no. 2017-12-002), and all participants provided written informed consent.
- International Study of Asthma and Allergies in Childhood Questionnaire
- This study was conducted based on the ISAAC guidelines [4-6] using the Korean version of the ISAAC questionnaire, the reliability and validity of which have been verified [12]. The questions assessed whether asthma and allergic diseases were diagnosed by a physician, as well as demographic characteristics, parents’ medical history, and socioeconomic status. The lifetime prevalence of symptoms was assessed by a question on whether the patient was being treated by a physician for those symptoms. Also, treatment rates mean cure rates calculated from experiences of received medical treatment due to asthma during the last 12 months.
- Data were extracted using a scanner, and missing data were addressed by reference to the data present in the questionnaire. In addition, staff in charge of the investigation cleaned the data after reviewing them in raw form. We analyzed the lifetime prevalence of treated symptoms.
- Ambient Air Quality
- Seoul is composed of 25 districts, each with local governments. Real-time national air quality data obtained by local governments from 2011 to 2016 were accessed via a public Website (www.airkorea.or.kr) run by the Ministry of the Environment. The mean PM10 concentration of each district was summarized and checked to obtain the annual mean concentration. In addition, the number of days per month on which the standard PM10 concentration (100 μg/m3) was exceeded was calculated.
- Data Analysis
- The mean PM10 concentration and the number of days per month on which the standard PM10 concentration was exceeded in each district were matched with the asthma data for that district.
- Because we did not consider the individual ppulations of the districts, the age-standardized prevalence rate (ASR) was calculated. The ASR was calculated for 1-12-year-olds based on resident registration data, using the 2010 population data for Seoul as the reference. The parameters of interest were calculated as follows: prevalence rate (Pi) (affected people÷100 000 people)=Xi/Ni×100 000;
- where Ni indicates the population in the its age group, Xi is the number of cases of asthma, Pi is the prevalence rate, and Wi indicates the standard population. Children aged 1-12 years were subjected to analyses by age group. The Pi was analyzed using descriptive statistics. The odds ratio (OR) and 95% confidence interval (CI) of risk factors for asthma prevalence were assessed by univariate logistic regression analyses. A multiple logistic regression analysis was applied after adjustment for age and sex. SPSS version 23 (IBM Corp., Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) were used for statistical analyses of the Pi and risk factors, respectively, of childhood asthma.
METHODS
- Prevalence and Trends of Childhood Asthma
- The general characteristics of the subjects are presented in Table 1. Around 35 000 students participated in the study annually. The mean age of the children in 2010 was 7.75 years and tended to decrease thereafter.
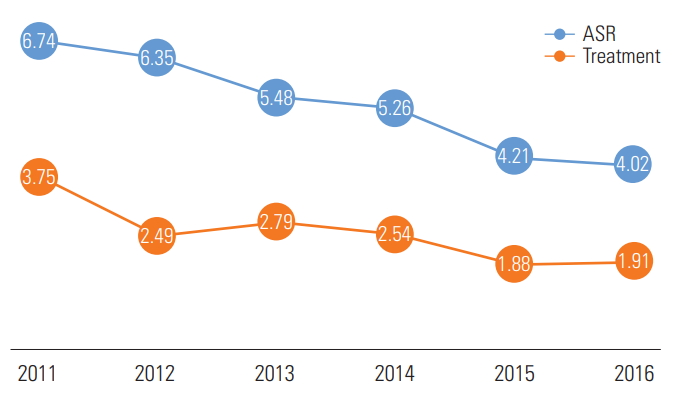
- Because of this change in the mean age of the subjects, the annual ASR was calculated. The total ASR in 2011 was 6.74% and decreased to 4.02% in 2016. The rate of hospital treatment for asthma decreased from 3.75% in 2010 to 1.91% in 2016 (Figure 1).
- Relationship Between Risk Factors for and the Prevalence of Childhood Asthma
- Factors related to asthma were identified using the lifetime prevalence as the dependent variable (Table 2). A history of allergic diseases in the parents was associated with a 2.39-fold higher lifetime asthma prevalence risk (OR, 2.39; 95% CI, 2.18 to 2.62); sex showed no such association. The asthma prevalence risk increased 1.13-fold (OR, 1.13; 95% CI, 1.12 to 1.15) for each 1 year increment in age.
- Children in families with the highest income level had a statistically significantly lower asthma risk than those in families with the lowest income level. However, the education level of parents was not significantly correlated with the asthma risk.
- Particulate Matter and Childhood Asthma
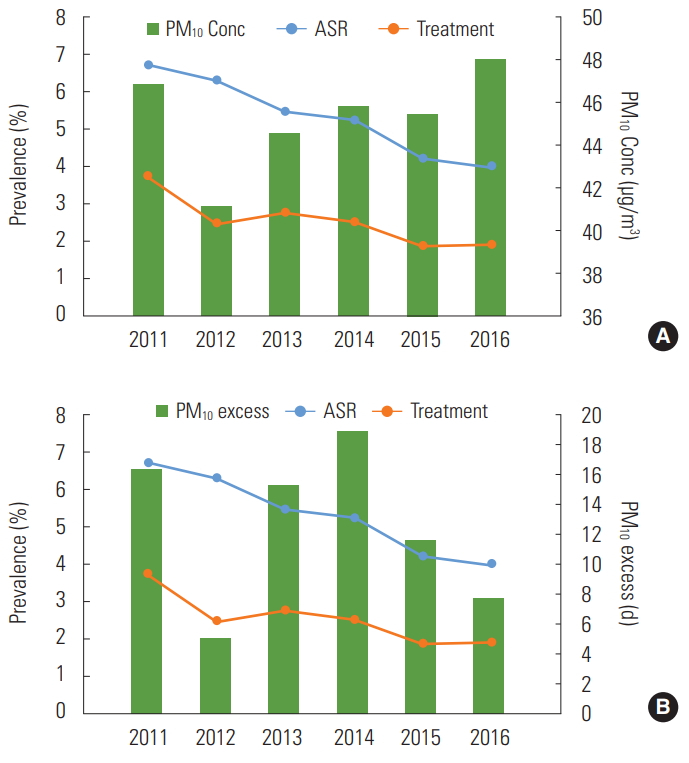
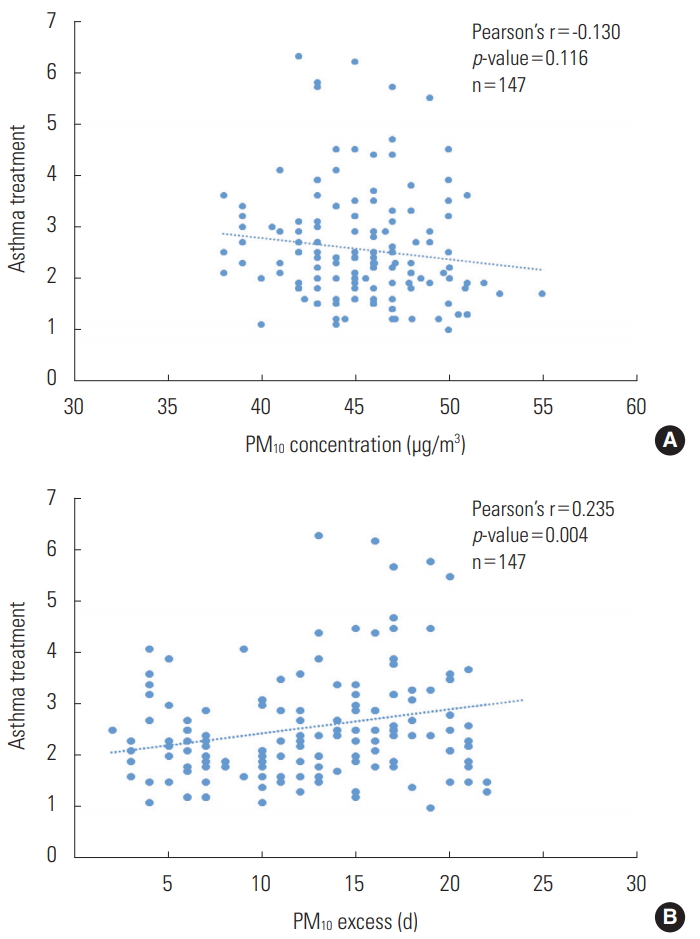
- The annual mean PM10 concentrations and childhood asthma Pis are shown in Figure 2A. The Pi and treatment rate are shown in Figure 1. The annual mean PM10 concentration decreased until 2012 and increased after 2013. The Pi decreased in 2013 but the treatment rate tended to increase. The number of days on which the daily air quality guidance level for PM10 was exceeded was also analyzed (Figure 2B), and the treatment rate for asthma was shown to increase again in 2013 after decreasing in 2012. There was no significant correlation between the monthly mean PM10 concentration and the asthma treatment rate (Pearson’s coefficient, -0.130; Figure 3A). There was a significant correlation between the number of days on which the daily air quality guidance level for PM10 concentration was exceeded and the asthma treatment rate (Pearson’s coefficient, 0.235; p=0.004; Figure 3B).
RESULTS
- The prevalence of childhood asthma in Seoul was 4.0-6.7% from 2011 to 2017. In addition, childhood asthma was significantly related to age, parent’s medical history, household income, and the number of days on which the standard PM10 concentration was exceeded.
- The Pi of childhood asthma decreased over time. A large number of studies in the 2000s, when there was a high level of concern regarding childhood asthma, investigated the prevalence of childhood allergic diseases in Korea. The prevalence of childhood asthma increased from 2000 to 2010 [13], but few studies after the mid-2010s assessed its prevalence in large populations [14-16]; this makes it difficult to verify their findings. Park et al. [14] reported that the prevalence of asthma in children aged 1-9 years peaked in 2011 and decreased thereafter. This trend confirms the results of a recent review, a national survey [15,16], and this study.
- Since 2010, local communities and the central government have attempted to control and raise awareness of childhood allergic diseases. The Ministry of Environment and the Ministry of Health and Welfare have promoted research on, and control measures for, environmental allergic diseases, and local governments established centers for prevention of asthma and allergic diseases through locally representative medical institutions. The reduction in the Pi of asthma after 2010 is likely due to these efforts; however, this should be confirmed by further in-depth research.
- The number of days on which the daily air quality guidance level for PM10 was exceeded was more strongly correlated with asthma treatment than the mean PM10 concentration. This suggests that rapid, short-term increases in PM10 led to an increased rate of hospital treatment, including in the emergency ward, as reported in a recent meta analysis [17].
- Genetic and socioeconomic factors were related to the incidence of childhood asthma in this study, similar to previous studies in Korea [18,19]. Socioeconomic factors relate to both the surrounding environment and the residential or indoor environment. In this study, household income had a significant association with asthma but parents’ education did not. A similar result has already shown in other study in Korea [20]. For this finding, authors of the previous study suggested that that the hierarchical difference according to the education level may be not significant due to the high enthusiasm for education–the entrance rate into the college is over 80%–in Korea [20]. Differences in the distribution of allergic diseases by region indicate differences in the level of environmental exposure and socioeconomic status [21]. Socioeconomic differences are related to differences in overall residential environment, which are in turn linked to environmental risk factors, such as use of heating oil, indoor air quality, and house dust mites [22]. We report here the annual trends in childhood asthma prevalence according to PM10 concentration in Seoul. Our data also confirm the importance of known risk factors.
- This study had the following limitations. First, the causality of the associations between variables and the prevalence of childhood asthma could not be determined. Second, seasonal trends could not be evaluated because we did not have information on the timing of the development or exacerbations of asthma. Thus, this study has limitations to determine any associations or causations for childhood asthma.
- It is important to reduce the Pi of disease, the burden of mortality, and the number of physician visits [23]. Although reducing the incidence of environmental diseases through national policy is important, multidisciplinary programs with specific goals are also required to reduce the incidence of exacerbations.
- The Seoul Atopy∙Asthma-friendly School project has to date involved 218 067 children in local communities in Seoul, and has determined the long-term trends in and factors related to childhood asthma. The results will enable formulation of environmental health policies aimed at preventing and/or controlling childhood allergic diseases.
DISCUSSION
ACKNOWLEDGEMENTS
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
Notes
Figure. 1.ASR of childhood asthma in Seoul, 2011-2016. ASR, age-standardized prevalence rate (%); treatment, received medical treatment for asthma during the last 12 months.
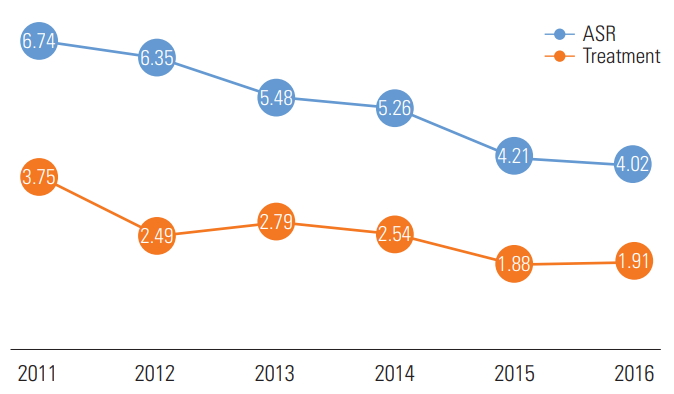
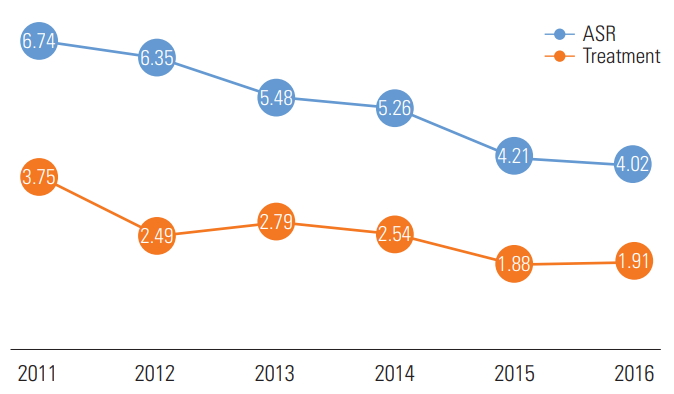
Figure. 2.PM10 Conc (A) and number of days exceeding the standard PM10 Conc (B), and the prevalence of childhood asthma in Seoul, 2011-2016. PM10, particulate matter; Conc, concentration; ASR, age-standardized prevalence rate (%); treatment, rate of experiences of received medical treatment for asthma during the last 12 months; PM10 excess, number of on which the standard PM10 Conc was exceeded.


Figure. 3.Particulate matter (PM10) concentrations of each district (A) and the number of days on which the standard PM10 concentration was exceeded in the districts (B) according to asthma treatment status.
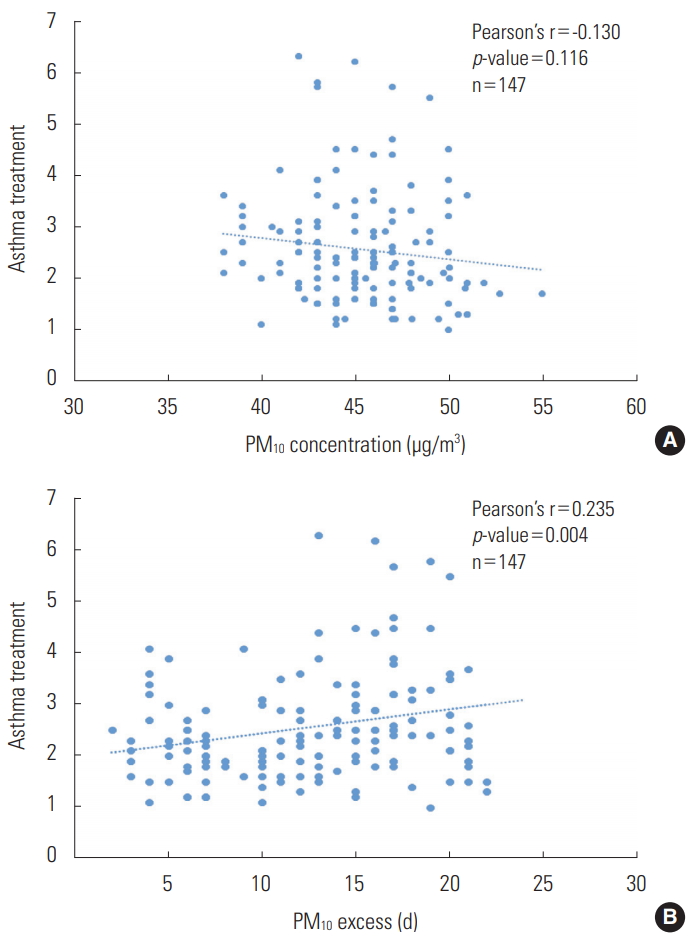
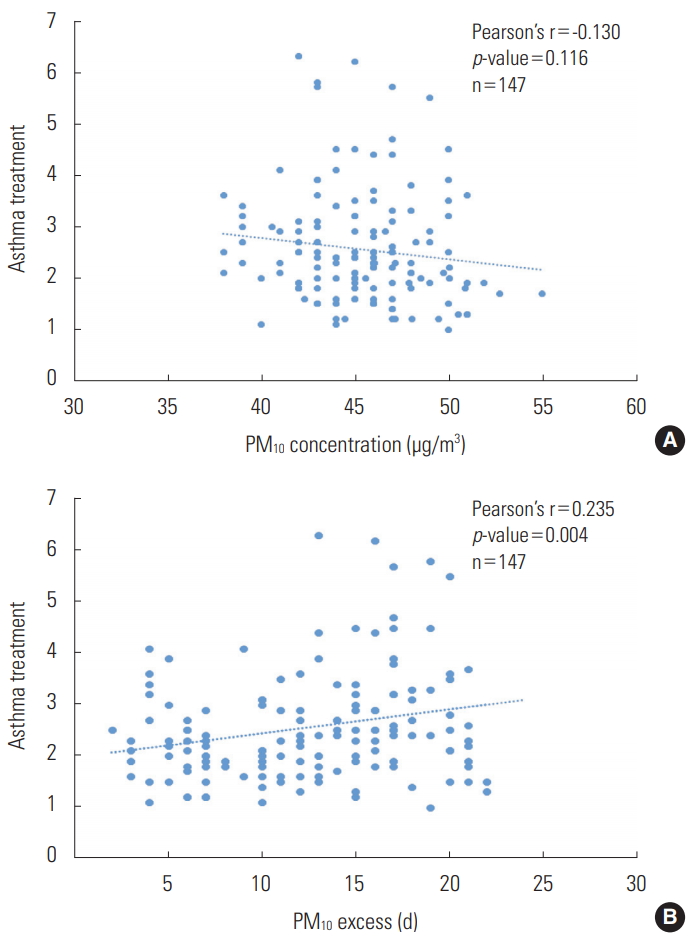
Table 1.General characteristics of the study population
| Characteristics | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|
| Total (n) | 38 985 | 34 098 | 37 226 | 29 312 | 37 400 | 41 046 |
| Sex, n (%) | ||||||
| Girls | 19 357 (49.6) | 16 903 (49.6) | 18 336 (49.3) | 14 471 (49.4) | 19 160 (51.2) | 20 775 (50.6) |
| Boys | 19 628 (50.3) | 17 195 (50.4) | 18 890 (50.7) | 14 841 (50.6) | 18 240 (48.8) | 20 271 (49.4) |
| Sex ratio1 | 1.01 | 1.02 | 1.03 | 1.03 | 0.95 | 0.98 |
| Age, mean±SD (y) | 7.75±2.93 | 7.00±3.05 | 6.47±2.90 | 5.75±2.45 | 6.51±2.85 | 6.24±2.73 |
Table 2.Associations between the prevalence of asthma and the variables of interest
| Variable | OR (95% CI) |
|---|---|
| Sex | |
| Boy | 1.00 (reference) |
| Girl | 1.01 (0.93, 1.09) |
| Age | |
| For 1 y old | 1.13 (1.12, 1.15) |
| Parents’ history1 | |
| No | 1.00 (reference) |
| Yes | 2.39 (2.18, 2.62) |
| Monthly household income (106 KRW) | |
| Low (≤2) | 1.00 (reference) |
| Medium (2-4) | 1.01 (0.88, 1.17) |
| High (≥4) | 0.85 (0.75, 0.96) |
| Parents’ education level | |
| Middle school | 1.00 (reference) |
| Highschool | 0.74 (0.44, 1.26) |
| College | 0.72 (0.43, 1.21) |
| Graduate | 0.74 (0.43, 1.26) |
- 1. Beasley R, Semprini A, Mitchell EA. Risk factors for asthma: is prevention possible? Lancet 2015;386(9998):1075-1085ArticlePubMed
- 2. Yoo Y. Air pollution and childhood allergic disease. Allergy Asthma Respir Dis 2016;4(4):248-256. (Korean)Article
- 3. Kim YR, Seo SC, Yoo Y, Choung JT. Are children with asthma in South Korea also associated with vitamin D deficiency? Environ Health Toxicol 2017;32: e2017005ArticlePubMedPMCPDF
- 4. Kim DI, Yang HJ, Park YM, Rha YH, Choung JT, Pyun BY. Clinical manifestations patterns of allergic disease in Korean children under the age of 6: multi-center study. Korean J Pediatr 2008;51(6):640-645. (Korean)Article
- 5. Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995;8(3):483-491ArticlePubMed
- 6. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998;351(9111):1225-1232ArticlePubMed
- 7. Ahn K, Kim J, Kwon HJ, Chae Y, Hahm MI, Lee KJ, et al. The prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in Korean children: nationwide cross-sectional survey using complex sampling design. J Korean Med Assoc 2011;54(7):769-778. (Korean)Article
- 8. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr 2008;51(4):343-350. (Korean)Article
- 9. Robertson CF, Roberts MF, Kappers JH. Asthma prevalence in Melbourne schoolchildren: have we reached the peak? Med J Aust 2004;180(6):273-276ArticlePubMedPDF
- 10. Seong HU, Cho SD, Park SY, Yang JM, Lim DH, Kim JH, et al. Nationwide survey on the prevalence of allergic diseases according to region and age. Pediatr Allergy Respir Dis 2012;22(3):224-231. (Korean)Article
- 11. Hong S, Son DK, Lim WR, Kim SH, Kim H, Yum HY, et al. The prevalence of atopic dermatitis, asthma, and allergic rhinitis and the comorbidity of allergic diseases in children. Environ Health Toxicol 2012;27: e2012006ArticlePubMedPMCPDF
- 12. Choi SW, Ju YS, Kim DS, Kim JY, Kwon HJ, Kang DH, et al. Reliability and validity of the korean version of ISAAC questionnaire. Korean J Prev Med 1998;31(3):361-371. (Korean)
- 13. Lim H, Kwon HJ, Lim JA, Choi JH, Ha M, Hwang SS, et al. Short-term effect of fine particulate matter on children’s hospital admissions and emergency department visits for asthma: a systematic review and meta-analysis. J Prev Med Public Health 2016;49(4):205-219ArticlePubMedPMCPDF
- 14. Park SY, Kwon HS, Kin H, Yang HJ, Cho YS. The situation of prevalence and incidence of asthma in Korea by the Korean National Health and Nutrition Examination Survey data. Obstr Lung Dis 2016;4(1):23-32. (Korean)
- 15. Kang SY, Song WJ, Cho SH, Chang YS. Time trends of the prevalence of allergic diseases in Korea: a systematic literature review. Asia Pac Allergy 2018;8(1):e8ArticlePubMedPMC
- 16. Korean Statistical Information Service. Statistical database for National Health & Nutrition Survey: chronic obstructive pulmonary disease 2007-2015. [cited 2017 Oct 30]. Available from: http://kosis.kr/eng/statisticsList/statisticsList_01List.jsp?vwcd=MT_ETITLE&parentId=D
- 17. Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS One 2015;10(9):e0138146ArticlePubMedPMC
- 18. Choi WJ, Um IY, Hong S, Yum HY, Kim H, Kwon H. Association between household income and asthma symptoms among elementary school children in Seoul. Environ Health Toxicol 2012;27: e2012020ArticlePubMedPMCPDF
- 19. Cho YM, Ryu SH, Choi MS, Tinyami ET, Seo S, Choung JT, et al. Asthma and allergic diseases in preschool children in Korea: findings from the pilot study of the Korean Surveillance System for Childhood Asthma. J Asthma 2014;51(4):373-379ArticlePubMed
- 20. Hwang GS, Choi JW, Yoo Y, Choung JT, Yoon CS. Residential environmental risk factors for childhood asthma prevalence in metropolitan and semirural cities in Korea. Asia Pac J Public Health 2012;24(1):58-67ArticlePubMed
- 21. Seo S, Kim D, Min S, Paul C, Yoo Y, Choung JT. GIS-based association between PM10 and allergic diseases in Seoul: implications for health and environmental policy. Allergy Asthma Immunol Res 2016;8(1):32-40ArticlePubMed
- 22. Schluger N. Household air quality in high-income countries: forgotten but not gone. Lancet Respir Med 2014;2(10):781-783Article
- 23. Haahtela T, Tuomisto LE, Pietinalho A, Klaukka T, Erhola M, Kaila M, et al. A 10 year asthma programme in Finland: major change for the better. Thorax 2006;61(8):663-670ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Association of exposure to indoor molds and dampness with allergic diseases at water-damaged dwellings in Korea
Seokwon Lee, Seung-Hun Ryu, Woo Jun Sul, Seunghyun Kim, Dohyeong Kim, SungChul Seo
Scientific Reports.2024;[Epub] CrossRef - Trends (2007–2019) of major atopic diseases throughout the life span in a large Mexican population
Martín Becerril-Ángeles, Mario H. Vargas, Ismael Seth Medina-Reyes, Ramón Alberto Rascón-Pacheco
World Allergy Organization Journal.2023; 16(1): 100732. CrossRef - Association between Socioeconomic Status and Healthcare Utilization for Children with Allergic Diseases: Korean National Health and Nutritional Examination Survey (2015–2019)
Jeoungmi Kim, Bomgyeol Kim, Do Hee Kim, Yejin Kim, Vasuki Rajaguru
Healthcare.2023; 11(4): 492. CrossRef - Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019
Youn Ho Shin, Jimin Hwang, Rosie Kwon, Seung Won Lee, Min Seo Kim, Jae Il Shin, Dong Keon Yon
Allergy.2023; 78(8): 2232. CrossRef - Changing Trends in School Absenteeism and Identification of Associated Factors in Adolescents with Atopic Dermatitis
Dong Wan Kang, Sung Hoon Kim, Yechan Kyung, Hae Jeong Lee
Children.2023; 10(12): 1918. CrossRef - Forecasting the Effects of Real-Time Indoor PM2.5 on Peak Expiratory Flow Rates (PEFR) of Asthmatic Children in Korea: A Deep Learning Approach
Jiyoung Woo, Ji-Hyun Lee, Yeonjin Kim, Guillaume Rudasingwa, Dae Hyun Lim, Sungroul Kim
IEEE Access.2022; 10: 19391. CrossRef - Incidence of Asthma, Atopic Dermatitis, and Allergic Rhinitis in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutrition Examination Survey
Hyo Geun Choi, So Young Kim, Yeon-Hee Joo, Hyun-Jin Cho, Sang-Wook Kim, Yung Jin Jeon
International Journal of Environmental Research and Public Health.2022; 19(21): 14274. CrossRef - Factors associated with electronic cigarette use among adolescents asthma in the Republic of Korea
Chang Hoon Han, Jae Ho Chung
Journal of Asthma.2021; 58(11): 1451. CrossRef - Evaluation of changing trend in depression, suicidal ideation, and suicide attempts among adolescents with asthma and identification of associated factors: 11-year national data analysis in 788,411 participants
Yechan Kyung, Young Joo Han, Ju Suk Lee, Jun Hwa Lee, Seon Hui Jo, Sung Hoon Kim
Journal of Asthma.2021; 58(7): 921. CrossRef - The role of the environment in shaping the trends of childhood asthma – An Asian perspective
Agnes S. Y. Leung, Elizabeth Huiwen Tham, Jing Li, Punchama Pacharn, Takumi Takizawa, Eun Lee, Yuhan Xing, Ting‐Fan Leung, Soo‐Jong Hong, Gary W. K. Wong, Ömer Kalaycı
Pediatric Allergy and Immunology.2021; 32(6): 1152. CrossRef - Association of ambient air pollution with depressive and anxiety symptoms in pregnant women: A prospective cohort study
Dirga Kumar Lamichhane, Dal-Young Jung, Yee-Jin Shin, Kyung-Sook Lee, So-Yeon Lee, Kangmo Ahn, Kyung Won Kim, Youn Ho Shin, Dong In Suh, Soo-Jong Hong, Hwan-Cheol Kim
International Journal of Hygiene and Environmental Health.2021; 237: 113823. CrossRef - Association between ambient air pollution and perceived stress in pregnant women
Dirga Kumar Lamichhane, Dal-Young Jung, Yee-Jin Shin, Kyung-Sook Lee, So-Yeon Lee, Kangmo Ahn, Kyung Won Kim, Youn Ho Shin, Dong In Suh, Soo-Jong Hong, Hwan-Cheol Kim
Scientific Reports.2021;[Epub] CrossRef - Ten-Year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017
Jihyun Ha, Seung Won Lee, Dong Keon Yon
Clinical and Experimental Pediatrics.2020; 63(7): 278. CrossRef - Trends in prevalence of allergic diseases in Korean children: how and why?
Kyung Suk Lee
Clinical and Experimental Pediatrics.2020; 63(7): 263. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite