Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 45(2); 2012 > Article
-
Original Article
Trends in Gender-based Health Inequality in a Transitional Society: A Historical Analysis of South Korea - Heeran Chun1, Sung-Il Cho2, Young-Ho Khang3, Minah Kang1, Il-Ho Kim4
-
Journal of Preventive Medicine and Public Health 2012;45(2):113-121.
DOI: https://doi.org/10.3961/jpmph.2012.45.2.113
Published online: March 31, 2012
1Department of Public Administration, Ewha Womans University, Seoul, Korea.
2Department of Epidemiology, School of Public Health, Seoul National University, Seoul, Korea.
3Department of Preventive Medicine, University of Ulsan College of Medicine, Seoul, Korea.
4Social Epidemiological Research Centre for Addiction and Mental Health, Toronto, Canada.
- Corresponding author: Il-Ho Kim, PhD. 33 Russell St. Suit T-306, Toronto, Ontario, M5S 2S1, Canada. Tel: +1-416-535-8501, Fax: +1-416-979-6811, il-ho_kim@camh.net
- *Current affiliation: Faculty of Health Science, Jungwon University, Goesan, Korea.
Copyright © 2012 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- This study examined the trends in gender disparity in the self-rated health of people aged 25 to 64 in South Korea, a rapidly changing society, with specific attention to socio-structural inequality.
-
Methods
- Representative sample data were obtained from six successive, nationwide Social Statistics Surveys of the Korean National Statistical Office performed during 1992 to 2010.
-
Results
- The results showed a convergent trend in poor self-rated health between genders since 1992, with a sharper decline in gender disparity observed in younger adults (aged 25 to 44) than in older adults (aged 45 to 64). The diminishing gender gap seemed to be attributable to an increase in women's educational attainment levels and to their higher status in the labor market.
-
Conclusions
- The study indicated the importance of equitable social opportunities for both genders for understanding the historical trends in the gender gap in the self-reported health data from South Korea.
- Despite reports of converging trends in mortality and life-expectancy between men and women in Western industrialized countries [1,2], numerous reports on gender gaps in morbidity have shown inconsistent patterns [3-5]. In earlier studies, the enhancement of the status of women has been suggested to be reflective of the overall improved health of women and of a reduced gender gap in health status [4,5]; however, few studies have examined this suggestion using historical data. Recently, this assumption has been challenged by empirical studies indicating that the complete removal of the gender gap may not further improve women's health. Using diverse measures of gender equality (political participation, division of labor, and economic resources), a Swedish study found that high levels of gender equality were associated with poorer health, in terms of life expectancy and sick absenteeism, for both men and women [6]. On the other hand, a study in the United States showed that educational enhancement for women explained almost all of women's improved self-rated health (SRH) during the 1970s to 1990s [7]. That study also presented evidence of a reversing pattern in the gender-based health gap in which male health status became lower than that of females among higher socioeconomic groups such as college graduates and full-time workers.
- The dynamics between rapid social change and traditional Confucian culture in South Korea (hereafter "Korea") may have shaped the unique characteristics of its gender-based health inequality. Despite the rapid increase in life expectancy in Korea, it has been reported that women still have higher levels of morbidity and lower levels of perceived health than men, commonly referred to as the "Korean version of the gender health paradox"[8]. Korea is not immune to social and cultural change, even though it may be proceeding at a slow pace. Since the 1990s, patriarchal gender roles at home and gender inequality in politics and the labor market have declined. Recent studies among the Korean population [8,9] have demonstrated and explained the associations between gender inequality and the consistently high levels of female morbidity. These findings added empirical evidence of a change in gender-based health inequality related to Korea's socio-structural inequalities.
- This study examines whether the gender gap in SRH in Korea has narrowed or widened since 1992, in relation to socio-structural factors such as education, occupational class, and employment status. Gender gap trends are assessed using six successive sets of representative Korean national data collected between 1992 and 2010, a period that includes the 1997 Korean economic downturn. Although several reports have described trends in SRH in both men and women [7,10-14], there has been little research comparing and explaining the gender gap trends in SRH. Our study reports on the gender gap trends in SRH with specific attention to socio-structural gender inequality in Korea.
INTRODUCTION
- I. Data
- The data were derived from six Korean Social Statistics Surveys, which were high-quality, large-scale, cross-sectional studies repeatedly undertaken by the Korea National Statistical Office (KNSO). In those surveys, a random sampling study design was applied to selecting more than 30 000 households among the 24 998 Population and Housing Census survey districts, where individuals older than 15 years were interviewed. The KNSO interviews occurred in each sample year. Interview sections on general health status were included in the 1992, 1995, 1999, 2003, 2006, and 2010 surveys. Well-trained interviewers conducted face-to-face interviews across the country and the overall interview success rate was more than 95% for all the surveys in every sample year. The total survey population was approximately 100 000 individuals for each survey. From the total survey population, this study included data for men and women aged 25 to 64, and the study sample was 288 703 (total from the six surveys) of which 51.2% were women.
- II. Health Outcome Measure
- In our study, SRH was used as a health outcome indicator of gender-based differences and their temporal trends. SRH is a simple but useful indicator of morbidity and mortality [15]. This single measure is known to be not only an indicator of current perceived health status but also predictor of future chronic morbidity and mortality [16]. Thus, SRH has been widely used in studies of gender-based health differences. In the six consecutive KNSO surveys, SRH was measured using the following two questions: 1) during the 1992 to 1999 surveys, "How would you rate your health compared to that of others of your own age?" and 2) during the 2003 to 2010 period, "How would you rate your general health status?" The responses were placed on a five point Likert scale, ranging from "very good" to "very poor." The five point scale was dichotomized by combining the categories "poor" and "very poor" as the "poor SRH" category. The remaining three categories of the Likert scale formed a reference.
- III. Independent Variables
- Age, an important health-related covariate, was included when calculating outcomes. The subjects' ages were grouped into four, 10-year age groups (25-34, 35-44, 45-54, and 55-64 years old). Education, occupation, and employment status were the major socio-structural determinants used to examine the effect of socio-structural gender-based inequality on SRH over time. Educational attainment level was classified as tertiary (college or higher), secondary (high school), or primary (middle school or less). The occupational classes included professional (legislators, senior officers and managers, professionals), non-manual (technicians and associate professionals, office workers), manual (service and sales workers, skilled agricultural/forestry/fishery workers, craft and related trades workers, plant/machine operators/assemblers, and unskilled labor), and others (unemployed and non-employed, including housewives, students, and those doing military service). The 2010 survey did not collect data regarding certain occupational categories. For instance, unlike the surveys in 1992 to 2006, in 2010 professionals were categorized as part of the non-manual group. Employment status had been classified into full-time, part-time, self-employed, unpaid-employed, and others, according to the KNSO's definitions of employment status. However, in the 2010 survey sample, the number of full-time and part-time workers grouped together.
- IV. Statistical Methods
- The statistical analyses included examination of age-adjusted prevalence rates to compare the absolute differences between genders, and the multivariate log-binomial regression analysis was used to assess the relative gender gap with men as the reference. Both the absolute (i.e., risk difference and prevalence difference) and relative (i.e., relative risk and prevalence ratio) measures are recommended for detecting health-related inequality [17]. Age-adjusted prevalence was computed using the direct method according to age adjustments for one-year age groups using the 2000 census age distribution as the standard population. As a means of statistical comparison, 95% confidence intervals for the age-adjusted rates were calculated under the assumption that the data form a Poisson distribution. The prevalence ratio (PR), a relative inequality measure, was computed via log-binomial regression using the PROC GENMOD of SAS (SAS Institute Inc., Cary, NC, USA) [18,19], adjusting for age, education, occupation, and employment status.
METHODS
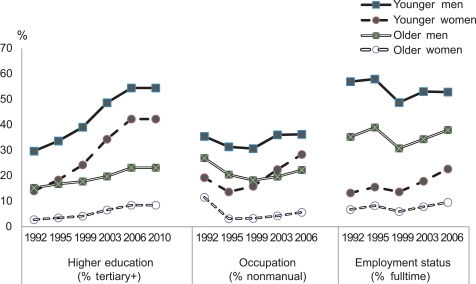
- Table 1 shows the subgroup-specific characteristics by gender over time. The data indicate that fewer women entered higher education and fewer working women were employed in professional, non-manual, or full-time positions than the men in all six surveys. As the gender gap narrowed, the increases in all three socio-structural factors were more pronounced for women than for men over time. The proportions with a tertiary education significantly increased in both genders, but the increase was greater among women (9.8% in 1992 to 35.6% in 2010) than men (24.5% in 1992 to 47.9% in 2010). When disaggregated by age group, the convergent trend in the educational gender gap was more significant for the younger group (Appendix 1). Within the survey period, occupation- and employment-related indicators decreased or remained stable for male workers, whereas some factors showed substantial improvement among women workers such as a 2.1% increase from 1992 to 2006 in the proportion of women in professional occupations and a 6% increase from 1992 to 2006 in the proportion of women in full-time employment.
- Table 2 shows a narrowing gender gap in age-adjusted prevalence of poor SRH between 1992 and 2010, with a consistent pattern of higher poor SRH prevalence among females than among males. The absolute gender difference in age-adjusted prevalence was 11.8% in 1992, and the difference continuously dropped (with the exception of 1999), reaching 4.3% in 2010 (Table 2). Subgroup specific prevalence by gender reveals some insights into the gender and socioeconomic disparity in Korea. Comparing gender groups within the same socioeconomic stratum, men reported consistently better health status than women by all indicators in all of the surveys, except in the "other" categories of the occupation and employment strata (Table 2). These two "other" groups were economically inactive groups that were predominantly women. Graded patterns of educational inequalities were observed in both genders in all of the surveys (Table 2). The gender gap significantly decreased in all of the education strata from 1992 to 2010 (9.2% to 1.2% in tertiary, 9.4% to 1.6% in secondary, and 9.6% to 1.0% in the primary group). During 1992 to 2006, decreasing trends in the gender gap were also detected in the occupation category (14.5% to 0.5% in professional, 12.1% to 2.4% in non-manual, and 19.4% to 4.8% in the manual groups) and employment status (9.3% to 4.1% in full-time, 8.4% to 4.3% in part-time, 10.1% to 6.7% in self-employed, and -1.8% to 1.9% in the unpaid employed groups). In 2010, the consistent pattern of higher levels of poor SRH in women than men, while still present, had started to lose statistical significance, as indicated by the overlapping confidence intervals in the highly educated and non-manual occupation subgroups of the youngest age group (aged 25-34).
- The age-class specific temporal trends in the gender gap are demonstrated in Figure 1. As expected, the prevalence rates were higher in the more advanced age groups for both genders, and the widest gender gaps were in the older groups. Over time, there were significant decreases in the poor SRH gender gaps in all age groups, but not in the 55-64 age group. In total, the gradient of the declining trend in poor SRH prevalence was steeper for women than for men from 1992 to 2010 (11.8% vs. 4.3%), a difference which reflects a decreasing gender gap over time.
- Table 3 displays the magnitude of, and trends in, the relative female to male health inequality ratio among poor SRH subjects over the period 1992 to 2010. Women more than men declared poor SRH in all of the age adjusted surveys. With men as the ratio reference, the age-adjusted female prevalence ratios for poor SRH subjects in all of the age groups dropped from a PR of 1.77 (95% confidence interval [CI], 1.71 to 1.83) in 1992 to a PR of 1.42 (95% CI, 1.34 to 1.51) in 2010, with the downward trend being statistically significant (p<0.001).
- Female PR values for poor SRH subjects were also computed individually for each of the socio-structural determinants and for the combination of all three socio-structural determinants. The individual adjustments for each covariate (education, occupation, and employment status) produced substantial attenuation in the magnitudes of the female PR values. In general, among all of the age groups and survey years, inclusion of employment status produced the greatest decrease in female PR values followed by occupation and education. When the female PR values were stratified by age group, the gender gap in the younger group (when adjusted for the employment status from 2003 to 2010 and the occupation class from 2006 to 2010) became insignificant. After adjusting for education, employment, and occupation in 2010, the gender gap in poor SRH had completely disappeared in both the younger and older groups.
RESULTS
- This study provides evidence that gender-based health inequality has lessened concomitant with an increase in the education, occupation, and employment status of Korean women. That evidence is based on six, successive social surveys (1992-2010) of representative Koreans. The reduction in the gender-based health gap was consistent between both the absolute and relative inequality measures (i.e., prevalence and prevalence ratio differences), although prevalence of poor SRH was still higher among women than among men in all of the surveys. Age-specific comparisons of the trends in the gender gap revealed a greater gap reduction in the younger cohort than in the older cohort over time. The more recent surveys (2006-2010) showed that poor SRH of women, adjusted for either occupation or employment status, was not significantly different from that of men in the young group (aged 25-44). Moreover, after fully adjusting for education, occupation, and employment status, there was no remaining gender gap in either young or old groups in the 2010 survey.
- Our findings on the reduction in the gender gap in SRH in Korea appears to be similar to the temporal trends reported in European and United States studies, but there have been few international reports, including those from developing countries, on gender differences in SRH. A cross-sectional comparative study of gender differences [20] indicated poorer health status in females across a variety of self-reported health measures in Jamaica, Malaysia, Bangladesh, and the United States. That study found that a gender-based health disparity had remained even after adjusting for possible biases in mortality selection related to gender, age, and other socio-demographic factors. In addition, the study pointed out the relative importance of the behavioral and biological bases of the disparity. In contrast, Schnittker [7] reported a temporally changing pattern in United States data with no significant gender differences in SRH (2004). In Finland, more women than men have reported good SRH in several recent studies [5,11,13]. The gender differential in Finland reversed to be in favor of women in the 1970s [11].
- The current study indicates that the reduction in the gender-based health gap is attributable to a greater decrease in the prevalence of poor SRH in women than in men (10.6% vs. 4.0% decrease, respectively, from 1992 to 2010) (Table 2). While women have declared poor SRH at statistically higher rates than did men in all of the successive surveys in Korea, adjustments for three covariates (education, occupational class, and employment status) produced substantial attenuation in the magnitude of the gender gap in each of the surveys. A recent study in the United States supported the assumption that rising education levels and increased labor market participation have contributed to the improvement of women's health over time-corresponding to the narrowing of the gender gap in SRH [7]. All three covariates affected gender-based health inequality, with employment status exhibiting the greatest effect followed by occupational class and finally educational level. Our results support those in the study by Arber and Cooper [4] in the UK, which indicated that occupational class and employment status were the most important factors affecting health in both men and women.
- Our analyses show that the magnitude of the gender gap in SRH diminished significantly over time, with the greatest reduction occurring in younger adults. The poor SRH gender gap estimates attenuated over time, particularly in the younger adults, while it increased until the 2003 survey in the older adults (Table 3). Overall, the gender gap in SRH was wider in older aged subjects due to a sharper increase in poor SRH in women than in men. Some authors suggest that the larger gender disparity among older adults could be an effect of the post-menopausal period of women [21]. Alternatively, we speculate that influences related to life course experiences on SRH assessments could persist in older women. For example, the negative effects of women's experiences during periods of war or extreme poverty may dominate the positive effects of the relatively recent betterment of women's education and occupational status. In contrast, the age-group related differences might be a reflection of reduced gender inequality in the younger cohort. Gender relations in the home have been reported to be increasingly in favor of women within the younger generation in Korea [22,23].
- The implications of our findings are as follows. First, attainment of higher education levels, professional jobs, and full-time employment has remarkably enhanced the SRH status of women more than of men between 1992 and 2010. This suggests that the magnitude of gender inequality in health has not only been weakening, but may reverse in the future if men and women continue to move toward equal social positions. Second, despite the substantial changes in education levels attained, the education covariate seemed to contribute less to the weakening of gender inequality in poor SRH than did the employment and occupational status covariates. A remarkably greater improvement of SRH over time for women than men was found among professional and full-time groups with tertiary education. Finally, our findings showed that these gender-based differential trends in the three factors were more marked when the data were stratified by age group [22,23]. Our covariate-based subgroup analysis of the trends in poor SRH by age also showed similar gender gap patterns. In the latest survey (2010), among the youngest, tertiary-educated, non-manual employees, there was minimal or no gender gap in poor SRH. Consequently, our findings are of particular interest, as the study period included a period of changing, and possibly reversing, temporal patterns in gender gaps affected by age, occupational class, and employment status in Korea.
- There are several limitations of this study. First, this study examined trends in gender-related health differences based on SRH outcomes. Despite the popular use of SRH as an indicator, concerns about the use of SRH as a monitor of health inequalities have been raised. A recent study in the United States showed markedly inconsistent SRH trends among four national surveys [14]. They argued that SRH may not be suitable for monitoring health inequality, particularly among vulnerable groups. In addition, there may be gender-based differential reporting that may have biased this type of health status comparison; inconsistent associations between SRH and mortality according to gender have already been reported [24,25]. However, our previous work showed similar levels of gender differences between SRH and physician-diagnosed chronic diseases in adult Koreans [9]. Second, the findings of this study were based on repeated cross-sectional data, so our analyses may have been affected by a causal relationship between exposure and outcome. This problem may be prominent when estimating the impact of occupational and employment status, as SRH can influence both occupational and employment status rather than vice versa. Regardless, repeated cross-sectional data can provide "representativeness" of the target population for a certain period, which is essential when monitoring trends in health inequality. Third, a change in the way the SRH question was asked occurred in the Social Statistics Survey from 1992 to 1999 (in reference to the same age) to 2003 to 2010 (no reference). While this change may require a more cautious interpretation, the ensuing differences were unlikely to have exerted an influence on our results. In sum, previous evidence has shown that the 'question-changing effect' in SRH would not result in serious differences [26]. Also, our results were similar to those of the 1998 to 2001 Korean National Health and Nutrition Examination Survey, which had used the same question form for measuring SRH. Lastly, there might be effects related to cohort compositional shifts. Thus, age and cohort effects over time may not be easy to differentiate.
- This study provides support for the theory that a progressive increase in women's social status can contribute to the elimination of a gender-based health gap in Korea, a country that shows a high level of gender inequality, slow cultural and attitudinal changes, and rapid economic development. Future cross-cultural validation studies are recommended. Such studies will enhance discussions on the historical processes related to gender-based health gaps in different social contexts.
DISCUSSION
ACKNOWLEDGEMENTS
-
The authors have no conflicts of interest with the material presented in this paper.
-
This article is available at http://jpmph.org/.
Notes
- 1. Trovato F, Heyen NB. A varied pattern of change of the sex differential in survival in the G7 countries. J Biosoc Sci 2006;38(3):391-401. 16613623ArticlePubMed
- 2. Trovato F, Lalu NM. Narrowing sex differentials in life expectancy in the industrialized world: early 1970's to early 1990's. Soc Biol 1996;43(1-2):20-37. 8909108ArticlePubMed
- 3. Macintyre S, Hunt K, Sweeting H. Gender differences in health: are things really as simple as they seem? Soc Sci Med 1996;42(4):617-624. 8643986ArticlePubMed
- 4. Arber S, Cooper H. Gender differences in health in later life: the new paradox? Soc Sci Med 1999;48(1):61-76. 10048838ArticlePubMed
- 5. Lahelma E, Martikainen P, Rahkonen O, Silventoinen K. Gender differences in illhealth in Finland: patterns, magnitude and change. Soc Sci Med 1999;48(1):7-19. 10048834ArticlePubMed
- 6. Backhans MC, Lundberg M, Mansdotter A. Does increased gender equality lead to a convergence of health outcomes for men and women? A study of Swedish municipalities. Soc Sci Med 2007;64(9):1892-1903. 17339070ArticlePubMed
- 7. Schinittker J. Working more and feeling better: women's health, employment, and family life, 1974-2004. Am Sociol Rev 2007;72(2):221-238Article
- 8. Chun H, Doyal L, Payne S, Il-Cho S, Kim IH. Understanding women, health, and social change: the case of South Korea. Int J Health Serv 2006;36(3):575-592. 16981632ArticlePubMed
- 9. Chun H, Khang YH, Kim IH, Cho SI. Explaining gender differences in ill-health in South Korea: the roles of socio-structural, psychosocial, and behavioral factors. Soc Sci Med 2008;67(6):988-1001. 18632197ArticlePubMed
- 10. Gu D, Dupre ME, Warner DF, Zeng Y. Changing health status and health expectancies among older adults in China: gender differences from 1992 to 2002. Soc Sci Med 2009;68(12):2170-2179. 19394120ArticlePubMedPMC
- 11. Heistaro S, Vartiainen E, Puska P. Trends in self-rated health in Finland 1972-1992. Prev Med 1996;25(5):625-632. 8888332ArticlePubMed
- 12. Kawada T, Wakayama Y, Katsumata M, Inagaki H, Otsuka T, Hirata Y, et al. Patterns in self-rated health according to age and sex in a Japanese national survey,1989-2004. Gend Med 2009;6(1):329-334. 19467528ArticlePubMed
- 13. Kunst AE, Bos V, Lahelma E, Bartley M, Lissau I, Regidor E, et al. Trends in socioeconomic inequalities in self-assessed health in 10 European countries. Int J Epidemiol 2005;34(2):295-305. 15563586ArticlePubMed
- 14. Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol 2009;170(3):343-351. 19564169ArticlePubMed
- 15. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997;38(1):21-37. 9097506ArticlePubMed
- 16. Khang YH, Kim HR. Gender differences in self-rated health and mortality association: role of pain-inducing musculoskeletal disorders. J Womens Health (Larchmt) 2010;19(1):109-116. 20088666ArticlePubMed
- 17. Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 1997;44(6):757-771. 9080560ArticlePubMed
- 18. Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol 2005;162(3):199-200. 15987728ArticlePubMed
- 19. Khang YH, Yun SC, Lynch JW. Monitoring trends in socioeconomic health inequalities: it matters how you measure. BMC Public Health 2008;8: 66. 18284701ArticlePubMedPMC
- 20. Rahman O, Strauss J, Gertler P, Ashley D, Fox K. Gender differences in adult health: an international comparison. Gerontologist 1994;34(4):463-469. 7959102ArticlePubMed
- 21. Bird CE, Rieker PP. Gender matters: an integrated model for understanding men's and women's health. Soc Sci Med 1999;48(6):745-755. 10190637ArticlePubMed
- 22. Shin YJ, Won JW, Lee SH, Park SM. Policy direction for the utilization of womens human capital in a low fertility and aging society. 2008. Seoul: Korea Institute for Health and Social Affairs
- 23. Hausmann R, Tyson LD, Zahid S. The global gender gap report 2009. 2009. Geneva: World Economic Forum
- 24. Benyamini Y, Blumstein T, Lusky A, Modan B. Gender differences in the self-rated health-mortality association: is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 2003;43(3):396-405. 12810904ArticlePubMed
- 25. Wolinsky FD, Johnson RJ. Perceived health status and mortality among older men and women. J Gerontol 1992;47(6):S304-S312. 1430868ArticlePubMed
- 26. Eriksson I, Unden AL, Elofsson S. Self-rated health. Comparisons between three different measures. Results from a population study. Int J Epidemiol 2001;30(2):326-333. 11369738ArticlePubMed
REFERENCES
Appendix

| 1992 | 1995 | 1999 | 2003 | 2006 | 2010 | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Age (y) | ||||||
| 25 - 34 | 10 171 (35.9) | 9647 (34.2) | 7182 (30.1) | 6584 (26.9) | 5573 (24.2) | 2710 (21.7) |
| 35 - 44 | 7913 (28.0) | 8452 (30.0) | 7776 (32.5) | 7951 (32.5) | 7115 (30.4) | 3792 (30.3) |
| 45 - 54 | 6086 (21.5) | 5922 (21.0) | 5071 (21.2) | 6045 (24.6) | 6688 (28.6) | 3693 (29.5) |
| 55 - 64 | 4146 (14.6) | 4166 (14.8) | 3867 (16.2) | 3915 (16.0) | 3926 (16.8) | 2315 (18.5) |
| Education | ||||||
| Tertiary | 6929 (24.5) | 7780 (27.6) | 7437 (31.1) | 9047 (36.9) | 9425 (40.3) | 5989 (47.9) |
| Secondary | 11 030 (39.0) | 11 927 (42.3) | 10 371 (43.4) | 10 182 (41.6) | 9476 (40.5) | 4695 (37.5) |
| Primary | 10 357 (36.5) | 8480 (30.1) | 6088 (25.5) | 5266 (21.5) | 4501 (19.2) | 1826 (14.6) |
| Occupation1 | ||||||
| Professional | 2130 (7.5) | 2660 (9.4) | 1899 (8.0) | 2402 (9.8) | 2309 (9.9) | 526 (4.2)2 |
| Non-manual | 7046 (24.9) | 5096 (18.1) | 4325 (18.1) | 4813 (19.7) | 4708 (20.1) | 3397 (27.2)2 |
| Manual | 16 021 (56.6) | 17 826 (63.3) | 14 149 (59.2) | 13 992 (57.1) | 13 062 (55.8) | 5589 (44.7) |
| Others | 3119 (11.0) | 2605 (9.2) | 3523 (14.7) | 3288 (13.4) | 3323 (14.2) | 2998 (23.9) |
| Employment status | ||||||
| Full-time | 13 914 (49.1) | 14 436 (51.2) | 10 042 (42.0) | 11 142 (45.5) | 10 800 (46.2) | 7994 (63.9)3 |
| Part-time | 4606 (16.3) | 4643 (16.5) | 4522 (18.9) | 4624 (18.9) | 4461 (19.1) | - |
| Self-employed | 6913 (24.4) | 6274 (22.3) | 5550 (23.3) | 5267 (21.5) | 4670 (20.0) | 2371 (18.6) |
| Unpaid-employed | 442 (1.6) | 322 (1.2) | 321 (1.4) | 223 (0.9) | 205 (0.9) | 79 (0.6) |
| Others | 2441 (8.6) | 2512 (8.9) | 3461 (14.5) | 3239 (13.2) | 3266 (14.0) | 2066 (16.5) |
| Total | 28 316 | 28 187 | 23 896 | 24 495 | 23 402 | 12510 |
| Women | ||||||
| Age (y) | ||||||
| 25 - 34 | 10 213 (34.6) | 9571 (32.8) | 7258 (29.4) | 7193 (27.5) | 6208 (24.6) | 3029 (23.0) |
| 35 - 44 | 7997 (27.1) | 8573 (29.4) | 2889 (32.0) | 8311 (31.8) | 7632 (30.3) | 3969 (30.1) |
| 45 - 54 | 6342 (21.4) | 6003 (20.6) | 5177 (21.0) | 6195 (23.8) | 6943 (27.5) | 3733 (28.4) |
| 55 - 64 | 4985 (16.9) | 5034 (17.2) | 4345 (17.6) | 4422 (16.9) | 4439 (17.6) | 2436 (18.5) |
| Education | ||||||
| Tertiary | 2881 (9.8) | 3730 (12.8) | 4080 (16.5) | 6033 (23.1) | 6829 (27.1) | 4690 (35.6) |
| Secondary | 8845 (30.0) | 10 398 (35.6) | 9762 (39.6) | 10 732 (41.1) | 10 462 (41.5) | 5269 (40.0) |
| Primary | 17 811 (60.3) | 15 053 (51.6) | 10 827 (43.9) | 9356 (35.8) | 7931 (31.4) | 3208 (24.4) |
| Occupation1 | ||||||
| Professional | 928 (3.1) | 810 (2.8) | 600 (2.4) | 1177 (4.5) | 1357 (5.3) | 86 (0.65)2 |
| Non-manual | 3897 (13.2) | 2020 (9.9) | 2116 (8.6) | 2773 (10.6) | 3217 (12.8) | 2618 (19.9)2 |
| Manual | 11 205 (37.9) | 13 619 (46.7) | 11 212 (45.5) | 10 789 (41.3) | 10 132 (40.2) | 3317 (25.2) |
| Others | 13 507 (45.7) | 12 732 (43.6) | 10 741 (43.5) | 11 382 (43.6) | 10 516 (41.7) | 7146 (54.3) |
| Employment status | ||||||
| Full-time | 3188 (10.8) | 3745 (12.8) | 2636 (10.7) | 3616 (13.8) | 4234 (16.8) | 4979 (37.8)3 |
| Part-time | 4662 (15.8) | 5036 (17.3) | 5252 (21.3) | 5864 (22.5) | 5782 (22.9) | - |
| Self-employed | 3297 (11.2) | 3151 (10.8) | 2519 (10.2) | 2358 (9.0) | 2342 (9.3) | 959 (7.3) |
| Unpaid-employed | 5096 (17.3) | 4520 (15.5) | 3521 (14.3) | 2893 (11.1) | 2348 (9.3) | 1053 (8.0) |
| Others | 13 294 (45.0) | 12 729 (43.6) | 10 741 (43.5) | 11 390 (43.6) | 10 516 (41.7) | 13 167 (8.9) |
| Total | 29 537 | 29 181 | 24 669 | 26 121 | 25 222 | 13 167 |
Values are presented as number (%).
1 Professional occupational class included legislators, senior managers, administrators, and professionals. Non-manual occupational class included technicians, paraprofessionals, and office workers. Manual occupational class included service and sales workers; skilled agricultural, forestry, and fishery workers; craft and related trades workers; plant workers, machine operators, assemblers, and unskilled labor.
2 In the 2010 SSS data, professional occupation class included only legislators, senior managers, and administrators, and non-manual occupational class included professionals, technicians, paraprofessionals, and office workers.
3 In the 2010 SSS data, the numbers of persons in full-time and part-time work were not separately identified.
| 1992 | 1995 | 1999 | 2003 | 2006 | 2010 | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Age (y) | ||||||
| 25 - 34 | 6.7 (6.1, 7.2) | 8.8 (8.2, 9.4) | 7.1 (6.5, 7.7) | 5.6 (5.0, 6.1) | 4.3 (3.8, 4.9) | 5.5 (4.6, 6.4) |
| 35 - 44 | 11.1 (10.3, 11.8) | 12.9 (12.2, 13.7) | 10.5 (9.7, 11.2) | 8.3 (7.7, 9.0) | 7.0 (6.4, 7.7) | 7.5 (6.6, 8.4) |
| 45 - 54 | 17.6 (16.5, 18.6) | 20.1 (18.9, 21.2) | 18.2 (17.0, 19.3) | 15.8 (14.8, 16.9) | 12.9 (12.0, 13.7) | 12.1 (10.9, 13.2) |
| 55 - 64 | 29.6 (27.9, 31.3) | 28.5 (26.8, 30.1) | 27.9 (26.3, 29.6) | 26.5 (24.9, 28.1) | 23.0 (21.4, 24.5) | 19.9 (18.1, 21.7) |
| Education | ||||||
| Tertiary | 8.0 (7.1, 8.8) | 10.4 (9.5, 11.2) | 8.7 (7.9, 9.5) | 6.6 (5.9, 7.2) | 6.3 (5.7, 6.9) | 6.7 (5.9, 7.4) |
| Secondary | 11.7 (10.9, 12.5) | 14.1 (13.3, 14.8) | 13.1 (12.3, 13.8) | 11.3 (10.6, 11.9) | 10.0 (9.3, 10.6) | 10.6 (9.6, 11.7) |
| Primary | 18.6 (17.7, 19.4) | 21.5 (20.4, 22.7) | 20.5 (18.9, 22.1) | 22.4 (19.7, 25.1) | 19.0 (15.7, 22.2) | 20.9 (15.9, 26.1) |
| Occupation | ||||||
| Professional | 6.7 (5.5, 7.8) | 9.2 (8.1, 10.4) | 6.3 (5.1, 7.4) | 5.3 (4.2, 6.4) | 4.8 (3.9, 5.8) | 6.4 (3.5, 9.3)2 |
| Non-manual | 10.8 (9.8, 11.8) | 9.9 (8.8, 11.0) | 8.8 (7.6, 10.0) | 6.4 (5.5, 7.4) | 5.7 (4.7, 6.7) | 5.3 (4.4, 6.1)2 |
| Manual | 13.8 (13.2, 14.3) | 15.3 (14.7, 15.9) | 13.1 (12.5, 13.7) | 11.3 (10.7, 11.8) | 9.0 (8.5, 9.5) | 8.8 (8.0, 9.6) |
| Others | 30.8 (28.5, 33.1) | 37.8 (34.9, 40.7) | 28.2 (26.2, 30.3) | 29.0 (26.9, 31.0) | 25.0 (23.1, 26.9) | 17.7 (16.1, 19.3) |
| Employment status | ||||||
| Full-time | 8.8 (8.2, 9.4) | 11.1 (10.5, 11.7) | 8.3 (7.6, 9.0) | 6.6 (6.1, 7.2) | 5.9 (5.4, 6.5) | 7.5 (6.8, 8.1)3 |
| Part-time | 15.7 (14.5, 16.9) | 18.0 (16.7, 19.3) | 15.1 (13.9, 16.3) | 12.8 (11.7, 13.8) | 10.3 (9.3, 11.2) | , |
| Self-employed | 13.8 (12.9, 14.7) | 15.0 (14.0, 16.0) | 13.0 (12.1, 13.9) | 11.7 (10.6, 12.8) | 8.5 (7.6, 9.4) | 9.4 (7.7, 11.0) |
| Unpaid-employed | 23.9 (17.7, 30.0) | 17.0 (9.6, 24.4) | 20.2 (13.0, 27.4) | 17.6 (10.1, 25.2) | 17.5 (11.4, 23.5) | 12.9 (5.0, 20.7) |
| Others | 38.6 (35.5, 41.7) | 39.1 (36.0, 42.2) | 28.8 (26.7, 30.8) | 29.4 (27.3, 31.5) | 25.6 (23.6, 27.6) | 21.0 (18.8, 23.2) |
| Women | ||||||
| Age (y) | ||||||
| 25 - 34 | 13.7 (13.0, 14.4) | 12.7 (12.0, 13.4) | 11.8 (11.0, 12.6) | 7.0 (6.4, 7.7) | 5.3 (4.8, 5.9) | 6.3 (5.4, 7.2) |
| 35 - 44 | 23.5 (22.4, 24.6) | 23.4 (22.3, 24.4) | 20.8 (19.8, 21.8) | 12.6 (11.9, 13.4) | 9.0 (8.3, 9.7) | 9.5 (8.5, 10.5) |
| 45 - 54 | 33.1 (31.7, 34.6) | 33.8 (32.3, 35.3) | 34.2 (32.6, 35.8) | 27.2 (25.9, 28.5) | 20.0 (18.9, 21.1) | 17.3 (16.0, 18.6) |
| 55 - 64 | 41.3 (39.5, 43.1) | 44.8 (42.9, 46.7) | 46.3 (44.3, 48.4) | 45.2 (43.2, 47.2) | 37.5 (35.6, 39.3) | 31.5 (29.3, 33.8) |
| Education | ||||||
| Tertiary | 17.2 (14.5, 19.9) | 16.8 (14.3, 19.3) | 18.0 (15.4, 20.6) | 10.3 (8.8, 11.9) | 7.8 (6.7, 9.0) | 7.9 (6.8, 9.1) |
| Secondary | 21.1 (19.5, 22.7) | 21.5 (20.1, 22.9) | 21.3 (19.9, 22.6) | 15.6 (14.6, 16.6) | 13.3 (12.4, 14.2) | 12.2 (11.1, 13.2) |
| Primary | 28.2 (27.4, 29.0) | 28.8 (27.8, 29.8) | 29.6 (28.1, 31.0) | 27.7 (24.9, 30.4) | 19.6 (17.3, 21.9) | 21.9 (17.8, 25.9) |
| Occupation | ||||||
| Professional | 21.2 (16.7, 25.8) | 11.9 (9.1, 14.7) | 11.9 (8.2, 15.6) | 8.2 (5.5 , 10.9) | 5.3 (3.1 , 7.5) | 11.6 (4.5, 18.7)2 |
| Non-manual | 22.9 (21.2, 24.6) | 21.0 (16.0, 25.9) | 16.3 (11.7, 20.9) | 9.9 (7.1, 12.7) | 8.1 (5.6, 10.7) | 8.8 (6.4, 11.3)2 |
| Manual | 23.2 (22.3, 24.1) | 24.5 (23.6, 25.3) | 24.3 (23.3, 25.2) | 19.3 (18.4, 20.1) | 14.8 (14.0, 15.6) | 13.8 (12.5, 15.2) |
| Others | 29.9 (28.9, 30.9) | 29.8 (28.7, 30.8) | 28.7 (27.7, 29.8) | 22.5 (21.6, 23.3) | 17.7 (17.0, 18.5) | 15.5 (14.6, 16.4) |
| Employment status | ||||||
| Full-time | 18.1 (16.0, 20.2) | 19.1 (17.3, 20.9) | 17.7 (15.3, 20.1) | 13.1 (11.3, 14.8) | 10.0 (8.3 , 11.6) | 12.8 (11.7, 13.9)3 |
| Part-time | 26.0 (24.4, 27.5) | 25.8 (24.4, 27.2) | 24.3 (22.9, 25.6) | 18.8 (17.6, 20.0) | 14.6 (13.6, 15.7) | , |
| Self-employed | 23.9 (22.2, 25.6) | 25.2 (23.4, 26.9) | 24.8 (22.7, 26.8) | 18.4 (16.7, 20.1) | 15.3 (13.6, 17.0) | 15.2 (12.4, 18.0) |
| Unpaid-employed | 22.1 (20.8, 23.4) | 23.5 (22.1, 24.9) | 25.0 (23.2, 26.7) | 19.5 (17.5, 21.4) | 13.1 (11.9, 14.5) | 12.3 (9.7, 15.0) |
| Others | 30.0 (29.0, 31.0) | 29.7 (28.7, 30.8) | 28.7 (27.7, 29.8) | 22.4 (21.6, 23.3) | 17.7 (17.0, 18.5) | 15.4 (14.5, 16.4) |
| Gender gap | ||||||
| Men | 14.2 (13.8, 14.7) | 15.9 (15.4, 16.4) | 14.1 (13.6, 14.6) | 12.2 (11.7, 12.6) | 10.2 (9.7, 10.6) | 9.9 (9.4, 10.5) |
| Women | 26.0 (25.4, 26.6) | 26.4 (25.8, 27.0) | 25.8 (25.1, 26.4) | 20.0 (19.5, 20.6) | 15.4 (14.9, 15.9) | 14.2 (13.6, 14.8) |
| Prevalence difference (women-men) | 11.8 | 10.5 | 11.7 | 7.8 | 5.2 | 4.3 |
1 Age adjusted prevalence rates were calculated with age adjustments based on one-year age groups using the direct method of standardization to the age distribution in the 2000 census.
2 In contrast with other years’SSS samples, in the 2010 SSS sample, the age adjusted prevalence rates were calculated for the professional occupation group that only included legislators, senior managers, and administrators, and for the non-manual occupational group that included professionals, technicians, paraprofessionals, and office workers.
3 The age adjusted prevalence rates were calculated for workers who combine the numbers of full-time and part-time workers.

Figure & Data
References
Citations

- Temporal trends in educational inequalities in non-communicable diseases in Korea, 2007-2015
Gyu Ri Kim, Chung Mo Nam, C. Mary Schooling
PLOS ONE.2017; 12(12): e0190143. CrossRef - Female disability disadvantage: a global perspective on sex differences in physical function and disability
FELICIA V. WHEATON, EILEEN M. CRIMMINS
Ageing and Society.2016; 36(06): 1136. CrossRef - Gender bias in cardiovascular healthcare of a tertiary care centre of North India
Shibba Takkar Chhabra, Sarbjit Masson, Tripat Kaur, Rajiv Gupta, Sarit Sharma, Abishek Goyal, Bhupinder Singh, Rohit Tandon, Naved Aslam, Bishav Mohan, Gurpreet Singh Wander
Heart Asia.2016; 8(1): 42. CrossRef - Marital Power Dynamics and Well-Being of Marriage Migrants
Hsin-Chieh Chang
Journal of Family Issues.2016; 37(14): 1994. CrossRef - Factors of change and cumulative factors in self-rated health trajectories: A systematic review
Stéphane Cullati, Emmanuel Rousseaux, Alexis Gabadinho, Delphine S. Courvoisier, Claudine Burton-Jeangros
Advances in Life Course Research.2014; 19: 14. CrossRef - The gender gap in sickness absence: long-term trends in eight European countries
A. Mastekaasa
The European Journal of Public Health.2014; 24(4): 656. CrossRef - Gender bias in child care and child health: global patterns
R. Khera, S. Jain, R. Lodha, S. Ramakrishnan
Archives of Disease in Childhood.2014; 99(4): 369. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


