Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 46(1); 2013 > Article
-
Original Article
The Effects of Temperature on Heat-related Illness According to the Characteristics of Patients During the Summer of 2012 in the Republic of Korea - Wonwoong Na1, Jae-Yeon Jang1, Kyung Eun Lee1, Hyunyoung Kim1, Byungyool Jun2, Jun-Wook Kwon2, Soo-Nam Jo2
-
Journal of Preventive Medicine and Public Health 2013;46(1):19-27.
DOI: https://doi.org/10.3961/jpmph.2013.46.1.19
Published online: January 31, 2013
1Department of Preventive Medicine and Public Health, Ajou University School of Medicine, Suwon, Korea.
2Korea Centers for Disease Control and Prevention, Cheongwon, Korea.
- Corresponding author: Soo-Nam Jo, MPH. Osong Health Technology Administration Complex, 187 Osongsaengmyeong 2-ro, Osong-eup, Cheongwon 363-700, Korea. Tel: +82-43-719-7263, Fax: +82-31-219-5084, joria517@gmail.com
• Received: October 10, 2012 • Accepted: November 24, 2012
Copyright © 2013 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- This study was conducted to investigate the relationship between heat-related illnesses developed in the summer of 2012 and temperature.
-
Methods
- The study analyzed data generated by a heat wave surveillance system operated by the Korea Centers for Disease Control and Prevention during the summer of 2012. The daily maximum temperature, average temperature, and maximum heat index were compared to identify the most suitable index for this study. A piecewise linear model was used to identify the threshold temperature and the relative risk (RR) above the threshold temperature according to patient characteristics and region.
-
Results
- The total number of patients during the 3 months was 975. Of the three temperature indicators, the daily maximum temperature showed the best goodness of fit with the model. The RR of the total patient incidence was 1.691 (1.641 to 1.743) per 1℃ after 31.2℃. The RR above the threshold temperature of women (1.822, 1.716 to 1.934) was greater than that of men (1.643, 1.587 to 1.701). The threshold temperature was the lowest in the age group of 20 to 64 (30.4℃), and the RR was the highest in the ≥65 age group (1.863, 1.755 to 1.978). The threshold temperature of the provinces (30.5℃) was lower than that of the metropolitan cities (32.2℃). Metropolitan cities at higher latitudes had a greater RR than other cities at lower latitudes.
-
Conclusions
- The influences of temperature on heat-related illnesses vary according to gender, age, and region. A surveillance system and public health program should reflect these factors in their implementation.
- Due to global climate change, heat waves are increasing in frequency, intensity, and duration [1]. The types of health damages caused by heat waves vary greatly, ranging from death, exacerbation of cardiovascular diseases, respiratory diseases, neurological diseases, and psychiatric diseases to the development of heat-related illnesses [2-9]. In particular, heat-related illnesses, which have a clear causal relationship with heat waves, can exacerbate cardiovascular diseases and can cause death in severe cases [10,11]. Heat-related illnesses are preventable by actions such as avoiding exposure to high temperature environments [12]. Therefore, with proper responses, serious health consequences of heat-related illness can be avoided, also. Damages caused by heat waves are expected to be on the rise with climate change [13]. Accordingly, heat-related morbidity and mortality are likely to grow significantly [14]. Thus, public health programs to prevent the occurrence of heat-related illnesses caused by heat waves will become more important.
- Health impact caused by heat waves is influenced by a threshold temperature, above which damage occurs at a sharply increased level [4,15,16]. The incidence of heat-related morbidity, below the threshold temperature, and at or above the threshold temperature shows a major difference in most cases [17]. The threshold temperature and the increase rate in patients at and above it differ by region [4,18], age, and gender. The threshold temperature is the most critical information in policies for preventing the health impacts of heat waves, as it is used as an indicator for initiating public health response actions to heat waves or to issue heat wave warnings. The rate of increase of patient numbers above a threshold temperature can also be used as an assessment of vulnerability and the evaluation of public health response [19]. Heat-related illnesses are reported to increase steeply above a certain level, with similar outcomes for other health impacts [20]. Nevertheless, the pattern of incidence of heat-related illnesses and its relationship with temperature have rarely been investigated in Korea.
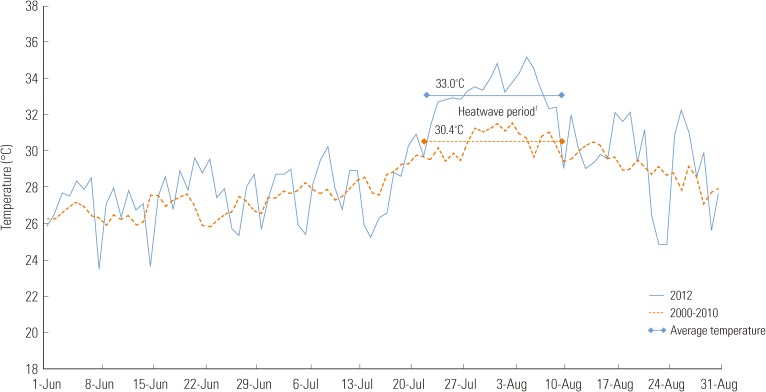
- For three straight weeks from July 22 to August 11, 2012, a record heat wave hit most parts of the nation. The daily maximum temperature stayed above 30℃ and peaked at 38.7℃. During this period, the average daily maximum temperature was 33.0℃, well over the average of the past ten years in the same period of 30.4℃ (Figure 1). The Korea Centers for Disease Control and Prevention (KCDC) has operated a heat wave surveillance system to collect data from patients with heat-related illnesses for three months since June, including the heat wave period. In this study, with the descriptive analysis of the data collected by the heat wave surveillance system, characteristics of the patients affected by the heat-related illnesses in the summer of 2012 were identified. The study also analyzed the rate of patient increase at and above the threshold temperature in examining the relationship between the occurrence of patients with heat-related illnesses and temperature. Moreover, the study was conducted to identify how the threshold temperature and patient increase rates differ according to region and demographic group.
INTRODUCTION
- In the summer of 2012, the KCDC operated a heat wave surveillance system in response to a heat wave, from June 1 to September 6. Among the patients who visited emergency medical institutions participating in this study, the active surveillance system collected the information from patients who were diagnosed with heat-related illnesses due to exposure to the heat waves. Among the total 461 emergency medical institutions nationwide, 458 institutions participated in the study. 250 institutions (54.6% of the total) have reported at least one case. Regionally, Seoul had the largest number of participating institutions, and Jeju, Incheon, and Gyeonggi had the fewest. Personnel in charge at each emergency medical institution reported through an electronic system individual cases of patients with heat-related illnesses who were admitted on the previous day of the reporting. The community health center in each region compiled the data and encouraged emergency medical institutions in their designated area to report cases in case they failed to report. Heat-related illness is listed as T67 in the 10th revision of International Classification of Diseases coding system. It is categorized into heat syncope, heat edema, heat cramp, heat exhaustion, and heat stroke. Items to be reported include: diagnosis, patient's gender and age, date and time of the onset of the symptoms, location of the onset of symptoms, date and time of visit to an emergency medical institution, level of consciousness at the time of the visit, vital signs including blood pressure and body temperature, and outcome of treatment.
- In this study, we used and analyzed the data of the three months in the summer, from June 1 to August 31, among the data of patients with heat-related illnesses collected through the heat wave surveillance system. In categorizing the diagnoses of heat-related illnesses, we integrated heat syncope, heat edema, and heat cramp into mild heat-related illnesses. Age groups were reclassified into three: younger than 19 years (school age); 20 to 64 years (who actively participate in economic activities); and 65 or older. The locations of the onset were categorized into the following: home, workplace both indoors and outdoors, road, fields and paddies, greenhouse, and other indoor and outdoor places. Regions were categorized into 16 cities and provinces in the administrative district, including seven metropolitan cities and nine provinces, based on the address of the medical institution that reports the incidence of cases. The seven cities are Seoul, Incheon, Daejeon, Daegu, Gwangju, Ulsan, and Busan. The nine provinces are Gyeonggi, Gangwon, Chungbuk, Chungnam, Gyeongbuk, Jeonbuk, Jeonnam, and Jeju. Patients with heat-related illnesses were represented by the number of patients per day, according to region, gender, age group, and diagnosis.
- As for meteorological data, we used daily maximum temperature, daily average temperature, and average humidity from 91 weather stations provided by the Korea Meteorological Administration website [21]. The heat index was calculated using the daily maximum temperature and average humidity, according to the formula suggested by the US National Weather Service [22].
- Heat index (°F)=-42.379+2.04901523T+10.14333127R-0.22475541TR-6.83783×10-3T2-5.481717×10-2R2+1.22874×10-3T2R+8.5282×10-4TR2-1.99×10-6T2R2
- Also, the following formula was used in converting the daily maximum temperature to be expressed in Fahrenheit to calculate the heat index and the calculated heat index to be expressed in celsius.
- °F=℃×9/5+32
- The location data of each weather station was verified from the annual weather report [23]. The mean of observed values at each measuring point were used as representative values for each city and province according to administrative district. Also, the mean of all observed values was used as a nationally representative value and used in analysis. By using location data from the weather stations, we computed the latitude information of each city and province. For the provinces, the latitudes of local government capitals were used as representative values.
- In order to obtain the threshold temperatures of each city and province and population groups as well as the rate of patient increase according to temperature at temperatures above the threshold temperature, a piecewise regression model was designed [17]. This model is a linear regression model, of which its regression coefficient differs from certain temperatures below and above. To find the point where the regression coefficient changes, we identified how goodness of fit of models changed according to a temperature change per 0.1℃ increment, using Akaike's information criterion (AIC) value, and set the point of inflection of the model with the smallest AIC value as the threshold temperature. Then, a log linear model that assumes Poisson distribution in temperatures above the threshold was used, and the regression coefficient was exponentiated to obtain relative risks (RR).
- Among temperature indicators such as daily maximum temperature, daily average temperature, and heat index, each piecewise linear regression model using each indicator were compared to each other, in order to select the one that can best predict the incidence of patients with heat-related illnesses. The AIC and the explanatory power of each model were compared, and the temperature indicator used in the most suitable model was used in other analysis later. Using threshold temperatures and RRs in the temperatures above the threshold in various population groups, such as patients with heat-related illnesses across the nation and in regions including 16 cities and provinces, in different types of regions, of gender, age, and diagnosis, the characteristics of relationships with temperature were analyzed. Also, a chi squared test was used to analyze how patterns of occurrence of heat-related illnesses differed according to age, gender, and type of region.
- For statistical analysis, SPSS version 19.0 (IBM, Armonk, NY, USA) and R version 2.15 (The Comprehensive R Archive Network, http://cran.r-project.org) were used.
METHODS
- The number of patients with heat-related illnesses reported through the heat wave surveillance system for three months from June 1 to August 31 was 975 in total (Table 1). The patients' age ranged from 4 to 93, covering most age groups. Those who are 65 or older accounted for 32.5% of the total. By gender, men accounted for 69.4%, more than twice the percentage of women. By region, cases occurred in the provinces (66.6%) approximately twice as frequently as in the metropolitan cities (33.4%). And by location, cases occurred outdoors more than three times more frequently than indoors: 210 cases (21.5%) occurred indoors in homes, indoor workplaces, and other indoor places; 765 cases (78.5%) occurred outdoors, including outdoor workplaces, roads, fields and paddies, greenhouses, and other outdoor places.
- The percentage of patients with mild heat-related illnesses, including heat cramps, heat edema, and heat syncope was 28.5%; heat exhaustion, 39.2%, and heat stroke, 32.2%. Among all, 15 patients who were diagnosed with heat stroke died. Two hundred and fifty eight (24.2%) of them were hospitalized, and 86 among them were admitted to the intensive care unit. At the time of admission, the average body temperature of the patients was 37.7℃, and in one case, a patient peaked to 43.2℃. The blood pressure values of the patients were close to the normal range: the average systolic blood pressure was 125.25 mmHg and diastolic, 76.80 mmHg.
- Figure 2 shows the relationship between the overall incidence of heat-related illnesses and each temperature indicator. The threshold temperature when the daily maximum temperature was used was 31.2℃, and in temperatures above the threshold temperature, the RR per 1℃ temperature increase was 1.691 (95% confidence interval [CI], 1.641 to 1.743). In the model using the daily maximum heat index, the threshold temperature was 39.3℃, and in temperatures above the threshold temperature, the RR was 1.234 (95% CI, 1.218 to 1.250). In a model using the daily average temperature, the number of patients increased by 82.3% (95% CI, 1.756 to 1.892) per 1℃ increase in temperatures above 26.9℃. The model using the daily maximum temperature had the smallest AIC value of 535.13, demonstrating the highest goodness of fit. The explanatory power of the model was the highest (90.5%) as well.
- Therefore, in this paper, the association between the daily maximum temperature and variables such as age, gender, and diagnosis, as well as the incidence of patients with heat-related illnesses in 16 cities and provinces was analyzed. Then the threshold temperature of the daily maximum temperature and RRs in temperatures above the threshold temperature of the variables were compared (Table 2). The threshold temperature of males and females were similar to each other, at 31.1℃ and 31.6℃, respectively. However, the men's RR of the patient increase in temperatures above the threshold was 1.643 (95% CI, 1.587 to 1.701), lower than that of women, 1.822 (95% CI, 1.716 to 1.934). By age, the threshold temperatures of the group 19 or younger and the group 65 and older were similar to each other, at 31.3℃ and 31.8℃, respectively, whereas the threshold temperature of the 20- to 64-year-old group was lower (30.4℃). Among the RRs of the patient increase in temperatures above the threshold, that of the group 65 and older was 1.863 (95% CI, 1.755 to 1.978), higher than those of the other two groups. By diagnosis, the threshold temperatures of mild heat-related illnesses, heat exhaustion, and heat stroke were similar. The RR of heat stroke was 1.770 (95% CI, 1.674 to 1.872), which was somewhat higher than those of the other two illness groups.
- In terms of region, the threshold temperature was higher in the metropolitan cities (32.2℃) than in the provinces (30.5℃) by 1.7℃. The RRs of the metropolitan cities and provinces were similar, at 1.704 (95% CI, 1.618 to 1.794) and 1.687 (95% CI, 1.626 to 1.751), respectively. Among the metropolitan cities, Seoul and Daegu showed the highest threshold temperature. In those cities, at temperatures of 33.9℃ and above, the number of patients increased by 91.5% (95% CI, 1.751 to 2.094) and 58.3% (95% CI, 1.375 to 1.823), respectively, per 1℃ increase. Daejeon showed the lowest threshold temperature of 31.4℃, with an RR of 1.675 (95% CI, 1.434 to 1.957), and Ulsan had the lowest RR. In Ulsan, the number of patients increased by 32.9% (95% CI, 1.165 to 1.517) per 1℃ rise in temperatures above the threshold of 33.6℃. In terms of latitude, the RRs of Seoul and Incheon, the cities located in the Northern area, tended to be higher than in other regions. In the provinces, Chungnam showed the highest threshold temperature of 34.0℃, and Gangwon the lowest of 28.8℃. The RR was the highest in Gyeonggi and Jeju, at 1.799 (95% CI, 1.658 to 1.953) and 1.803 (95% CI, 1.375 to 2.364), respectively. Gangwon had the lowest RR among all of the provinces, with 1.527 (95% CI, 1.326 to 1.757).
- Table 3 demonstrates the pattern of heat-related illness according to gender, age, and region. Women had fewer cases of mild heat-related illness and a higher fraction of heat stroke than men, but such tendencies were not statistically significant. In relation to the pattern of heat-related illnesses, heat exhaustion was the most prevalent type among the 19 and younger group (50.0%) and the 20 to 64 group (45.3%). While heat stroke occurred at the similar incidence in these groups (25.0% and 26.0%, respectively), heat stroke was the most prevalent type in the group 65 and older (45.4%). By region, patterns of heat-related illnesses were similar between metropolitan cities and provinces.
RESULTS
- This study was conducted for the following purposes: to identify characteristics of patients who developed heat-related illnesses in the summer of 2012 in Korea; to analyze the relationship between the incidence of the illnesses with temperature; and to find threshold temperatures according to factors such as demographic characteristics and region, and RRs in temperatures above the threshold. Heat-related illnesses occurred more in men than in women and in provinces than in metropolitan cities. People 65 and older developed heat stroke more frequently than other age groups did. The threshold temperature was lower in the group of 20- to 64-year-olds than in the other age groups, and in provinces than in metropolitan cities. The RR at temperatures above the threshold temperature was higher in women than in men, and in the elderly aged 65 and up than in the younger age groups. In metropolitan cities, the RR generally tended to be higher with higher latitude. In terms of diagnosis, heat stroke showed the highest RR compared to the other types of illnesses.
- Previous studies conducted in Korea have demonstrated the association between total number of deaths or stroke and temperature and have discovered threshold temperatures. According to these studies, the threshold temperature of southern regions, such as Daegu, where the average temperature is high, was higher than that of Seoul or Incheon, where the latitude is higher and therefore the average temperature is relatively lower [4,6]. Nevertheless, in this study, which analyzed the data of patients with heat-related illnesses, the difference between Seoul and Daegu in threshold temperature was not high (0.7℃), and other regions did not show differences in the value according to latitude, either. Such differences have possibly originated from the difference in the mechanisms through which the health impacts are being influenced by temperature. In other words, while the total number of deaths rises in many cases due to indirect mechanisms such as exacerbation of cardiovascular diseases caused by the temperature rise, heat-related illnesses are mainly caused by direct exposure to high temperatures during outdoor activities [24]. Therefore, the threshold temperature of a demographic group related to an increase in heat-related illnesses is largely influenced by the pattern of activities of the group at high temperatures. This study demonstrated that the age group of 20 to 64 had the lowest threshold temperature of all of the age groups. This is thought to be due to the fact that the group engages in outdoor activities or economic activities more frequently than any other groups, and thus has more opportunities to be exposed to environments with high temperatures, and not necessarily because the group had a lower ability to adapt to high temperatures. Also, the finding that threshold temperatures in the provinces is lower than in metropolitan cities can imply that people in provinces, compared to their counterparts in metropolitan cities, are more likely to be easily exposed to high temperature. That is, they engage in outdoor activities more or work in conditions without air conditioning.
- At and above the threshold temperature, higher RRs signify a higher patient incidence according to temperature increase. Therefore, the RR reflects the sensitivity of heat-related illnesses to temperature. The findings of this study also demonstrated that the RRs of women and the age group of those 65 and older were higher than those of other groups. These groups are generally thought to have higher sensitivity to illnesses. The finding that the proportion of heat stroke was higher in those groups also appears to reflect that, as heat stroke is more severe than other heat-related illness. The RRs of heat-related illnesses to temperature can differ significantly by factors other than sex and age, such as the degree of adaptation to environments with high temperature by residents of each community, or the effectiveness of measures taken by local communities to adapt to high temperatures [25]. In this study, in a comparison between metropolitan cities, cities with higher latitude tended to have higher RR. This is considered to be due to the fact that residents in the metropolitan cities in the southern area are relatively more adapted to high temperatures.
- It can be said that the higher the threshold temperature, at which the number of patients starts to increase sharply, and the lower the RR, which represents the degree of the increase of patients, the less that health damages are caused by heat waves. The threshold temperature reflects the degree of exposure to high temperature and activity patterns of a demographic group. The RR is determined by the group's vulnerability and the group's degree of adaptation to high temperatures. Considering these facts, the following strategies may be needed: environments that expose a population group to high temperatures should be minimized in order to increase the threshold temperature; individuals' or communities' capacity to adapt to high temperatures should be increased to reduce their RRs to heat-related health damages.
- The threshold temperature can be used as a fundamental data point in making decisions related to investing resources and implementing policies to prevent health damages in a region or a population group, or in deciding when to issue a heat warning [26]. Also, the RR can be helpful in determining vulnerable groups. In this study, the rate of patient incidence increase according to the temperature rise was higher in women, compared to men, and in the elderly population. Such a trend can be changed by preventive action and management, not only by unmodifiable factors such as gender and age [27]. Therefore, preventive and management policies against heat-related illnesses can be evaluated based on RRs.
- The data on patents with heat-related illnesses used in this study were collected by the heat wave surveillance system of the KCDC. This system was implemented in 2011, in response to the ever-increasing possibility of heat wave occurrence. The system uses patients with heat-related illnesses as a monitoring indicator. While many countries across the world are operating surveillance systems for heat waves, various monitoring indicators are being utilized: total number of deaths, number of patients who visit emergency rooms, number of patients with heat-related illnesses, and others [20,28-30]. Nevertheless, in Korea, currently it is very difficult to establish a real-time mortality surveillance system. This is because a death is required to be reported within a month, and it takes approximately one year to establish official mortality statistics nationwide [31]. Mortality data reflects the overall damage of heat waves, and patterns of mortality and patients with heat-related illnesses at the time of a heat wave can vary. Thus, it is imperative for Korea to establish a mortality surveillance system in the future. In the meantime, the current surveillance system that monitors patients with heat-related illnesses is thought to have proven to be a useful surveillance system: It has highly sensitively demonstrated the relationship between temperature and the patient incidence during the summer of 2012, including the record high heat wave period, and the system accordingly induced the threshold temperatures and RRs.
- The limitations of this study are as follows. First, as a weakness of the surveillance system, the distribution of the participating institution with the surveillance system was not identical with that of all nationwide medical institutions. Because the representativeness of emergency medical institutions can differ by region and therefore can differ from the distribution of actual patient occurrence, it is difficult to compare the incidence rate by region. Nonetheless, such an inherent weakness of the surveillance system data may not be very significant. This is because the goal of this study was to identify and compare regional characteristics based on the threshold temperature and the rate of patient increase according to temperature, not on the incidence rate per region. Another limitation is that there is a possibility of underestimation, due to failure in patient reporting. There were personnel who were responsible for encouraging institutions to actively participate in this heat wave surveillance system. However, as the patient reporting was not mandatory, it is possible that reporting was not made when the workload in the emergency medical institutions was high.
- The strength of this study is that the accuracy of cases and diagnosis used in the study was very high because the data were collected by a national surveillance system. With definitions on the cases of patients and judgments made by professional medical staff, the accuracy of diagnosis was improved. Also, by excluding cases that occurred indoors or in workplaces, the relationship between the heat-related illnesses and outside temperature could be made more clearly.
- This study analyzed the relationship between temperature and heat-related illnesses occurring in the summer, including the heat wave period. It has identified threshold temperatures and RRs for the first time in Korea, and has interpreted their implications for public health. Heat-related illnesses occurring in Korea show the pattern of increasing drastically in temperatures at and above the threshold temperature. We have verified that threshold temperatures and the RRs of the patient incidence in temperatures above the threshold temperature can differ by the characteristics and location of the region, and patient characteristics such as gender and age. The findings of this study, the threshold temperature according to risk factors in 16 cities and provinces in the administrative districts, along with gender and age and RRs in temperatures above the threshold, should be used as critical information in implementing and evaluating heat-related illness preventive policies.
DISCUSSION
- 1. Bernstein L, Pachauri RK, Reisinger A. Intergovernmental Panel on Climate Change. Climate change 2007: synthesis report. 2008. Geneva: Intergovernmental Panel on Climate Change; p. 29-54
- 2. Bosch X. European heatwave causes misery and deaths. Lancet 2003;362(9383):543. 12932408ArticlePMC
- 3. Hajat S, Kovats RS, Atkinson RW, Haines A. Impact of hot temperatures on death in London: a time series approach. J Epidemiol Community Health 2002;56(5):367-372. 11964434ArticlePubMedPMC
- 4. Kim H, Ha JS, Park J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch Environ Occup Health 2006;61(6):265-270. 17967749ArticlePubMed
- 5. Cheng X, Su H. Effects of climatic temperature stress on cardiovascular diseases. Eur J Intern Med 2010;21(3):164-167. 20493415ArticlePubMed
- 6. Lim YH, Kim H, Hong YC. Variation in mortality of ischemic and hemorrhagic strokes in relation to high temperature. Int J Biometeorol 2013;57(1):145-153. 22527757ArticlePubMed
- 7. Page LA, Hajat S, Kovats RS, Howard LM. Temperature-related deaths in people with psychosis, dementia and substance misuse. Br J Psychiatry 2012;200(6):485-490. 22661680ArticlePubMed
- 8. Michelozzi P, Accetta G, De Sario M, D'Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 2009;179(5):383-389. 19060232ArticlePubMed
- 9. Blum LN, Bresolin LB, Williams MA. From the AMA Council on Scientific Affairs. Heat-related illness during extreme weather emergencies. JAMA 1998;279(19):1514. 9605881ArticlePubMed
- 10. Jardine DS. Heat illness and heat stroke. Pediatr Rev 2007;28(7):249-258. 17601937ArticlePubMed
- 11. Hausfater P, Doumenc B, Chopin S, Le Manach Y, Santin A, Dautheville S, et al. Elevation of cardiac troponin I during non-exertional heat-related illnesses in the context of a heatwave. Crit Care 2010;14(3):R99. 20507603ArticlePubMedPMC
- 12. Maher HK. Preventing heat-related illness. AAOHN J 2007;55(9):388. 17896653ArticlePubMedPDF
- 13. Rahmstorf S, Coumou D. Increase of extreme events in a warming world. Proc Natl Acad Sci U S A 2011;108(44):17905-17909. 22025683ArticlePubMedPMC
- 14. Dessai S. Heat stress and mortality in Lisbon Part II. An assessment of the potential impacts of climate change. Int J Biometeorol 2003;48(1):37-44. 12750971ArticlePubMed
- 15. Williams S, Nitschke M, Sullivan T, Tucker GR, Weinstein P, Pisaniello DL, et al. Heat and health in Adelaide, South Australia: assessment of heat thresholds and temperature relationships. Sci Total Environ 2012;414: 126-133. 22169392ArticlePubMed
- 16. Williams S, Nitschke M, Weinstein P, Pisaniello DL, Parton KA, Bi P. The impact of summer temperatures and heatwaves on mortality and morbidity in Perth, Australia 1994-2008. Environ Int 2012;40: 33-38. 22280925ArticlePubMed
- 17. Muggeo VM. Estimating regression models with unknown break-points. Stat Med 2003;22(19):3055-3071. 12973787ArticlePubMed
- 18. Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 2002;155(1):80-87. 11772788ArticlePubMed
- 19. Morabito M, Profili F, Crisci A, Francesconi P, Gensini GF, Orlandini S. Heat-related mortality in the Florentine area (Italy) beand after the exceptional 2003 heat wave in Europe: an improved public health response? Int J Biometeorol 2012;56(5):801-810. 21822792ArticlePubMed
- 20. Rhea S, Ising A, Fleischauer AT, Deyneka L, Vaughan-Batten H, Waller A. Using near real-time morbidity data to identify heat-related illness prevention strategies in North Carolina. J Community Health 2012;37(2):495-500. 21882040ArticlePubMed
- 21. Korea Meteorological Administration. Daily meteorological data. cited 2013 Jan 2. Available from: http://www.kma.go.kr/weather/observation/past_cal.jsp (Korean)
- 22. Rothfusz LP. The heat index "equation" or more than you ever wanted to know about heat index: National Weather Service Southern Region technical attachment SR/SSD 90-23. 1990. Fort Worth: National Weather Service; p. 1-2
- 23. Korea Meteorological Administrationation. Annual climatological report. 2011. cited 2013 Jan 2. Available from: http://www.kma.go.kr/repositary/sfc/pdf/sfc_ann_2011.pdf (Korean)
- 24. Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, Rubin CH. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Health 2007;97(Suppl 1):S158-S162. 17413056ArticlePubMedPMC
- 25. Taylor NA. Challenges to temperature regulation when working in hot environments. Ind Health 2006;44(3):331-344. 16922177ArticlePubMed
- 26. Lowe D, Ebi KL, Forsberg B. Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. Int J Environ Res Public Health 2011;8(12):4623-4648. 22408593ArticlePubMedPMC
- 27. Carson C, Hajat S, Armstrong B, Wilkinson P. Declining vulnerability to temperature-related mortality in London over the 20th century. Am J Epidemiol 2006;164(1):77-84. 16624968ArticlePubMed
- 28. Josseran L, Fouillet A, Caillère N, Brun-Ney D, Ilef D, Brucker G, et al. Assessment of a syndromic surveillance system based on morbidity data: results from the Oscour network during a heat wave. PLoS One 2010;5(8):e11984. 20711252ArticlePubMedPMC
- 29. Nogueira PJ, Machado A, Rodrigues E, Nunes B, Sousa L, Jacinto M, et al. The new automated daily mortality surveillance system in Portugal. Euro Surveill 2010;15(13):pii: 19529Article
- 30. Green HK, Andrews NJ, Bickler G, Pebody RG. Rapid estimation of excess mortality: nowcasting during the heatwave alert in England and Wales in June 2011. J Epidemiol Community Health 2012;66(10):866-868. 22766783ArticlePubMedPMC
- 31. Ministry of Health and Welfare. A study for improving the accuracy of cause-of-death statisitics. 2006. Seoul: Ministry of Health and Welfare; p. 271-283 (Korean)
REFERENCES
Figure 1Average daily maximum temperature (℃) during the surveillance period (June 1, 2012 to August 31, 2012). 1Heat wave period: July 22 to August 11, 2012.
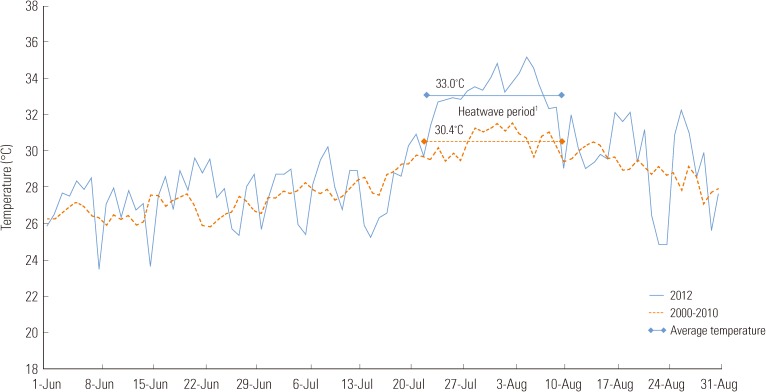
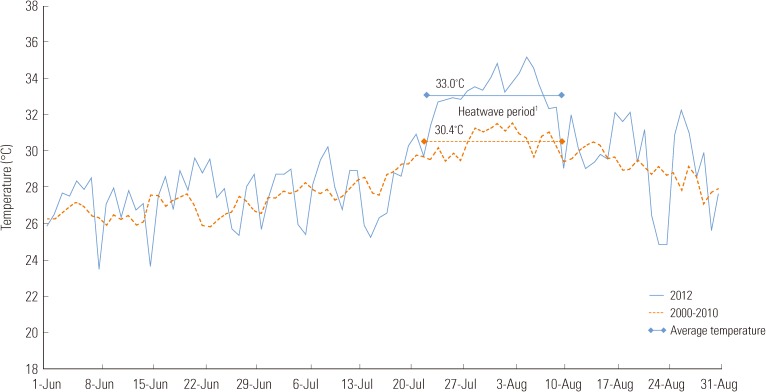
Figure 2Scatter plots and graphs of piecewise linear model of number of total heat-related patients according to several temperature indices (A, maximum temperature [℃]; B, maximum heat index [℃]; and C, average temperature [℃]) and threshold temperature (℃). RR, relative risk; CI, confidence interval; AIC, Akaike's information criterion.


Table 1.General characteristics of heat-related patients (n=975)
| n (%) | Mean | Minimum | Maximum | SD | ||
|---|---|---|---|---|---|---|
| Age (y) | Total | 975 (100) | 52.24 | 4 | 93 | 20.929 |
| 0-19 | 80 (8.2) | 14.68 | 4 | 19 | 3.628 | |
| 20-64 | 578 (59.3) | 44.45 | 20 | 64 | 12.094 | |
| 65- | 317 (32.5) | 75.91 | 65 | 93 | 7.023 | |
| Gender | Men | 676 (69.3) | - | - | - | - |
| Women | 299 (30.7) | - | - | - | - | |
| Region | Metropolitan cities1 | 326 (33.4) | - | - | - | - |
| Provinces2 | 649 (66.6) | - | - | - | - | |
| Location | Home | 99 (10.2) | - | - | - | - |
| Workplace-indoor | 74 (7.6) | - | - | - | - | |
| Workplace-outdoor | 219 (22.5) | - | - | - | - | |
| Road | 151 (15.5) | - | - | - | - | |
| Fields and paddies | 151 (15.5) | - | - | - | - | |
| Greenhouse | 16 (1.6) | - | - | - | - | |
| Other-indoors | 37 (3.8) | - | - | - | - | |
| Other-outdoors | 228 (23.4) | - | - | - | - | |
| Heat cramp | 123 (12.6) | - | - | - | - | |
| Diagnosis | Heat edema | 2 (0.2) | - | - | - | - |
| Heat syncope | 50 (15.4) | - | - | - | - | |
| Heat exhaustion | 386 (39.6) | - | - | - | - | |
| Heat stroke | 314 (32.2) | - | - | - | - | |
| Death | 15 (1.5) | - | - | - | - | |
| Outcome | Admission (ICU) | 86 (8.8) | - | - | - | - |
| Admission (general ward) | 171 (17.5) | - | - | - | - | |
| Transferred | 46 (4.7) | - | - | - | - | |
| Discharged | 654 (67.1) | - | - | - | - | |
| Discharged with-out treatment | 3 (0.3) | - | - | - | - | |
| Body temperature (°C) | 37.67 | 34.9 | 43.2 | 1.655 | ||
| Systolic blood pressure (mmHg) | 125.25 | 40 | 214 | 24.761 | ||
| Diastolic blood pressure (mmHg) | 76.80 | 28 | 160 | 15.602 | ||
Table 2.Threshold temperature (°C) and relative risk of heat-related illness associated with 1°C increment of maximum temperature above threshold according to gender, age, diagnosis, and region
| Latitude1 | Threshold (°C) | RR | 95% CI | p-value | |
|---|---|---|---|---|---|
| Gender | |||||
| Men | - | 31.1 | 1.643 | 1.587, 1.701 | <0.001 |
| Women | - | 31.6 | 1.822 | 1.716, 1.934 | <0.001 |
| Age (y) | |||||
| 0-19 | - | 31.3 | 1.590 | 1.442, 1.753 | <0.001 |
| 20-64 | - | 30.7 | 1.627 | 1.568, 1.689 | <0.001 |
| 65- | - | 31.8 | 1.863 | 1.755, 1.978 | <0.001 |
| Heat-related illness | |||||
| Mild2 | - | 31.2 | 1.647 | 1.559, 1.740 | <0.001 |
| Heat exhaustion | - | 31.1 | 1.666 | 1.589, 1.746 | <0.001 |
| Heat stroke | - | 31.3 | 1.770 | 1.674, 1.872 | <0.001 |
| Metropolitan cities | 32.2 | 1.704 | 1.618, 1.794 | <0.001 | |
| Seoul | 37˚34´ | 33.9 | 1.915 | 1.751, 2.094 | <0.001 |
| Incheon | 37˚28´ | 33.8 | 1.725 | 1.500, 1.984 | <0.001 |
| Daejeon | 36˚22´ | 31.4 | 1.675 | 1.434, 1.957 | <0.001 |
| Daegu | 35˚53´ | 33.9 | 1.583 | 1.375, 1.823 | <0.001 |
| Ulsan | 35˚33´ | 33.6 | 1.329 | 1.165, 1.517 | <0.001 |
| Gwangju | 35˚10´ | 32.8 | 1.531 | 1.336, 1.754 | <0.001 |
| Busan | 35˚06´ | 33.1 | 1.610 | 1.381, 1.876 | <0.001 |
| Provinces | 30.5 | 1.687 | 1.626, 1.751 | <0.001 | |
| Gangwon | 37˚54´ | 28.8 | 1.527 | 1.326, 1.757 | <0.001 |
| Gyeonggi | 37˚16´ | 31.9 | 1.799 | 1.658, 1.953 | <0.001 |
| Chungbuk | 36˚38´ | 30.9 | 1.655 | 1.470, 1.863 | <0.001 |
| Chungnam | 36˚22´ | 34.0 | 1.706 | 1.552, 1.876 | <0.001 |
| Gyeongbuk | 35˚53´ | 31.4 | 1.663 | 1.483, 1.865 | <0.001 |
| Jeonbuk | 35˚49´ | 31.8 | 1.672 | 1.476, 1.894 | <0.001 |
| Gyeongnam | 35˚10´ | 31.3 | 1.678 | 1.496, 1.883 | <0.001 |
| Jeonnam | 35˚10´ | 30.0 | 1.698 | 1.569, 1.837 | <0.001 |
| Jeju | 33˚30´ | 29.6 | 1.803 | 1.375, 2.364 | <0.001 |
Table 3.Number of patients with heat-related illnesses according to gender, age, and region
| Variables | No. of cases of mild heat- related illnesses (%) | No. of cases of heat exhaustion (%) | No. of cases of heat stroke (%) | p-value1 |
|---|---|---|---|---|
| Gender | ||||
| Men | 200 (29.6) | 272 (40.2) | 204 (30.2) | 0.10 |
| Women | 75 (25.1) | 114 (38.1) | 110 (36.8) | |
| Age (y) | ||||
| 0-19 | 20 (25.0) | 40 (50.0) | 20 (25.0) | <0.001 |
| 20-64 | 166 (28.7) | 262 (45.3) | 150 (26.0) | |
| 65- | 89 (28.1) | 84 (26.5) | 144 (45.4) | |
| Region | ||||
| Metropolitan cities2 | 87 (26.7) | 111 (34.0) | 128 (39.3) | 0.63 |
| Provinces3 | 188 (29.0) | 203 (31.3) | 258 (39.8) |
Figure & Data
References
Citations
Citations to this article as recorded by 

- Adaptation behaviors modify the effects of body fat on heat-related symptoms among Taiwanese elderly
Chi-Hsien Chen, Wen-Yi Lin, Kang-Yun Lee, Wen-Jung Sun, Li-Ying Huang, Yue-Liang Leon Guo
International Journal of Hygiene and Environmental Health.2024; 255: 114296. CrossRef - Analysis of Urban Heat Island Effect, Heat Stress and Public Health in Colombo, Sri Lanka and Shenzhen, China
Srimalee Nanayakkara, Weimin Wang, Jie Cao, Jia Wang, Weiqi Zhou
Atmosphere.2023; 14(5): 839. CrossRef - Outdoor Microclimate in Courtyard Buildings: Impact of Building Perimeter Configuration and Tree Density
Lia Marchi, Jacopo Gaspari, Kristian Fabbri
Buildings.2023; 13(11): 2687. CrossRef - Real-World Evidence for the Association between Heat-Related Illness and the Risk of Psychiatric Disorders in Taiwan
Fang-Ling Li, Wu-Chien Chien, Chi-Hsiang Chung, Chung-Yu Lai, Nian-Sheng Tzeng
International Journal of Environmental Research and Public Health.2022; 19(13): 8087. CrossRef - Heat Exposure, Heat-Related Symptoms and Coping Strategies among Elderly Residents of Urban Slums and Rural Vilages in West Bengal, India
Barun Mukhopadhyay, Charles A. Weitz
International Journal of Environmental Research and Public Health.2022; 19(19): 12446. CrossRef - The Development of New Generation of Manikin for Outdoor Thermal Comfort Evaluation – A Literature Review
R Kelundapyan, M A Zakaria, V C Segaran
IOP Conference Series: Materials Science and Engineering.2021; 1144(1): 012026. CrossRef - Probabilistic Heat Wave Forecast Based on a Large-Scale Circulation Pattern Using the TIGGE Data
Hyun-Ju Lee, Woo-Seop Lee, Jong Ahn Chun, Hwa Woon Lee
Weather and Forecasting.2020; 35(2): 367. CrossRef - Research Trends in Agenda-setting for Climate Change Adaptation Policy in the Public Health Sector in Korea
Su-Mi Chae, Daeeun Kim
Journal of Preventive Medicine and Public Health.2020; 53(1): 3. CrossRef - Risk of heat illness in men and women: A systematic review and meta-analysis
Robert M. Gifford, T. Todisco, M. Stacey, T. Fujisawa, M. Allerhand, D.R. Woods, R.M. Reynolds
Environmental Research.2019; 171: 24. CrossRef - Fuzzy comprehensive evaluation of human physiological state in indoor high temperature environments
Guozhong Zheng, Ke Li, Wentao Bu, Yajing Wang
Building and Environment.2019; 150: 108. CrossRef - The Effects of High-Temperature Weather on Human Sleep Quality and Appetite
Guozhong Zheng, Ke Li, Yajing Wang
International Journal of Environmental Research and Public Health.2019; 16(2): 270. CrossRef - Tens of thousands additional deaths annually in cities of China between 1.5 °C and 2.0 °C warming
Yanjun Wang, Anqian Wang, Jianqing Zhai, Hui Tao, Tong Jiang, Buda Su, Jun Yang, Guojie Wang, Qiyong Liu, Chao Gao, Zbigniew W. Kundzewicz, Mingjin Zhan, Zhiqiang Feng, Thomas Fischer
Nature Communications.2019;[Epub] CrossRef - Estimation of heat-related deaths during heat wave episodes in South Korea (2006–2017)
Youn-Hee Lim, Kyung-Shin Lee, Hyun-Joo Bae, Dowoo Kim, Hyosoon Yoo, Sungwoo Park, Yun-Chul Hong
International Journal of Biometeorology.2019; 63(12): 1621. CrossRef - Thermal discomfort analysis using UTCI and MEMI (PET and PMV) in outdoor environments: case study of two climates in Iran (Arak & Bandar Abbas)
Mehdi Asghari, Gholamheidar Teimori, Marzieh Abbasinia, Fahimeh Shakeri, Reza Tajik, Mohammad Javad Ghannadzadeh, Gholamabbas Fallah Ghalhari
Weather.2019;[Epub] CrossRef - Anthropometry-based estimation of body heat capacity in individuals aged 7–69 years: the Size Korea Survey 2010
Duong Duc Pham, Jeong Hoon Lee, Ka Yul Kim, Ji Yeon Song, Ji Eun Kim, Chae Hun Leem
Scientific Reports.2018;[Epub] CrossRef - Effect of Socioeconomic Status and Underlying Disease on the Association between Ambient Temperature and Ischemic Stroke
Seong-Kyung Cho, Jungwoo Sohn, Jaelim Cho, Juhwan Noh, Kyoung Hwa Ha, Yoon Jung Choi, Sangjoon Pae, Changsoo Kim, Dong Chun Shin
Yonsei Medical Journal.2018; 59(5): 686. CrossRef - Heatwave and health impact research: A global review
Sharon Campbell, Tomas A. Remenyi, Christopher J. White, Fay H. Johnston
Health & Place.2018; 53: 210. CrossRef - Short-term effect of heat waves on hospital admissions in Madrid: Analysis by gender and comparision with previous findings
J. Díaz, I.A. López, R. Carmona, I.J. Mirón, M.Y. Luna, C. Linares
Environmental Pollution.2018; 243: 1648. CrossRef - Factors affecting heat-related diseases in outdoor workers exposed to extreme heat
Jungsun Park, Yangho Kim, Inbo Oh
Annals of Occupational and Environmental Medicine.2017;[Epub] CrossRef - Current and Projected Burden of Disease From High Ambient Temperature in Korea
Soo Eun Chung, Hae-Kwan Cheong, Jae-Hyun Park, Jong-Hun Kim, Hyunjin Han
Epidemiology.2017; 28: S98. CrossRef - Heat-related illness in China, summer of 2013
Shaohua Gu, Cunrui Huang, Li Bai, Cordia Chu, Qiyong Liu
International Journal of Biometeorology.2016; 60(1): 131. CrossRef - A spatial analysis of heat stress related emergency room visits in rural Southern Ontario during heat waves
Katherine E. Bishop-Williams, Olaf Berke, David L. Pearl, David F. Kelton
BMC Emergency Medicine.2015;[Epub] CrossRef - Body temperature regulation: Sasang typology-based perspective
Duong Duc Pham, Chae Hun Leem
Integrative Medicine Research.2015; 4(4): 189. CrossRef - Hot Spot: Impact of July 2011 Heat Wave in Southern Italy (Apulia) on Cardiovascular Disease Assessed by Emergency Medical Service and Telemedicine Support
Natale Daniele Brunetti, Daniele Amoruso, Luisa De Gennaro, Giulia Dellegrottaglie, Giuseppe Di Giuseppe, Gianfranco Antonelli, Matteo Di Biase
Telemedicine and e-Health.2014; 20(3): 272. CrossRef - The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011–2013
Li Bai, Gangqiang Ding, Shaohua Gu, Peng Bi, Buda Su, Dahe Qin, Guozhang Xu, Qiyong Liu
Environmental Research.2014; 132: 212. CrossRef - Emergency Department Visits for Heat Stroke in the United States, 2009 and 2010
Xian Wu, Joanne E Brady, Henry Rosenberg, Guohua Li
Injury Epidemiology.2014;[Epub] CrossRef - The effect of pre-existing medical conditions on heat stroke during hot weather in South Korea
Si-Heon Kim, Soo-Nam Jo, Hyung-Nam Myung, Jae-Yeon Jang
Environmental Research.2014; 133: 246. CrossRef - Short-Term Effect of Temperature on Daily Emergency Visits for Acute Myocardial Infarction with Threshold Temperatures
Suji Lee, Eunil Lee, Man Sik Park, Bo Yeon Kwon, Hana Kim, Dea Ho Jung, Kyung Hee Jo, Myung Ho Jeong, Seung-Woon Rha, Qinghua Sun
PLoS ONE.2014; 9(4): e94070. CrossRef - An investigation into future performance and overheating risks in Passivhaus dwellings
Robert S. McLeod, Christina J. Hopfe, Alan Kwan
Building and Environment.2013; 70: 189. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite