Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(6); 2023 > Article
-
Original Article
Risks for Readmission Among Older Patients With Chronic Obstructive Pulmonary Disease: An Analysis Using Korean National Health Insurance Service – Senior Cohort Data -
Yu Seong Hwang
 , Heui Sug Jo
, Heui Sug Jo
-
Journal of Preventive Medicine and Public Health 2023;56(6):563-572.
DOI: https://doi.org/10.3961/jpmph.23.346
Published online: November 10, 2023
- 1,113 Views
- 64 Download
Department of Health Policy and Management, Kangwon National University School of Medicine, Chuncheon, Korea
- Corresponding author: Heui Sug Jo, Department of Health Policy and Management, Kangwon National University School of Medicine, 1 Kangwondaehak-gil, Chuncheon 24341, Korea E-mail: joheuisug@gmail.com
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- The high readmission rate of patients with chronic obstructive pulmonary disease (COPD) has led to the worldwide establishment of proactive measures for identifying and mitigating readmissions. This study aimed to identify factors associated with readmission, as well as groups particularly vulnerable to readmission that require transitional care services.
-
Methods
- To apply transitional care services that are compatible with Korea’s circumstances, targeted groups that are particularly vulnerable to readmission should be identified. Therefore, using the National Health Insurance Service’s Senior Cohort database, we analyzed data from 4874 patients who were first hospitalized with COPD from 2009 to 2019 to define and analyze readmissions within 30 days after discharge. Logistic regression analysis was performed to determine factors correlated with readmission within 30 days.
-
Results
- The likelihood of readmission was associated with older age (for individuals in their 80s vs. those in their 50s: odds ratio [OR], 1.59; 95% confidence interval [CI], 1.19 to 2.12), medical insurance type (for workplace subscribers vs. local subscribers: OR, 0.84; 95% CI, 0.72 to 0.99), type of hospital (those with 300 beds or more vs. fewer beds: OR, 0.77; 95% CI, 0.66 to 0.90), and healthcare organization location (provincial areas vs. the capital area: OR, 1.66; 95% CI, 1.14 to 2.41).
-
Conclusions
- Older patients, patients holding a local subscriber insurance qualification, individuals admitted to hospitals with fewer than 300 beds, and those admitted to provincial hospitals are suggested to be higher-priority for transitional care services.
- Chronic obstructive pulmonary disease (COPD) is highly prevalent worldwide, affecting approximately 12% of the population [1]. It is the third-ranking cause of death globally [2]. In Korea, COPD has a 10.8% prevalence rate, and it is the ninth leading cause of death [3].
- COPD is a chronic and irreversible condition characterized by damage to the airways and lung tissue, resulting in limited airflow [4]. Given its nature, ongoing management is necessary after diagnosis [5]. Failing to manage symptoms consistently can lead to avoidable hospitalizations and frequent readmissions. Readmissions are defined as subsequent admissions to the same or different hospitals within 30 days of discharge [6]. A higher readmission rate is associated with higher mortality rates [7] and lower quality of life for patients and their families [8].
- Compared to other diseases, COPD has notably high readmission rates. International studies indicate that approximately 20-23% of COPD patients are readmitted within 1 month, 39% within 3 months, and 79% within 2 years [9]. In Korea, the risk-standardized readmission rate for COPD is 12.7%, the highest among the evaluated disease groups [10]. Notably, the “avoidable” hospitalization or readmission rate for COPD patients in Korea exceeds the average rate among Organization for Economic Cooperation and Development countries [11].
- Internationally, proactive measures are already being implemented to identify and mitigate readmissions. In the United States, the Hospital Readmissions Reduction Program (HRRP) aims to minimize avoidable readmissions by imposing a 3% reduction in insurance reimbursement on providers that exceeded the predicted readmission levels, based on the average values for the last 3 years [12]. In the United Kingdom, emergency readmissions within 30 days of hospital discharge are analyzed to identify regional variations in readmission levels [13]. Similarly, in Canada, readmission rates within 30 days of discharge are monitored by the Canadian Institute for Health Information (CIHI) [14].
- In order to reduce the likelihood of hospital readmission, transitional care services are a viable option. These services provide a range of support and interventions for individuals transitioning from one healthcare setting, typically a hospital, to another, such as post-acute or home-based care [15]. They encompass essential components, including medication management, care coordination, patient education, and follow-up care. Though transitional care services in Korea have not been systematically established, 2 pilot projects are underway. Given the substantial disease burden in older adult patients with COPD, establishing a post-discharge patient management plan is essential to reduce COPD readmissions in older patients.
- Identifying characteristics of older adult COPD patients vulnerable to readmission is essential for prioritizing transitional care services. A few comprehensive analytical studies on this topic have been conducted in Korea. For instance, Kim et al. [16] analyzed factors associated with the COPD readmission rate using the National Health Insurance Service Senior Cohort (NHIS-SC) database and found that sex, institution type, insurance type, length of study, residential area, and medical service accessibility were associated with higher readmission rates. However, the study was limited in not specifying initial hospitalization because it did not consider patients’ medical history. In addition, it did not include the underlying disease or initial hospitalization route.
- To address this gap, this cross-sectional study based on NHIS-SC data aimed to identify factors associated with readmissions of older COPD patients at 3 levels: socio-demographic, healthcare organization, and each individual’s underlying disease.
INTRODUCTION
- Data Sources
- This retrospective cohort study analyzed data from version 2.0 of the NHIS-SC database. The database contains representative cohort data on 8% of the population selected through simple random sampling. It focuses on individuals aged ≥60 years who had maintained their health insurance and medical benefit qualifications as of 2008 [17]. Each year since 2009, new records are added for individuals turning 60 years old, together with 10 years’ worth of their medical records [17]. Consequently, the analysis included patients in their 50s as well.
- Study Population
- The participants in this study consisted of patients aged 50 years or older who were hospitalized for the first time with COPD as their main diagnosis between 2009 and 2019. According to the Korean Standard Classification of Disease version 7.0, codes J43 and J44 indicate COPD patients [18]. To simplify the analysis, patients with a prior COPD primary diagnosis in 2007 or 2008 were excluded, since the first hospitalization for COPD was presumed to occur during the study’s cohort period.
- Definition of Readmission
- In our model, the dependent variable was the 30-day all-cause readmission rate. This aligns with the approach used by the HRRP in the United States and the CIHI in Canada, both of which consider all-cause readmissions in their analyses of factors associated with COPD readmissions [6,14].
- Billing for stays exceeding 1 month was assessed monthly, and because of the nature of the claims data, there were records of transfers to other hospitals or consultations with other departments during hospitalization. As a result, clear operational definitions were necessary to determine readmissions. We considered cases to have a single hospitalization if they met all 3 of the following conditions: (1) the readmission occurred 1 day or less after discharge, (2) the same healthcare institution number was used, and (3) the same main diagnosis code was used. Patients were excluded if they had consultations with other departments during hospitalization, since the days of medication use were not recorded in such cases.
- Statistical Analysis
- A cross-sectional study based on a retrospective cohort database was conducted to analyze the associations among 30-day readmissions of COPD patients and risk factors associated with hospital readmission. A comprehensive systematic review of factors associated with COPD patient readmission worldwide classified the risk factors for readmission in COPD patients into 3 categories: (1) patient-related socioeconomic risk factors, (2) provider-related risk factors, and (3) patient-related clinical risk factors [19]. Based on these categories, our study established a 3-stage model using variables that can be extracted from the NHIS-SC database.
- Model 1 contained socio-demographic factors. Model 2 added healthcare organization factors to model 1, and model 3 added the underlying diseases of each patient to model 2. Socio-demographic factors representing biological characteristics such as age and sex, and conditions that could help or hinder utilization, such as residential area, insurance type, and income level, were included in model 1. Residential areas were categorized into distinct regions, namely the capital area (comprising Seoul and Gyeonggi Province), metropolitan cities, and provincial (do) areas. The insurance types were local subscriber, workplace subscriber, and Medical Aid beneficiary; local subscribers included self-employed individuals and the unemployed, excluding workplace subscribers and their dependents. Income levels were delineated into 6 distinct groups. The lowest income group included Medical Aid beneficiaries, while income levels 2 to 6 were defined based on insurance fee information.
- In model 2, the analysis was expanded to encompass additional variables, namely hospital type (defined by the bed capacity, i.e., more or fewer than 300 beds), admission route (emergency room or an outpatient visit), and the hospital site’s region type (capital area, metropolitan cities, and provincial areas). This augmented selection of variables was chosen to explore the efficacy of the initial hospitalization process. Preliminary studies have emphasized the effects of hospital-level characteristics on the readmission rates of COPD patients [20,21]. The route of initial admission was included as a proxy indicator for the severity of the patient’s COPD.
- Model 3 added components of each patient’s underlying disease. The underlying diseases comprised a total of 6 conditions, namely stroke, myocardial infarction, hypertension, diabetes, tuberculosis, and other diseases, which were elicited during the mandatory medical checkup. A systematic review concluded that “hospitalization in the previous year and comorbidity (asthma) were the most consistent predictors of exacerbation of COPD readmission,” highlighting the importance of the effects of the underlying disease [19].
- The univariate chi-square test was conducted to assess whether each indicator was evenly distributed based on patient characteristics. Logistic regression analysis was performed to determine whether the factors in the established model were significantly correlated with readmission within 30 days. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses. All reported p-values were 2-sided. Statistical significance was defined as p<0.05.
- Ethics Statement
- The study protocol was reviewed and approved by the Institutional Review Board of Kangwon University Hospital (approval No. KNUH-2023-02-003).
METHODS
- In total, 4874 patients were included in the analysis, of whom 1131 (23.2%) were readmitted within 30 days after hospital discharge (Table 1). Male participants outnumbered female participants by 3231 (66.3%), although the readmission rate of male participants (23.1%) was similar to that of female participants (23.4%). Regarding participant age, 398 (8.2%) were in their 50s, 1328 (27.2%) were in their 60s, 2062 (42.3%) were in their 70s, and 1074 (22%) were in their 80s. The readmission rate was higher among older participants. Regarding participants’ residential areas, 1109 (22.8%) lived in the capital area (Seoul and Gyeonggi Province), 999 (20.5%) lived in metropolitan cities, and 2766 (56.8%) lived in provincial (do) areas.
- Regarding health insurance type, 1382 participants (28.4%) were local subscribers, 3070 (63%) were workplace subscribers, and 422 (8.7%) were Medical Aid beneficiaries. The health insurance percentiles representing the first through sixth income levels included 532 (10.9%), 653 (13.4%), 560 (11.5%), 761 (15.6%), 920 (18.9%), and 1448 (29.7%) participants, respectively. The Medical Aid beneficiaries were included in the first percentile. At the time of their first hospitalization, 2830 (58.1%) and 2044 (41.9%) patients were admitted in healthcare organizations with fewer and more than 300 beds, respectively. Regarding the location of healthcare organizations, 1182 (24.3%) were in the capital area, 1232 (25.3%) in metropolitan cities, and 2460 (50.5%) in provincial areas.
- At the time of their first hospitalization, 3573 (73.3%) patients were admitted through outpatient visits and 1255 (25.7%) through emergency room visits. The participants’ underlying diseases were identified based on their previous medical examination records closest to the date of first hospitalization, which showed that 159 (3.3%) participants had stroke, 449 (9.2%) had heart failure, 1818 (37.3%) had hypertension, 708 (14.5%) had diabetes, 181 (3.7%) had pulmonary tuberculosis, and 1203 (24.7%) had other conditions.
- Table 2 summarizes the logistic regression analysis results for the factors associated with readmission across the 3 models. In model 1, among socio-demographic factors, readmission within 30 days showed a significant association with age and residential area. In model 2, among healthcare organization factors, readmission within 30 days had a significant association with type of hospital and hospital location. Moreover, the type of hospital and location were significantly associated with readmission. In model 3, the individual’s underlying disease had no significant association with readmission within 30 days.
- In model 1, among the socio-demographic factors, sex was not significantly associated with readmission within 30 days. However, older age was significantly associated with readmission within 30 days. Specifically, sex showed a weak correlation with readmission in model 3 (female: odds ratio [OR], 0.94; 95% confidence interval [CI], 0.81 to 1.09). Participants in their 80s or 90s were more likely to be admitted than those their 50s (model 3, 60s: OR, 0.97; 95% CI, 0.73 to 1.28; 70s: OR, 1.18; 95% CI, 0.90 to 1.54; 80s: OR, 1.59; 95% CI, 1.19 to 2.12; 90s: OR, 3.83; 95% CI, 1.17 to 12.50).
- In model 1, a participant’s residential area was associated with a higher readmission rate in provincial areas than in metropolitan cities (provincial areas: OR, 1.26; 95% CI, 1.06 to 1.49); however, it was not associated with readmission rates in models 2 or 3, which included the healthcare organization factors (model 3, metropolitan cities: OR, 0.87; 95% CI, 0.57 to 1.33; provincial areas: OR, 0.76; 95% CI, 0.53 to 1.11). In all models, workplace subscribers had lower readmission rates than local subscribers, while the readmission rates of local subscribers and Medical Aid beneficiaries did not differ (model 3, workplace subscribers: OR, 0.84; 95% CI, 0.72 to 0.99; Medical Aid beneficiaries: OR, 1.34; 95% CI, 0.80 to 2.26). Although income level was not significantly associated with readmission within 30 days, the OR for readmission within 30 days showed a U-shaped relationship with income level.
- The first hospitalization and type of hospital were significantly associated with early readmission in models 2 and 3, with the first hospitalization in a hospital with more than 300 beds likely to be associated with lower readmission rates (model 3, <300 beds: OR, 0.77; 95% CI, 0.66 to 0.90). Additionally, patients who were first hospitalized in an institution located in a provincial area were more likely to be readmitted than those admitted to an institution located in the capital area (model 3, metropolitan cities: OR, 1.39; 95% CI, 0.92 to 2.10; provincial areas: OR, 1.66; 95% CI, 1.14 to 2.41). Whether the first hospitalization was through an emergency room or an outpatient visit was irrelevant in models 2 and 3 (model 3, admission through an emergency room visit: OR, 1.11; 95% CI, 0.94 to 1.31).
- Participants’ underlying diseases were not significantly associated with readmissions (model 3, stroke: OR, 1.15; 95% CI, 0.79 to 1.65; heart failure: OR, 1.07; 95% CI, 0.85 to 1.35; hypertension: OR, 0.96; 95% CI, 0.83 to 1.11; diabetes: OR, 0.92; 95% CI, 0.75 to 1.13; tuberculosis: OR, 0.90; 95% CI, 0.62 to 1.31; other diseases: OR, 1.01; 95% CI, 0.87 to 1.19). Figure 1 shows forest plots for the association between readmission of COPD patients and risk factors.
RESULTS
- This study included 4874 patients hospitalized with COPD as their principal diagnosis between 2009 and 2019. This finding is consistent with that of a previous study, which reported a readmission rate of 22.6% for patients discharged with COPD within 30 days for various reasons [22]. The readmission rate in our study was higher than the risk-standardized readmission rate for COPD [10]. This discrepancy may be attributed to the fact that our analysis encompassed all healthcare organizations, whereas the previous study considered only general hospitals and upper-level general hospitals with 500 beds or more. The readmission rate of healthcare organizations with over 500 beds may be an underestimate, since our results indicated that hospitals with fewer than 300 beds had a higher readmission rate.
- When considering personal demographic factors, age emerged as a significant contributor to readmission, with older adults showing a higher susceptibility. This can be attributed to factors such as natural aging and the presence of other medical conditions that can impede recovery from COPD hospitalization. These factors can increase the risk of acute exacerbations and subsequent readmission. Therefore, physicians would tend to consider older COPD patients as having a higher risk of readmission.
- In addition, the insurance type showed significant association with readmission. Given that the mean age of the COPD patients in this study was higher than the average retirement age, it is probable that employed families, especially the older patients’ offspring, registered their parents. Korea’s national insurance system allows workers to register their family members with the same insurance status if they live together. Consequently, holding workplace insurance qualifications can imply that an elderly individual has family members who can offer care and immediate assistance. Notably, medical services are offered uniformly in Korea, irrespective of the insurance type. Therefore, the difference in readmission rates cannot be attributed to variations in service based on insurance coverage. Instead, the results may be attributed to variations in support from family caregivers, suggesting that patients lacking family support are more vulnerable to readmission. According to one study, caregiving is associated with lower readmission rates in patients with COPD [23]. Therefore, it is advisable to consider prioritizing transitional care services for patients who may not have access to ample caregiving support from their family members.
- Among the hospital-level characteristics examined in this study, hospital type and the initial admission location of patients were significantly correlated with readmission. Notably, patients admitted to hospitals with more than 300 beds had a lower likelihood of readmission. In this study, the number of beds was considered an indicator of the medical staff’s competency and the range of medical services offered, rather than just the size of the hospital. A prior study highlighted that the quality of medical and therapeutic services received during hospitalization and appropriate outpatient management could affect differences in readmission rates [24]. Furthermore, other studies tracking healthcare utilization by the same patients have suggested that disparities in healthcare facilities play a role, at least partially, in readmission rates independent of patient factors [25].
- Korean statistical data indicate that tertiary general hospitals and general hospitals have higher implementation rates of pulmonary function tests (PFTs), prescription rates of bronchodilators, and maintenance rates of PFT equipment compared to other types of hospitals and clinics [26]. Therefore, to address the need for reducing readmission rates in COPD patients, it is recommended that transitional care interventions, including initiatives such as providing education on home healthcare and implementing early post-discharge follow-up, along with other supportive measures [26,27], be implemented specifically within the context of smaller and medium-sized hospitals that have fewer than 300 beds.
- Furthermore, our analysis revealed that hospitalizations in provincial areas are followed by higher readmission rates compared to those in metropolitan areas and metropolitan city hospitals. When considering both patient residential area and hospital location in models 2 and 3, we found that only hospital location was significantly associated with readmission rates, which suggests that readmission rates are more strongly influenced by the latter. The result indicates that services provided by hospitals may vary by area. In metropolitan areas and large cities, primary healthcare and social welfare resources are more abundant [28], suggesting that the appropriate services for discharged patients can be readily available. Therefore, further studies should be conducted on the differences in patient support services by regional area.
- Finally, our analysis revealed that comorbidities were not significantly associated with readmission, which contrasts with the findings of previous research. Baker et al. [23] identified comorbid conditions as a significant predictor of readmission within 30 days after discharge, and another study found an association between readmission of COPD patients and comorbidities such as heart failure, renal failure, acute myocardial infarction, pneumonia, and depression [29]. Our analysis focused on patients who were initially diagnosed with COPD during their first hospitalization, which could explain why underlying diseases were not associated with readmission in our findings. Future studies that investigate individuals’ continuous healthcare utilization records to analyze comorbidities may offer a more comprehensive understanding of the impact of comorbidities on readmission.
- Limitations
- This study has certain limitations due to the use of secondary data for analysis. The severity of the underlying disease may not have been adequately captured because it relied on self-reported information from medical examinations. Consequently, detailed aspects such as the severity and duration of the illnesses were not available. The NHIS-SC data also did not contain medical usage records before the initial year of the cohort.
- In addition, there is a limitation in that it does not directly incorporate variables that consider community support, such as participants’ access to healthcare organizations, the number and distribution of medical facilities and healthcare professionals in the region, and the quality and availability of transportation and other social infrastructure. Instead, it relies on indirect variables such as the size and location of healthcare organizations.
- Furthermore, this study examined the factors influencing readmission of all causes, rather than specifically focusing on COPD-related readmission in patients initially hospitalized with COPD. This approach was taken because COPD is a systemic disease that can lead to various comorbid conditions [30], and our aim was to analyze relevant factors across demographics, healthcare organizations, and underlying diseases. Many previous studies used all-cause readmission within 30 days to identify readmission factors. However, further research that focuses on the irreversible prognosis of COPD could be beneficial in treatment of severe COPD patients.
- Nevertheless, the significance of this study lies in its process of defining and analyzing readmissions within 30 days after discharge using NHIS-SC data. This study comprehensively incorporated multiple aspects of healthcare service utilization. These findings enable us to identify higher-priority patient management groups that may require special attention during hospital discharge.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This research was supported by a grant from the Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (grant No. HC21C0171).
-
AUTHOR CONTRIBUTIONS
Both authors contributed equally to conceiving the study, analyzing the data, and writing this paper.
Notes
ACKNOWLEDGEMENTS
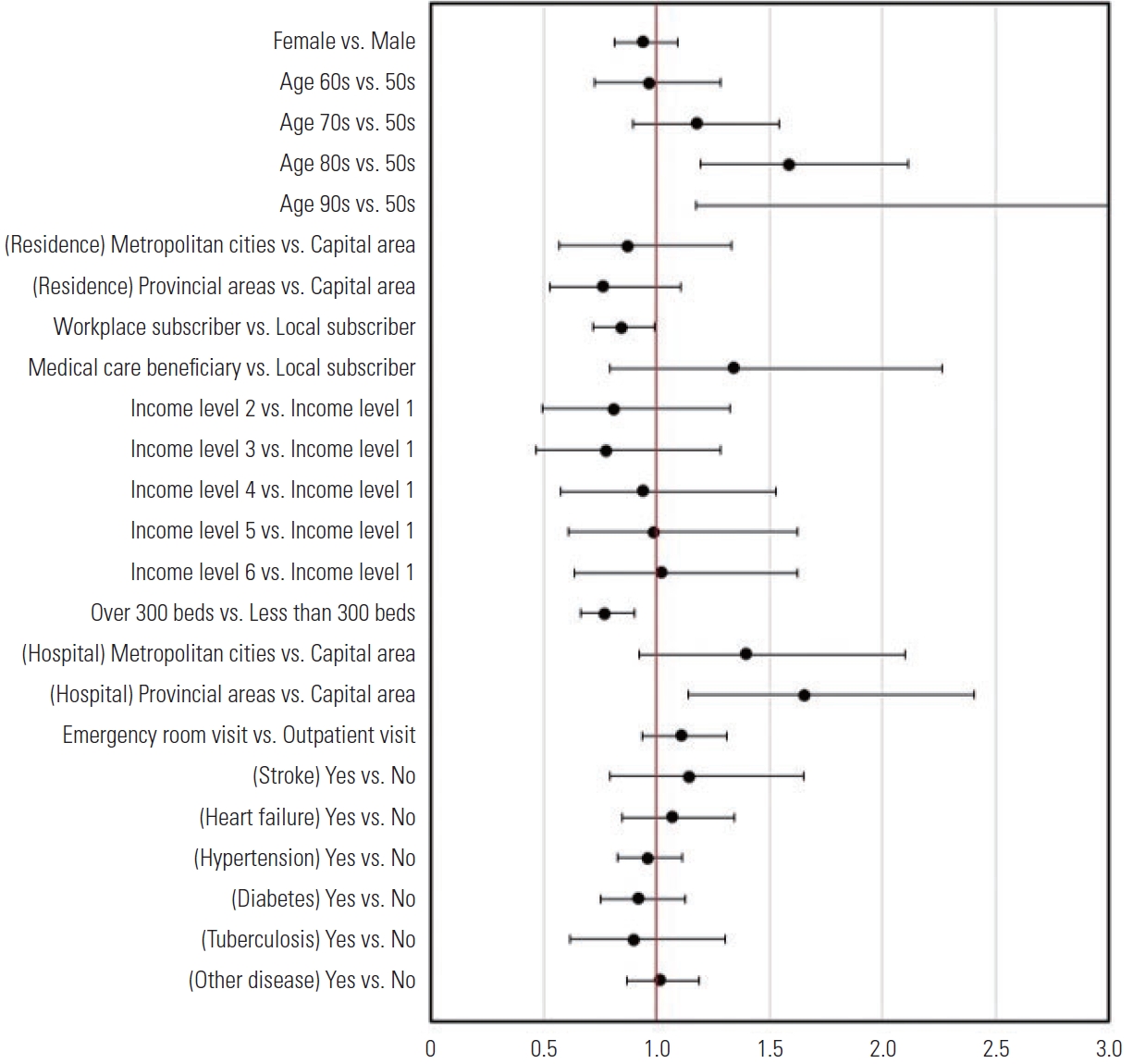
Values are presented as odds ratio (95% confidence interval).
1 Model I: only socio-demographic factors included; Model II: sociodemographic factors and healthcare organization factors included; Model III: socio-demographic factors, healthcare organization factors and underlying diseases variables included.
- 1. Varmaghani M, Dehghani M, Heidari E, Sharifi F, Moghaddam SS, Farzadfar F. Global prevalence of chronic obstructive pulmonary disease: systematic review and meta-analysis. East Mediterr Health J 2019;25(1):47-57ArticlePubMed
- 2. World Health Oraganization. Chronic obstructive pulmonary disease (COPD). 2023 [cited 2023 Feb 13]. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
- 3. Cho KS. Current status of chronic obstructive pulmonary disease (COPD) in the Republic of Korea. Public Health Wkly Rep 2021;14(16):943-951. (Korean)
- 4. Korean Academy of Tuberculosis and Respiratory Diseases. Practice guidelines: COPD guideline revised 2018 [cited 2022 Dec 13]. Available from: https://www.lungkorea.org/bbs/skin/guide/download.php?code=guide&number=10635 (Korean)
- 5. Bourbeau J, Saad N, Joubert A, Ouellet I, Drouin I, Lombardo C, et al. Making collaborative self-management successful in COPD patients with high disease burden. Respir Med 2013;107(7):1061-1065ArticlePubMed
- 6. Alqahtani JS, Njoku CM, Bereznicki B, Wimmer BC, Peterson GM, Kinsman L, et al. Risk factors for all-cause hospital readmission following exacerbation of COPD: a systematic review and meta-analysis. Eur Respir Rev 2020;29(156):190166ArticlePubMedPMC
- 7. Schoenbaum SC, Schoen C, Nicholson JL, Cantor JC. Mortality amenable to health care in United States: the roles of demographics and health systems performance. J Public Health Policy 2011;32(4):407-429PubMed
- 8. Almagro P, Barreiro B, Ochoa de Echaguen A, Quintana S, Rodríguez Carballeira M, Heredia J, et al. Risk factors for hospital readmission in patients with chronic obstructive pulmonary disease. Respiration 2006;73(3):311-317ArticlePubMedPDF
- 9. Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med 2000;160(8):1074-1081ArticlePubMed
- 10. Health Insurance Review and Assessment Service. The result of the risk-standardized readmission rate of 2017 (2nd). 2018 [cited 2023 Feb 13]. Available from: https://www.hira.or.kr/cms/open/04/04/12/2018_10.pdf (Korean)
- 11. Organization for Economic Cooperation and Development (OECD). OECD reviews of public health: Korea: a healthier tomorrow. 2020 [cited 2023 Feb 13]. Available from: https://www.oecd-ilibrary.org/sites/6e005d47-en/index.html?itemId=/content/component/6e005d47-en
- 12. Cox JC, Sadiraj V, Schnier KE, Sweeney JF. Incentivizing costeffective reductions in hospital readmission rates. J Econ Behav Organ 2016;131(B):24-35ArticlePubMedPMC
- 13. Nolte E, Roland M, Guthrie S, Brereton L. Preventing emergency readmissions to hospital: a scoping review. Rand Health Q 2012;2(1):10
- 14. Canadian Institute for Health Information. All-cause readmission to acute care and return to the emergency department. 2012 [cited 2023 Feb 13]. Available from: https://publications.gc.ca/collections/collection_2013/icis-cihi/H118-93-2012-eng.pdf
- 15. Naylor MD, Van Cleave J. Transitional care model. In: Meleis AI, editor. Transitions theory: middle-range and situation-specific theories in nursing research and practice. New York: Springer Publishing; 2012. p. 459-465
- 16. Kim TW, Choi ES, Kim WJ, Jo HS. The association with COPD readmission rate and access to medical institutions in elderly patients. Int J Chron Obstruct Pulmon Dis 2021;16: 1599-1606ArticlePubMedPMCPDF
- 17. National Health Insurance Sharing Service. Sample research DB [cited 2022 Dec 3]. Available from: http://nhiss.nhis.or.kr/bd/ab/bdaba022Oeng.do
- 18. Statistics Korea. Korean Standard Classification of Disease (KCD) version 7. 2015 [cited 2022 Jun 3]. Available from: http://kssc.kostat.go.kr/ksscNew_web/kssc/common/ClassificationContent.do?gubun=1&strCategoryNameCode=004&categoryMenu=007&addGubun=no (Korean)
- 19. Njoku CM, Alqahtani JS, Wimmer BC, Peterson GM, Kinsman L, Hurst JR, et al. Risk factors and associated outcomes of hospital readmission in COPD: a systematic review. Respir Med 2020;173: 105988ArticlePubMed
- 20. Press VG, Au DH, Bourbeau J, Dransfield MT, Gershon AS, Krishnan JA, et al. Reducing chronic obstructive pulmonary disease hospital readmissions. An official American Thoracic Society workshop report. Ann Am Thorac Soc 2019;16(2):161-170ArticlePubMedPMC
- 21. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med 2010;170(18):1664-1670ArticlePubMedPMC
- 22. Portillo EC, Wilcox A, Seckel E, Margolis A, Montgomery J, Balasubramanian P, et al. Reducing COPD readmission rates: using a COPD care service during care transitions. Fed Pract 2018;35(11):30-36
- 23. Baker CL, Zou KH, Su J. Risk assessment of readmissions following an initial COPD-related hospitalization. Int J Chron Obstruct Pulmon Dis 2013;8: 551-559PubMedPMC
- 24. Krumholz HM, Wang K, Lin Z, Dharmarajan K, Horwitz LI, Ross JS, et al. Hospital-readmission risk - isolating hospital effects from patient effects. N Engl J Med 2017;377(11):1055-1064ArticlePubMedPMC
- 25. Chung SM, Lee SY. Evaluation of appropriate management of chronic obstructive pulmonary disease in Korea: based on Health Insurance Review and Assessment Service (HIRA) claims. Tuberc Respir Dis (Seoul) 2017;80(3):241-246ArticlePubMedPMCPDF
- 26. Nantsupawat T, Limsuwat C, Nugent K. Factors affecting chronic obstructive pulmonary disease early rehospitalization. Chron Respir Dis 2012;9(2):93-98ArticlePubMedPDF
- 27. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med 2010;170(18):1664-1670ArticlePubMedPMC
- 28. Lee J. Urban-rural differences in intention to age in place while receiving home care srvices: findings from the National Survey of Older Koreans. Arch Gerontol Geriatr 2022;101: 104690PubMed
- 29. Rinne ST, Castaneda J, Lindenauer PK, Cleary PD, Paz HL, Gomez JL. Chronic obstructive pulmonary disease readmissions and other measures of hospital quality. Am J Respir Crit Care Med 2017;196(1):47-55ArticlePubMedPMC
- 30. Agusti A, Soriano JB. COPD as a systemic disease. COPD 2008;5(2):133-138ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


