Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(6); 2023 > Article
-
Original Article
The Trajectory of Depressive Symptoms Across Years of Community Care Utilization Among Older Adults: A 14-Year Follow-up Study Using the ‘Korean Welfare Panel Survey’ -
Il-Ho Kim1
 , Cheong-Seok Kim1,2
, Cheong-Seok Kim1,2 , Min-Hyeok Jeong3
, Min-Hyeok Jeong3
-
Journal of Preventive Medicine and Public Health 2023;56(6):495-503.
DOI: https://doi.org/10.3961/jpmph.23.022
Published online: October 6, 2023
- 1,031 Views
- 84 Download
1Center for Collaborative Research on Population and Society, Dongguk University, Seoul, Korea
2Department of Sociology, Dongguk University, Seoul, Korea
3Jason TG, Stata Korea, Seoul, Korea
- Corresponding author: Cheong-Seok Kim, Center for Collaborative Research on Population and Society, Dongguk University, 2 Toegye-ro 36-gil, Jung-gu, Seoul 04626, Korea E-mail: chkim108@hanmail.net
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- While older adults using community care services are known to be vulnerable for depression, community care utilization (CCU) may help to improve the mental health of these elderly. To date, however, it is much less clear how CCU affects depressive symptoms in the elderly population. This study focuses on the trajectory of depressive symptoms across years of CCU among older adults in Korea.
-
Methods
- Using the 2006-2019 Korean Welfare Panel Survey, this study is focused on elderly born in 1940 or earlier and selected 3281 persons for baseline interviews in 2006. This consisted of 35 800 person-year observations during a period of 14 years. Panel data analysis were employed to construct years of CCU.
-
Results
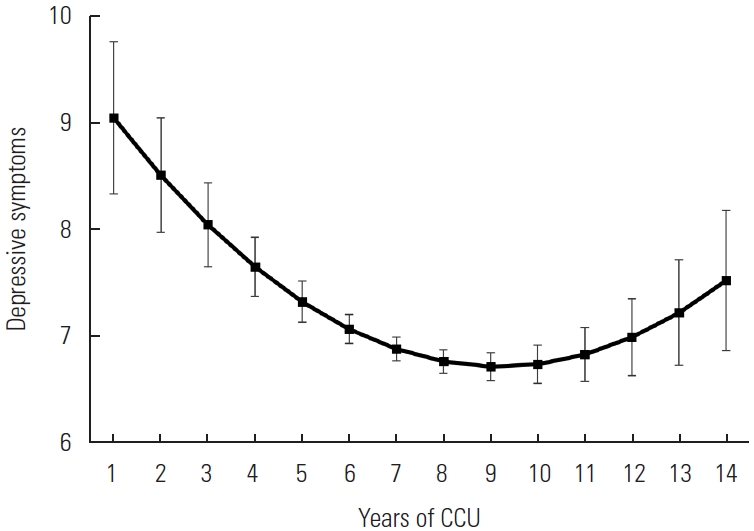
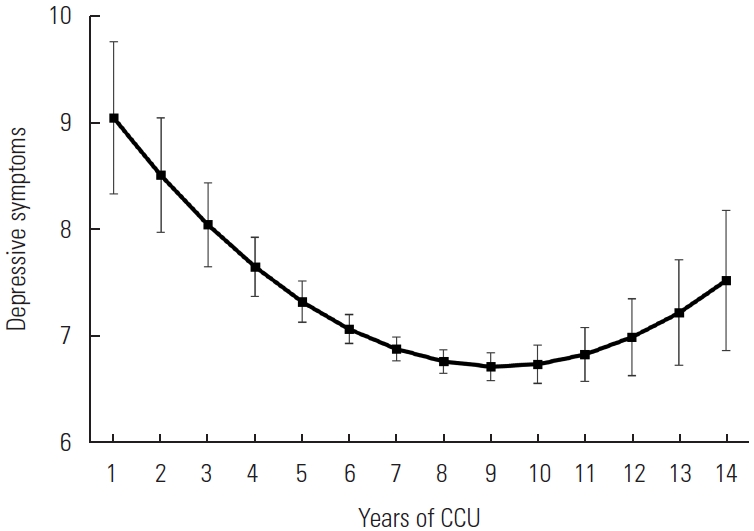
- After controlling for covariates, linear term of years using community care was negatively associated with depressive symptoms, but a quadratic term was positively significant. The trajectory of depressive symptoms across the years of CCU follows a U-shaped curve. Older adults in the first year of using community care reported the highest level of depressive symptoms. However, a significant and steady decrease in depressive symptoms was observed during the following 9 years of CCU, which then gradually increased. The level of depressive symptoms at the 14th year of using community care remains significantly lower than the level at the outset of its utilization.
-
Conclusions
- This finding implies that CCU could be beneficial for improving mental health among older adults.
- Depression is a significant public health problem for older adults using community care services. Accompanied by a growing number of severe chronic diseases, functional disabilities, and/or lack of social supports, older community care users are expected to bear distress from increasing levels of depression [1]. Adding to the challenges of facing serious illness, they could be susceptible to further stressors, such as loss of roles, disengagement from social activities, and social isolation, all of which hike up severe depressive symptoms [2]. Furthermore, the social stigma of viewing disabled older adults as incompetent and/or useless may lead them to experience high levels of depression [3,4]. In the past few decades, scientific research has confirmed that older community care users are vulnerable to depression worldwide [5-7]. According to research from the United States, the prevalence of depression among older community care users was 8.5%, which was a lot higher than the 2.7-4.7% among their counterparts [5]. Another nationally representative research suggested that approximately half of older community care users suffered from a high risk of depressive symptoms: 38.7% of them had subthreshold depression and 13.4% suffered from major depressive disorders [6]. Similar results were observed in the European and Korean research [7,8]. In Korea, a study showed that the prevalence of depressive symptoms was three times as high for community care users (32.1%) when compared to non-users (9.8%) [8]. Although these findings may feasibly appear to be intuitive and were endorsed by a good amount of community care research, recent research has refuted this argument regarding the role that community care services perform for older adults.
- It is commonly acknowledged that community care can be regarded as an effective policy in promoting psychological health for older adults. Community care was designed to help older adults maintain more independence and dignity in their homes whenever health and/or physical functions deteriorated [9]. It covers a wide range of community-based and home-based healthcare services (such as home-visit nursing and services), as well as social care services (i.e., housekeeping tasks, day/night care, companion care activities, and/or lifelong education, etc.). Older adults, in the initial years of community care utilization (CCU), may inevitably be linked to a high risk of depressive symptoms for several reasons, though a whole spectrum of community care services may assist coping and exert beneficial effects on stress-related mental health problems amidst older community care users [10,11]. First, community care services could improve the quality of life and cultivate self-confidence, as the services provide home-visits nursing care, physical therapy, and psychological support for the elderly [11,12]. Second, older adults could foster a perception of proficiency or a sense of autonomy with living independently in their own homes, since community care plays an important part in meeting the elderly’s daily needs, such as dressing, bathing, serving meals, and/or mobility, etc. [13]. Third, collaborative community care services (companion care activities, social activities, and/or communication programs) has been linked to mild or severe geriatric depression. In community services, appropriate intervention strategies could be effective for the improvement of late-life mental health in these care settings [14,15]. Community care services can be a substantial source of instrumental, emotional, and social support against depression in older adults. We assume that the higher risk of depressive symptoms among older community care users could occur, since previous research has focused on the mental health of CCU only over a brief period. In community care settings, however, current research has been limited when attempting to fully account for the long-term effect of community care on mental health problems among older adults.
- According to clinical research for 3 months, 6 months, and 12 months of interventions with 306 community care users in the United States, significant improvement in depressive symptoms over time was observed [16]. A study analyzing 250 older, Canadian, community care users noted a beneficial effect from a nurse-led, care program for depression, cognitive function, and anxiety [12]. In a Korean study, older adults using community care services experienced significantly less depressive symptoms than their counterparts without such care (24.0 vs. 39.3%) [17]. However, some empirical research could not find any beneficial effect for CCU on mental health [18-20]. Although the degree of depression among older adults may decline through community care services, a meta-analysis using 22 studies could not suggest any conclusive evidence for the effectiveness of community care for an improvement in mental health [20]. Despite the controversy around the roles of community care on mental health, a dearth of research focuses on the applicability of long-term community care for older adults’ mental health in their community settings. Understanding the mental health trajectory appears foundational for effectively addressing how the impact of community care upon depressive symptoms was created. Thus, this study will expand previous research by focusing on the trajectory of depressive symptoms across 14 years of CCU and by identifying the potential influence of care on depression with long-term trajectories.
INTRODUCTION
- Data Source
- Data for this study were derived from the Korean Welfare Panel Survey (KOWEPS, 2019): a nationally representative panel survey conducted from 2006 to 2019 (14 years). The 2006 KOWEPS was drawn from the total Korean population, aged 15 and over, who live in the 17 provinces and 243 cities, gun, and gu in Korea (n=13 799). A multistage cluster, random sampling procedure was used to select respondents. Data were collected from November 6, 2006 to January 19, 2007, using Computer-Assisted Personal Interviewing. This study is focused on elderly born in 1940 or earlier, to reduce a cohort effect on the effectiveness and pattern of CCU. These are the generation who spent their youth during the turmoil of Japanese colonial era as well as the Korean War. Compared to those born in 1950s or later, they experienced not only extreme poverty and least access to education, but also significantly higher rates of depression and lower rates of positive health [21,22]. The subjects of this final sample were 3281 individuals aged 65 or older in 2006, and 1746 in 2019. We analyzed the data from all 14 waves of data collection, conducting every observation where information on depressive symptoms and CCU (36 334 person-year observations, baseline=3281) were available.
- Measures
- Depressive symptoms were assessed with the 11-item version Center for Epidemiological Studies Depression Scale (short-form, 11-item version CES-D) [23]. This scale measured how often the elderly experienced depressive symptoms during the past week (e.g., ‘I felt depressed’; ‘I did not feel like eating; my appetite was poor’; ‘I had trouble keeping my mind on what I was doing’). Participants responded to each item using a 4-point Likert scale from rarely or none of the time (0) to most or all of the time (3). Among the 11 questions, the “I was relatively well” and “I live without complaints” were reverse-coded to calculate the total of 11 questions. Total scores ranging from 0 to 60, were calculated by multiplying the sum of 11 items on the CES-D scale by 20/11. Cronbach’s alpha of depression scale for this sample was 0.871.
- The main independent variable was the time of years of CCU. Community care was defined by the public programs provided with total or partial assistance from public institutions and the public sectors. More specifically, community care programs included: (1) home-based services from long-term care insurance (LTCI) of Korea, (2) customized care services for those who are not eligible for the LTCI services, (3) basic care services provided to the elderly living alone who do not need nursing services, (4) home-based elderly support services targeting low-income older people who do not need long-term care insurance, and/or (5) home-based welfare services.
- Among the welfare services of older adults, community care services were (1) home-visit nursing and healthcare services, (2) home-visit services: dressing, bathing services, (3) day and night care, (4) home-visit housekeeping services (cleaning, laundry, meal preparation, etc.), (5) free meal supplies (no self-pay), (6) meal delivery services, (7) transportation and companion care, (8) social participation programs, etc. The respondents who answered ‘yes’ to any of these items was classified as one year of CCU at each survey year. To measure the number of years in CCU for each senior citizen, we added the year of CCU sequentially for 14 years from 2006 to 2018.
- Demographic factors (age, birth cohort, gender, marital status) and socioeconomic factors (education, household income, living alone), and health conditions (self-rated health, chronic diseases) were considered as potential covariates. Age was considered to be a stable, continuous variable, whereas birth cohorts were categorized into four five-year birth cohorts (born 1926 or earlier, 1926-1930, 1931-1935, 1936-1940). Marital status had two categories: currently married (reference), currently unmarried (single/widowed/separated/divorced). Education levels were split into ‘elementary school or less,’ ‘junior high school,’ ‘high school or more (reference).’ The equalized household income (=total household income/family size 0.5) was divided into tertiles. Living alone was categorized as “yes” or “no”. Self-rated health was grouped into three categories: (1) good, (2) average, and (3) poor. Chronic diseases were categorized as ‘yes’ or ‘no.’ We treated covariates of age, live alone, marital status, self-rated health, and chronic diseases as time-varying covariates, whose values can change across time. Otherwise, covariates of cohort, gender, education, years of CCU, were treated as time-invariant covariates.
- Statistical Analysis
- Descriptive statistics were calculated to understand the weighted percentages of demographic, socioeconomic, and health-related variables. Conducting a test for interaction, there was no statistical gender difference in the relationship between the number of years of CCU and depressive symptoms (F-value: 1.04, p-value: 0.411). Initially, we also checked for multicollinearity among independent variables. No multicollinear explanatory variables were found in this sample (variance inflation factor: 1.15-4.51; tolerance value: <0.72).
- We used a sequential modeling strategy for the multivariate portion of the analysis, progressively adjusting for our panel data analysis to assess the relationship between years of CCU and change in depressive symptoms. As widely used in social science, epidemiology, and/or econometrics, panel data analysis can analyze two-dimensional (cross-sectional, longitudinal) panel data.
- There are time-variant variables (age, marital status, education, household income, living alone, the number of years of CCU, and time-invariant variables (gender, birth cohort). In order to utilize some of the virtues of fixed effects and random effects methods, we performed a hybrid model for the analysis, after performing the Hausman-test (F-test: 3.64, p<0.001). We decomposed years of CCU into two parts, one representing within-person variation and the other representing between-person variation [24]. As group-mean centering, deviation scores of years of CCU from its within-person mean were calculated. The calculation of centered predictor is similar to the computational method for the fixed effects estimates. Furthermore, we can calculate coefficients for time-invariant predictors (gender, birth cohort).
- Panel data, by blending the inter-individual differences and intra-individual dynamics has several advantages over cross-sectional or time-series data [25]. First, panel data can control individual specificity. Panel data analysis can control both individual and time characteristic effects that are impossible in time series or cross-sectional analysis. Second, panel data provide more accurate inference of model parameters than cross-sectional data, as it contains more degrees of freedom and sample variability. Third, panel data contain information on both the intertemporal dynamics and the individuality of the entities may allow researchers to control the impact of omitted or unobserved variables.
- The first model included an age and birth cohort and years of CCU to examine variability in depressive symptoms across the years within its care utilization. It would be good to control all three axes of time (age, period [time], and birth cohort) to exclude the potential confounders. However, age and time effects cannot be considered at the same time, because of perfect multicollinearity. Both years of CCU (the centered variable) and mean years of CCU (person-specific mean year) were included as predictors in this model. Years of CCU (the centered variable) as linear and quadratic terms were included in the model to test a curvilinear relationship between years of CCU and depressive symptoms. In model 2, we affixed the control variables (i.e., gender, marital status, education, household income, living alone). Finally, the reference model was reexamined in expanded models that included self-rated health and chronic diseases. The adequacy of fit for growth model was tested through the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). All analyses were conducted by Stata version 17 (StataCorp., College Station, TX, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
- Ethics Statement
- Research involved secondary data analysis of the KOWEPS (2006-2019), which were approved by the Bioethics Committee (approval No. 33109, Statistics Korea). In addition, they are non-aggregated data which are carefully modified and then reviewed to ensure that no individual is directly or indirectly identified.
METHODS
Symptoms of depression
Community care utilization
Potential covariates
- The descriptive characteristics are presented in Table 1 and the sample at baseline (n=3281) were weighted to account for sampling design. The mean depression score was 7.92±0.12. Person years of CCU is 2.97±0.06 through the 14 survey years. The mean age of the participants was approximately 71.97±4.76 years. Approximately 43.4% of respondents were in a 1936-1940 birth cohort; 28.9% were in a 1931-1935 birth cohort; 15.5% were in a 1926-1930 birth cohort; and 12.3% in the oldest birth cohort. The sample consisted of 41.4% men and 58.6% women. As regards marital status, 60.1% were currently married, whereas 39.9% were currently unmarried. Approximately 67.7% of the respondents had earned elementary school or less, whereas 12.3% of them have a junior high school diploma, and 20.1% have a high school diploma or more. Approximately 20% of the respondents were living alone. In terms of health conditions, 60.4% of the respondents rated their health as poor, whereas less than one-fourth (70.8%) had at least one chronic disease.
- The results from panel data analysis predict depressive symptoms, using the stepwise process (Table 2). Based on model fit, linear and quadratic terms for age and years of CCU were included in the model. After adjusting for an age and birth cohort, the association between years of CCU (within-person variation) and depressive symptoms were negatively significant, whereas the quadratic term of years with CCU was positively significant (model 1). The association between years of CCU and depressive symptoms persisted even after adjusting for individual differences and health conditions. Meanwhile, the association between mean years of CCU (between-person variation) and depressive symptoms were positively significant in the reduced model, but the relationship disappeared after controlling for potentially confounding factors.
- Figure 1 depicts graphically the changes of depressive symptoms across years of CCU. As the graphic shows, the trajectory of depressive symptoms has a quadratic shape as regards years of CCU among older adults aged 65 and over. First, levels of depressive symptoms were highest among elderly in the first year of CCU. Then, depressive symptoms declined significantly over the 9-year interval of CCU, but steadily increased through the ensuing 14 years of receiving care. However, the beneficial effects of CCU on depressive symptoms were not completely eliminated over longer periods in such care.
RESULTS
- Using 14 waves of panel data, the goal of this study was to investigate the impact of CCU on depressive symptoms among older adults aged 65 and over. Furthermore, this study aimed to identify the trajectory of depressive symptoms across 14 years of CCU. This study expanded on previous research by tracing the long-term effect of CCU on mitigating depressive symptoms. In this present study, we have uncovered two important, evidential results that are related to CCU among the elderly population. First, CCU appears to act protectively against depressive symptoms for older community care users. Second, the trajectory of depressive symptoms across 14 years of CCU showed a U-shaped pattern: in the first year of CCU, the highest level of depressive symptoms was found, and then ameliorated significantly for up to 9 years after CCU. Furthermore, the protective effect of CCU on depressive symptoms still remains, though it seems to gradually weaken after 9 years of community care usage. Although, with beginning CCU, older community care users seem to suffer from higher levels of depressive symptoms, the beneficial effect of these care services were evident in regards to community care’s long-term utilization. Accordingly, these findings will offer an important contribution to this knowledge about the whole spectrum wherein the long-term effect of community care services shall curtail the depressive symptoms among older community care users.
- In agreement with an enormous amount of evidence, this study’s result identified that the highest level of depressive symptoms shift from the first stage of CCU amidst older adults. Several findings mirror this study’s evidence, which reported the highest risk of depressive symptoms among older community care users [5,6,8,26]. It is commonly accepted that social isolation and loneliness followed by serious medical conditions are closely related to an increased risk of persistent depressive symptoms [15,27]. In fact, Korea’s community care policy was implemented to provide care for older adults who have difficulties in carrying out their daily lives, due to severe chronic diseases, disabilities, and/or dementia. The elderly’s poor health status could lead to feelings of helplessness in carrying out their basic daily needs, which could bring on despair and depression in their community care settings [15,28]. In the initial stage of CCU, older adults, in particular, may fall into vicious cycles of helplessness that’s fueled by distressing social and psychological problems [17]. This finding suggests that special intervention programs should aim at reducing depressive symptoms that pressure, older adults who had at first reveled in the community care settings.
- Interestingly, our results indicated the long-term effects of community care services on depressive symptoms among older community care users. Moreover, the effect of CCU on depressive symptoms showed a U-shape pattern. Our findings offered important evidence suggesting that long-term utilization of community care may reduce the high risk of depressive symptoms among older adults using community care for the first time.
- Although previous studies have yielded inconsistent results in various populations, the U-shape curve in depressive symptoms across 14 years of CCU can be interpreted as showing that community care service’s beneficial role with depressive symptoms is very evident. Despite inconclusive results from a meta-analysis by Burns et al. [20], the highest level of depressive symptoms inside CCU’s first stage had substantially declined after up to 9 years of using such care. A systematic review of 3 studies, on the link between psychogeriatric community care and mental health, has proposed that community care interventions were effective in fewer admissions to hospital and nursing homes, as well as lower costs for this care [29]. Furthermore, the effectiveness of community care services may be essential for managing these social skills [29,30]. Given the diverse community care services including home-visit nursing, companion care activities, and/or lifelong education, community care covers daily living skills and daytime activities. Accordingly, older community care users can cultivate the perception of competence or healthy self-concepts as they perceive that their performing activities are self-determined. By engaging in social activities inside their community care settings, older adults can perceive of themselves as social beings who cope with stressful circumstances that potentially threaten their mental health [14,31].
- This study had several strengths. By employing the panel design from 2006-2018 KOWEPS, this research provided relatively accurate results. In addition, the nationwide large sample, over a 14-year period, allows us to analyze how continuous utilization of community care affects mental health across time. To our knowledge, there is no evidence that supports depression’s trajectory across long-term years of CCU. However, this study has several limitations. First, attention should be paid to the research results, since attribution bias could occur in a specific group selectively during the observation period across the 14 years of the panel survey. Second, omitted variable bias can influence on this study’s result, although multivariable models were used to control confounders. Possible risk and protective factors, such as biological, psychological, social factors, may interlink and influence depressive symptoms. In this study, however, we used panel data analysis which deals with omitted variable bias due to heterogeneity in the data. Third, due to small population who receiving sub-parts of community care services, this study also fails to investigate the distinct effect of each care service that may drive the relationship between CCU and depression. Fourth, we need to pay attention to the interpretation for sample, since this study’s sample was limited the elderly born in the year of 1940 or earlier. Further research is needed to fully understand which care services could be more effective for depression, and whether long-term care services could reduce depression for all older adults.
- Despite this study’s shortcomings, in our knowledge, our findings provided useful evidence that community and home-based care services could be used as an effective intervention strategy that integrates community mental health and aged care services to address service fragmentation. Furthermore, our findings can be generalized to the Korean elderly population, since this study utilized the representative sample of the 2006-2019 KOWEPS.
- In conclusion, our study highlights the importance of community care as a key intervention tool for older adults to sustain psychological wellbeing in community care settings. The findings implied that community care services might expand and be utilized in communities as a useful strategy for mental health interventions in vulnerable, older adult populations.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This research project was supported by the Ministry of Education of Republic of Korea and the National Research Foundation (NRF) of Korea (grant No. NRF- 2022S1A5C2A03092307).
-
AUTHOR CONTRIBUTIONS
Conceptualization: Kim IH, Kim CS, Jeong MH. Data curation: Kim IH, Jeong MH. Formal analysis: Kim IH, Jeong MH. Funding acquisition: Kim CS. Methodology: Kim IH, Jeong MH. Project administration: Kim CS, Kim IH. Visualization: Kim IH, Jeong MH. Writing – original draft: Kim IH, Jeong MH. Writing – review & editing: Kim IH, Kim CS.
Notes
ACKNOWLEDGEMENTS
| Characteristics | Mean±SD or n (%) |
|---|---|
| Depression | |
| 0-33 | 7.92±0.12 |
| Years of CCU1 | |
| 0-14 | 2.97±0.06 |
| Age (y) | |
| 65 or over | 71.97±4.76 |
| Birth cohort | |
| 1936-1940 | 1328 (43.4) |
| 1931-1935 | 979 (28.9) |
| 1926-1930 | 556 (15.5) |
| <1926 | 418 (12.3) |
| Gender | |
| Men | 1358 (41.4) |
| Women | 1923 (58.6) |
| Marital status | |
| Currently married | 1973 (60.1) |
| Currently unmarried | 1308 (39.9) |
| Education | |
| High school or more | 658 (20.1) |
| Junior high school | 402 (12.3) |
| Elementary school | 2221 (67.7) |
| Household income | |
| Low | 1095 (33.4) |
| Average | 1093 (33.3) |
| High | 1093 (33.3) |
| Live alone | |
| No | 2623 (80.0) |
| Yes | 658 (20.0) |
| Self-rated health | |
| Good | 757 (23.1) |
| Fair | 542 (16.5) |
| Poor | 1983 (60.4) |
| Chronic diseases | |
| None | 957 (29.2) |
| One & more | 2324 (70.8) |
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Age | |||
| 65 or over | -0.01 (0.02) | -0.01 (0.02) | -0.01 (0.02) |
| Age*age | 0.03 (0.01)*** | 0.02 (0.01)*** | 0.02 (0.01)*** |
| Birth cohort | |||
| 1936-1940 | Reference | Reference | Reference |
| 1931-1935 | 1.01 (0.18)*** | 0.74 (0.17)*** | 0.55 (0.15)*** |
| 1926-1930 | 1.90 (0.21)*** | 1.42 (0.20)*** | 1.11 (0.19)*** |
| <1926 | 1.87 (0.24)*** | 1.36 (0.23)*** | 1.17 (0.21)*** |
| Years of CCU1 | |||
| 1-14 y | -0.16 (0.03)*** | - 0.15 (0.03)*** | -0.12 (0.03)*** |
| Years of CCU*Years of CCU1 | |||
| 1-14 y | 0.02 (0.01)** | 0.02 (0.01)* | 0.02 (0.01)* |
| Mean years of CCU2 | 0.19 (0.04)*** | -0.01 (0.04) | -0.01 (0.03) |
| Gender | |||
| Men | - | Reference | Reference |
| Women | - | 1.34(0.16)*** | 1.11 (0.15)*** |
| Marital status | |||
| Married | - | Reference | Reference |
| Currently unmarried | - | 0.01 (0.16) | 0.19 (0.15) |
| Education | |||
| High school | - | Reference | Reference |
| Junior high school | - | 0.29 (0.25) | 0.23 (0.23) |
| Elementary school | - | 0.95 (0.20)*** | 0.72 (0.19)*** |
| Income | |||
| High | - | Reference | Reference |
| Middle | - | 0.72 (0.09)*** | 0.65 (0.09)*** |
| Low | - | 1.41 (0.10)*** | 1.31 (0.10)*** |
| Living alone | |||
| No | - | Reference | Reference |
| Yes | - | 0.45 (0.15)*** | 0.39 (0.14)** |
| Self-rated health | |||
| Good | - | - | Reference |
| Fair | - | - | 0.47 (0.08)*** |
| Poor | - | - | 2.34 (0.08)*** |
| Chronic diseases | |||
| None | - | - | Reference |
| One & more | - | - | 0.17 (0.09)† |
| -2 log likelihood | 196 210 | 195 797 | 194 721 |
| AIC | 196 220 | 195 807 | 194 731 |
| BIC | 196 252 | 195 839 | 194 763 |
Values are presented as B (standard error).
CCU, community care utilization; AIC, Akaike information criterion; BIC, Bayesian information criterion.
1 Years of CCU: deviation scores of years of CCU per each older adult (1-14 years).
2 Mean years of CCU: person-specific mean years of CCU.
† p<0.1,
* p<0.05,
** p<0.01,
*** p<0.001.
- 1. Prince MJ, Harwood RH, Blizard RA, Thomas A, Mann AH. Impairment, disability and handicap as risk factors for depression in old age. The Gospel Oak Project V. Psychol Med 1997;27(2):311-321ArticlePubMed
- 2. Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health 2020;20(1):129ArticlePubMedPMCPDF
- 3. Kim IH, Noh S, Chun H. Mediating and moderating effects in ageism and depression among the Korean elderly: the roles of emotional reactions and coping reponses. Osong Public Health Res Perspect 2016;7(1):3-11ArticlePubMedPMC
- 4. Lim JS, Chung SM, Chung S. The effect of “old-age” stigma on depression in middle-aged and older adults: the mediating effect of aging anxiety. Health Soc Welf Rev 2019;39(4):173-203. (Korean)Article
- 5. Ell K, Unützer J, Aranda M, Sanchez K, Lee PJ. Routine PHQ-9 depression screening in home health care: depression prevalence, clinical and treatment characteristics, and screening implementation. Home Health Care Serv Q 2006;24(4):1-19ArticlePubMedPMC
- 6. Xiang X, Leggett A, Himle JA, Kales HC. Major depression and subthreshold depression among older adults receiving home care. Am J Geriatr Psychiatry 2018;26: 939-949ArticlePubMedPMC
- 7. Komulainen K, Gluschkoff K, García Velázquez R, Airaksinen J, Szmulewicz A, Jokela M. Association of depressive symptoms with health care utilization in older adults: longitudinal evidence from the Survey of Health, Aging, and Retirement in Europe. Int J Geriatr Psychiatry 2021;36(4):521-529ArticlePubMedPDF
- 8. Lee IJ. The level and correlates of depression in home care elders: focused on comparison with community dwelling elders who do not use home care. Health Soc Welf Rev 2012;32(4):31-65. (Korean)Article
- 9. Thiam Y, Allaire JF, Morin P, Hyppolite SR, Doré C, Zomahoun HT, et al. A conceptual framework for integrated community care. Int J Integr Care 2021;21(1):5ArticlePubMedPMC
- 10. Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol 2007;3: 377-401ArticlePubMed
- 11. Flanagan S, Damery S, Combes G. The effectiveness of integrated care interventions in improving patient quality of life (QoL) for patients with chronic conditions. An overview of the systematic review evidence. Health Qual Life Outcomes 2017;15(1):188ArticlePubMedPMCPDF
- 12. Markle-Reid MF, McAiney C, Forbes D, Thabane L, Gibson M, Hoch JS, et al. Reducing depression in older home care clients: design of a prospective study of a nurse-led interprofessional mental health promotion intervention. BMC Geriatr 2011;11: 50ArticlePubMedPMCPDF
- 13. Joo S, Jun H, Choi B. The moderating effect of home-based welfare facilities for older adults between ADL/IADL and depressive symptoms among Korean in later life. J Korea Gerontol Soc 2018;38(1):243-259. (Korean)
- 14. Ouyang Z, Chong AM, Ng TK, Liu S. Leisure, functional disability and depression among older Chinese living in residential care homes. Aging Ment Health 2015;19(8):723-730ArticlePubMed
- 15. Kim IH, Kim CS. “Leisure life satisfaction:” will it have a beneficial impact on depression among older adults in community care settings in Korea? J Prev Med Public Health 2022;55(4):398-406ArticlePubMedPMCPDF
- 16. Bruce ML, Raue PJ, Reilly CF, Greenberg RL, Meyers BS, Banerjee S, et al. Clinical effectiveness of integrating depression care management into medicare home health: the Depression CAREPATH Randomized trial. JAMA Intern Med 2015;175(1):55-64ArticlePubMedPMC
- 17. Chung S. Residential status and depression among Korean elderly people: a comparison between residents of nursing home and those based in the community. Health Soc Care Community 2008;16(4):370-377ArticlePubMed
- 18. Thornicroft G, Deb T, Henderson C. Community mental health care worldwide: current status and further developments. World Psychiatry 2016;15(3):276-286ArticlePubMedPMC
- 19. Markle-Reid M, McAiney C, Fisher K, Ganann R, Gauthier AP, Heald-Taylor G, et al. Effectiveness of a nurse-led hospital-to-home transitional care intervention for older adults with multimorbidity and depressive symptoms: a pragmatic randomized controlled trial. PLoS One 2021;16(7):e0254573ArticlePubMedPMC
- 20. Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al. Home treatment for mental health problems: a systematic review. Health Technol Assess 2001;5(15):1-139ArticlePDF
- 21. Namgung E. Will the Korean elderly get healthier?: age, cohort, period effectiveness. 2022 [cited 2023 Nov 21]. Available from: https://kostat.go.kr/board.es?mid=a90102010100&bid=11918 (Korean)
- 22. Tampubolon G, Maharani A. When did old age stop being depressing? Depression trajectories of older Americans and Britons 2002-2012. Am J Geriatr Psychiatry 2017;25(11):1187-1195ArticlePubMedPMC
- 23. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385-401
- 24. Neuhaus JM, Kalbfleisch JD. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 1998;54(2):638-645ArticlePubMed
- 25. Hsiao C. Panel data analysis—advantages and challenges. Test 2007;16(1):1-22ArticlePDF
- 26. Pepin R, Leggett A, Sonnega A, Assari S. Depressive symptoms in recipients of home- and community-based services in the United States: are older adults receiving the care they need? Am J Geriatr Psychiatry 2017;25(12):1351-1360ArticlePubMedPMC
- 27. Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav 2009;50(1):31-48ArticlePubMedPMCPDF
- 28. Pearlin LI, Bierman A. Current issues and future directions in research into the stress process. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the sociology of mental health. Dordrecht: Springer; 2013. p. 325-340Article
- 29. Klug G, Gallunder M, Hermann G, Singer M, Schulter G. Effectiveness of multidisciplinary psychiatric home treatment for elderly patients with mental illness: a systematic review of empirical studies. BMC Psychiatry 2019;19(1):382ArticlePubMedPMCPDF
- 30. Killaspy H, Harvey C, Brasier C, Brophy L, Ennals P, Fletcher J, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry 2022;21(1):96-123ArticlePubMedPMCPDF
- 31. Coleman D, Iso-Ahola SE. Leisure and health: the role of social support and self-determination. J Leis Res 1993;25(2):111-128Article
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite