Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 55(4); 2022 > Article
-
Special Article
The KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD): A Korean Chronic Kidney Disease Cohort -
Kook-Hwan Oh1
 , Sue K. Park2,3,4
, Sue K. Park2,3,4 , Jayoun Kim5
, Jayoun Kim5 , Curie Ahn6
, Curie Ahn6 ,
, -
Journal of Preventive Medicine and Public Health 2022;55(4):313-320.
DOI: https://doi.org/10.3961/jpmph.22.031
Published online: July 1, 2022
1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
2Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea
3Cancer Research Institute, Seoul National University, Seoul, Korea
4Integrated Major in Innovative Medical Science, Seoul National University College of Medicine, Seoul, Korea
5Medical Research Collaborating Center, Seoul National University Hospital, Seoul, Korea
6Department of Internal Medicine, National Medical Center, Seoul, Korea
- Corresponding author: Kook-Hwan Oh, Department of Internal Medicine, Seoul National University College of Medicine, 103 Daehak-ro, Jongno-gu, Seoul 03080, Korea, E-mail: khoh@snu.ac.kr
Copyright © 2022 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- The KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD) was launched in 2011 with the support of the Korea Disease Control and Prevention Agency. The study was designed with the aim of exploring the various clinical features and characteristics of chronic kidney disease (CKD) in Koreans, and elucidating the risk factors for CKD progression and adverse outcomes of CKD. For the cohort study, nephrologists at 9 tertiary university-affiliated hospitals participated in patient recruitment and follow-up. Biostatisticians and epidemiologists also participated in the basic design and structuring of the study. From 2011 until 2016, the KNOW-CKD Phase I recruited 2238 adult patients with CKD from stages G1 to G5, who were not receiving renal replacement therapy. The KNOW-CKD Phase II recruitment was started in 2019, with an enrollment target of 1500 subjects, focused on diabetic nephropathy and hypertensive kidney diseases in patients with reduced kidney function who are presumed to be at a higher risk of adverse outcomes. As of 2021, the KNOW-CKD investigators have published articles in the fields of socioeconomics, quality of life, nutrition, physical activity, renal progression, cardiovascular disease and outcomes, anemia, mineral bone disease, serum and urine biomarkers, and international and inter-ethnic comparisons. The KNOW-CKD researchers will elaborate a prediction model for various outcomes of CKD such as the development of end-stage kidney disease, major adverse cardiovascular events, and death.
- Kidney Disease Improving Global Outcomes defined chronic kidney disease (CKD) as abnormalities of kidney structure or function, persisting for >3 months, regardless of their underlying cause [1]. CKD is a growing health burden worldwide [2], as well as in Korea [3]. The global all-age mortality rate from CKD increased by 41.5% between 1990 and 2017 [2]. The prevalence of CKD in Korea is estimated to be 13% in the adult population [4]. Approximately 5% of the Korean adult population is estimated to have decreased renal function, with an estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m2 [4]. CKD, which potentially leads to dialysis or kidney transplantation, presents a major threat for cardiovascular (CV) events and all-cause mortality. The numbers of patients with CKD and end-stage kidney disease (ESKD) are starkly increasing [5,6]. Not only is CKD a significant threat in terms of morbidity and mortality, but the overall health expenditures for CKD management are remarkably increasing.
- In order to expand our medical knowledge regarding the basic features of CKD in Koreans and the clinical course and risk factors of renal progression and adverse outcomes, the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD) was launched in 2011 with support from the Korean Disease Control and Prevention Agency (KDCA) [7]. Between 2011 and 2016, KNOW-CKD recruited 2238 adult subjects with CKD at 9 tertiary care hospitals throughout Korea [8]. It is expected that KNOW-CKD will provide abundant information on various issues, such as CV comorbidities, anemia, mineral metabolic derangements, quality of life (QoL), and health-related habits in CKD patients. It is exceptional that, unlike other CKD cohort studies such as the Chronic Renal Insufficiency Cohort (CRIC) of the United States [9,10] or the Chronic Kidney Disease Japan Cohort (CKD-JAC) of Japan [11], the KNOW-CKD study also recruited subjects at early stages of CKD (stage G1 and G2), as well as advanced stages, thereby enabling research on the long-term clinical course of early CKD (Supplemental Material 1).
- The study aims of KNOW-CKD are as follows: (1) to investigate the natural clinical course of CKD, such as renal function deterioration, mortality, and complications with respect to the cause, glomerular filtration rate, and albuminuria categories, (2) to evaluate the risk factors for renal progression and related complications by elucidating the mechanistic link between renal injury and adverse outcomes, (3) to establish a clinical database and obtain numerous biological resources for future CKD research, and (4) to identify the genetic and molecular influences on renal progression and related complications.
- The present article provides the basic design and summary of the findings from the KNOW-CKD Study Phase I and II.
INTRODUCTION
- Organization
- The KNOW-CKD was designed as a hospital-based cohort study. Nephrologists working at 9 clinical centers of major university-affiliated hospitals, epidemiologists, specialists in laboratory medicine, and biostatisticians have participated in this study. The basic study protocol was approved by the ethical committee of the 9 participating centers. The study is supervised by the CKD Advisory Committee, which comprises members from the KDCA and the Korean Society of Nephrology (NCT01630486 at http://www.clinicaltrials.gov).
- Study Population
- Each participating center enrolled consecutive individuals over a 5-year period from May 2011 to January 2016, totaling 2238 adult patients with CKD who provided written informed consent. The participating individuals were followed until death or drop-out.
- The inclusion criteria of the KNOW-CKD Phase I study were ethnic Korean patients aged between 20 years and 75 years and at CKD stages ranging from G1 to G5 (non-dialysis).
- Excluded subjects were those who (1) were unable or unwilling to give written consent, (2) had a history of chronic dialysis or any organ transplantation, (3) had severe heart failure or liver cirrhosis, (4) had a past or current history of malignancy, (5) were currently pregnant, or (6) had a single kidney due to trauma or nephrectomy.
- CKD stages were defined on the basis of the eGFR calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI [cr]) formula [12].
- Data Collection and Management
- The study protocol and information collected at each study visit are summarized in Supplemental Material 2 [8]. Demographic and anthropometric information was collected according to the pre-specified protocol, reported elsewhere [7]. Serum creatinine was measured at a central laboratory (LabGenomics, Seongnam, Korea), using an assay traceable to the international reference material. Essential laboratory tests from the serum and urine such as serum creatinine, cystatin C, urine protein/albumin, and intact parathyroid hormone were conducted at a central laboratory in order to minimize inter-assay variation. Radiographic images such as lateral abdominal X-rays and kidney computed tomography were sent to the data coordinating center and evaluated by at least 2 independent and blinded experts. Study-related clinical and laboratory data were collected on an electronic web-based case report form using the PhactaX system, developed and maintained by the Medical Research Collaborating Center of Seoul National University Hospital.
- Recruitment and Follow-up
- From 2011 until 2016, Phase I of the KNOW-CKD study recruited 2238 subjects with CKD from 9 university-affiliated tertiary-care hospitals throughout Korea. We classified the subjects according to the underlying cause of CKD into 4 subgroups: glomerulonephritis, diabetic nephropathy, hypertensive nephropathy, and autosomal dominant polycystic kidney disease. The other causative diseases were categorized as “unclassified.” Hypertensive nephropathy and autosomal dominant polycystic kidney disease were oversampled in order to compare among the 4 major causative diseases of CKD. The basic demographic and clinical features of the KNOW-CKD Phase I subjects were reported previously elsewhere [13].
- Outcomes: Definitions and Data Acquisition
- Composite renal events are defined as eGFR halving or development of ESKD. CV events are defined as any first event of the following: acute myocardial infarction, unstable angina, either ischemic or hemorrhagic cerebral stroke, congestive heart failure, symptomatic arrhythmia, aggravated valvular heart disease, pericardial disease, abdominal aortic aneurysm, and severe peripheral arterial disease that require hospitalization or interventions during follow-up. Three-point major adverse cardiovascular events (3-point MACE) were defined as fatal cardiac events, acute myocardial infarction, or stroke (ischemic or hemorrhagic). Four-point MACE included 3-point MACE and unstable angina.
- Data on the time and specific causes of death were also obtained from either hospital records or the Korean Statistical Information Service. Other events, such as all-cause hospitalization, surgery, and fractures, were also collected during the follow-up period. All the events described above were recorded on a special report form and further adjudicated by the Central Adjudication Committee of the KNOW-CKD Study.
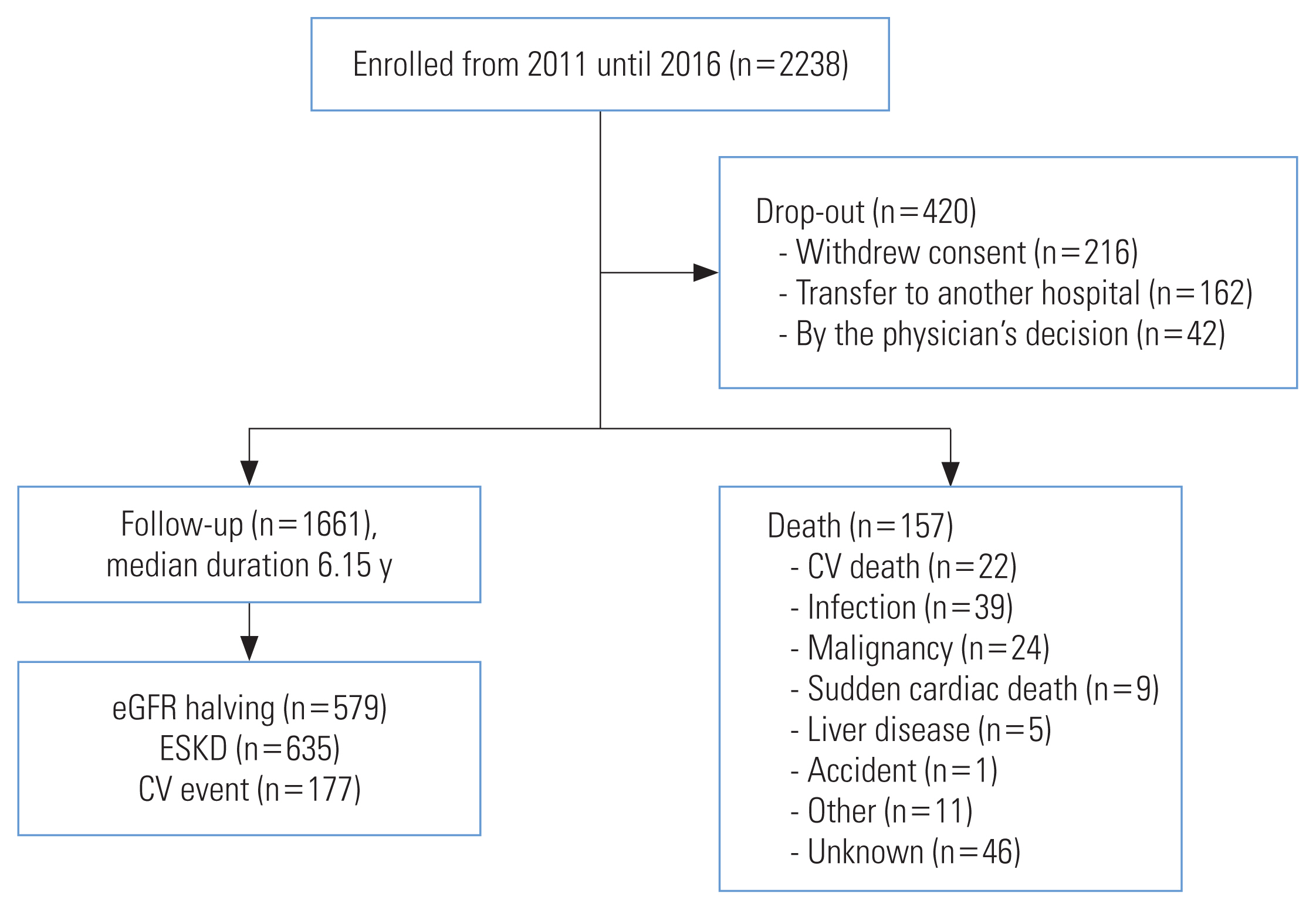
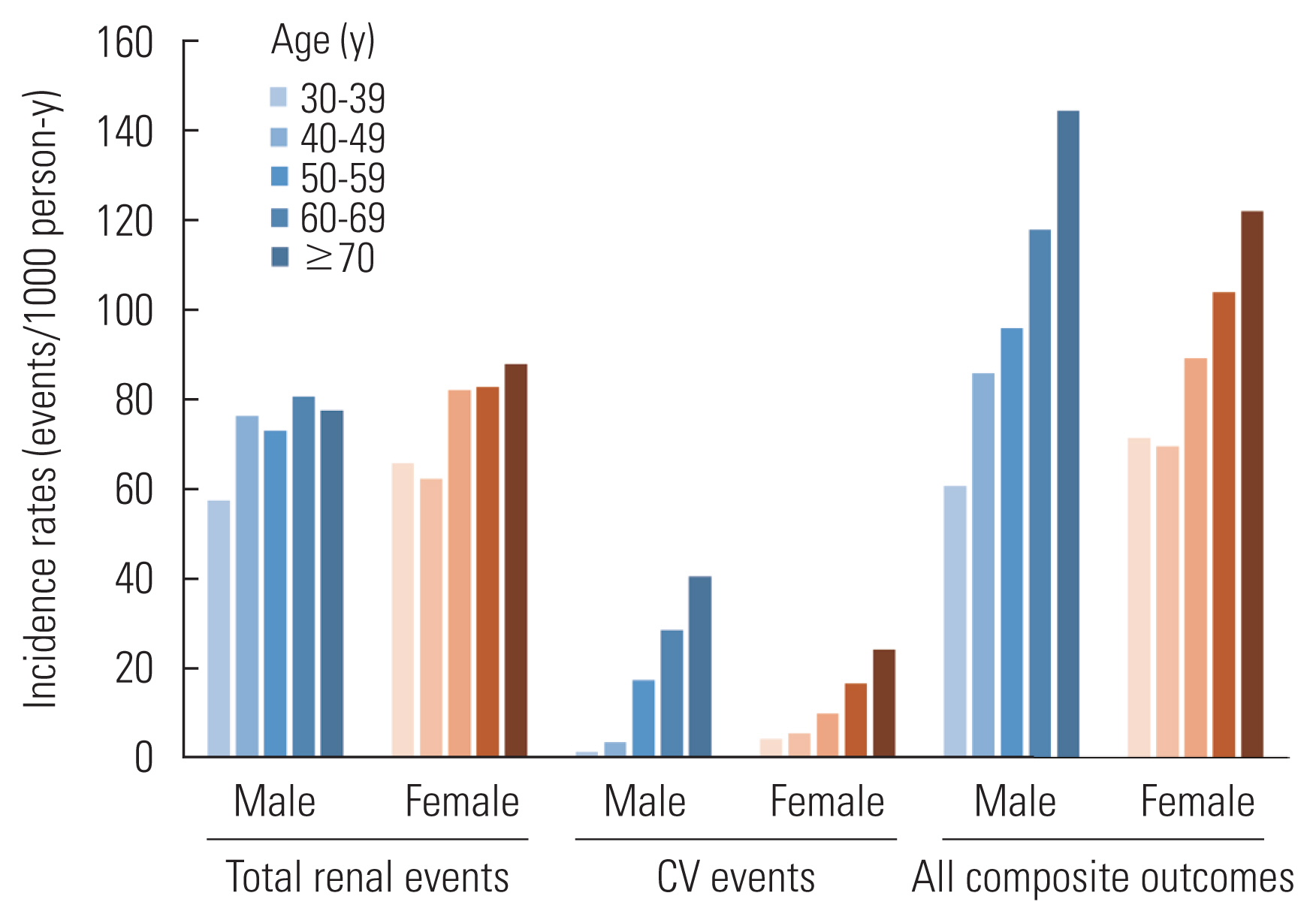
- As of March 31, 2021, among 2238 subjects enrolled in the study, there were 157 deaths, and 177 fatal or non-fatal CV events after 6.15 years (median) of follow-up. Furthermore, 635 subjects developed ESKD (Figure 1). There were 420 drop-outs (18.7%) during follow-up as of March 2021. Basic statistics, such as the crude and adjusted incidence rates of major events, such as ESKD, CV events and death, have been reported elsewhere (Table 1 and Figure 2) [14]. The KNOW-CKD Phase I study has recently revised the study protocol in order to extend the follow-up period of the participants for up to 20 years.
- Major Findings on Chronic Kidney Disease
- We have conducted research in a broad range of CKD-related areas, such as (1) the influence of socioeconomics and health-related habits on the outcomes of CKD, (2) CV comorbidities, (3) anemia, (4) mineral bone disease, (5) nutrition and QoL, (5) biomarker discovery, (6) clinical courses and outcomes of Korean CKD patients, and (7) international comparisons and meta-analysis. As of December 2021, the KNOW-CKD investigators have published 87 articles in major peer-reviewed international journals and are currently conducting research on >150 different research topics (Figure 1 and Supplemental Material 3). For a summary and major findings related to the KNOW-CKD Study, the readers are referred either to the recent review published elsewhere [13] or to the following website (http://www.know-ckd.org).
- Socioeconomic status (SES), defined by education and income levels, is related to a set of socioeconomic factors, including health insurance, medical literacy, transportation, stress level, housing quality, and access to medical care [15]. Research analyzing KNOW-CKD data showed that lower SES was significantly associated with left ventricular hypertrophy, which is a major surrogate marker for future CV events [16]. An analysis of the association between SES and longitudinal outcomes is currently underway.
- The subjects of KNOW-CKD were categorized into 6 groups according to a combination of body mass index (BMI; normal, overweight, obese) and waist-to-hip ratio (WHR; lower or higher than the sex-specific median WHR). Subjects with a normal BMI but higher WHR had a higher risk of coronary artery calcification than those with a normal BMI and lower WHR (odds ratio, 2.104; 95% confidence interval [CI], 1.074 to 4.121). Thus, BMI and WHR—2 surrogates of obesity—can help predict CV risk in CKD patients [17].
- The KNOW-CKD researchers investigated the effect of health-related habits [18–21] and physical activity of individuals on CKD outcomes. The study collected detailed information on exercise, alcohol drinking, and smoking through a self-reported questionnaire. Compared with non-drinkers, regular and occasional binge drinkers had 2.2-fold (95% CI, 1.38 to 3.46) and a 2.0-fold (95% CI, 1.33 to 2.98) higher risks of CKD progression, respectively. This association was particularly evident in patients who had decreased kidney function and proteinuria [20]. In a recent publication, the KNOW-CKD study investigators reported that the higher systolic and diastolic blood pressure (BP) levels are associated with a higher risk of a composite kidney outcome reflecting CKD progression. Systolic BP had a stronger association with adverse kidney outcomes than diastolic BP [22].
- The incidence, prevalence, and clinical outcomes of CKD/ESKD differ depending on patients’ socio-genetic backgrounds [23,24]. The KNOW-CKD investigators have been actively participating in the International Network of CKD Cohort Studies (iNET-CKD) [25], searching for determinants explaining these differences through inter-ethnic and international comparisons and meta-analyses.
- A recent publication compared the prevalence of uncontrolled BP among 17 cohort studies, including 34 602 individuals with eGFR <60 mL/min/1.73 m2 and treated hypertension adjusted for potential confounders [26]. The crude prevalence of BP ≥140/90 mmHg ranged from 28% to 61%. The adjusted prevalence ratios indicated better control in North America and high-income Asian countries, including Korea and Japan. Of particular note, KNOW-CKD exhibited the lowest prevalence of uncontrolled hypertension (27.3%) among the 17 participating CKD cohorts.
- Another international meta-analysis compared the longitudinal outcomes of CKD across 8 different cohorts [27]. The KNOW-CKD cohort population, as compared to the other 7 cohorts in Europe, Japan, North America, and South America, exhibited relatively lower incidence of all-cause mortality, while exhibiting higher incidences of renal progression and ESKD, after adjustment (Supplemental Material 4).
- Currently, KNOW-CKD is participating in the international collaborative research for exploring the international variability in hemoglobin and the approach to anemia treatment among individuals with CKD.
KNOW-CKD PHASE I
- KNOW-CKD has recently launched the Phase II study, with a target recruitment of another 1500 subjects from the year 2019 until 2022. The Phase II KNOW-CKD study aims (1) to enhance the statistical power by enlarging the total pool of CKD subjects in the cohort, particularly those with eGFR <60 mL/min/1.73 m2 and with higher risks of adverse events, (2) to further focus on diabetic nephropathy and hypertensive kidney disease, which are the 2 most common causes of CKD in Korea, (3) to strengthen the KNOW-CKD research as a resource on the health habits of CKD patients by obtaining more information on their dietary patterns, nutritional status, and cognitive function (Table 2).
- In addition, with the coronavirus disease 2019 (COVID-19) pandemic, KNOW-CKD Phase II has modified its study protocol in order to investigate the impact of COVID-19 vaccination and the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection on the clinical course of CKD subjects. The study is collecting COVID-19-related information, such as SARS-CoV-2 infections, vaccination against COVID-19, and related adverse events. This information will provide valuable insights into the long-term effects of COVID-19 on the clinical course of CKD.
- As of September 2021, the KNOW-CKD Phase II has enrolled 1071 subjects, among whom 62% have diabetes. An interim analysis of the KNOW-CKD Phase II study subjects is presented in Table 3.
KNOW-CKD PHASE II
- As the nation’s largest CKD cohort, KNOW-CKD has elucidated numerous clinical features of CKD, particularly related to an East Asian population. The KNOW-CKD cohort has endeavored to answer basic questions regarding the clinical courses of the Korean population with CKD and to elucidate risk factors for adverse outcomes. Among various aspects of CKD, particular emphasis has been placed on socioeconomic factors, nutrition and QoL, health habits, CKD progression, CV comorbidities and outcomes, anemia, mineral bone disease, biomarker discovery, and international and inter-ethnic comparisons. KNOW-CKD Phase I plans to extend the follow-up period up to 20 years, and the Phase II study is currently recruiting subjects with CKD at higher risk of adverse outcomes in order to obtain more robust statistical power and to eventually offer a prediction model for the long-term consequences of CKD. The KNOW-CKD will enable us to identify the at-risk population, on whom we can focus more medical attention for risk modification. Furthermore, by pursuing biomarker discovery research using serum, urine, and DNA samples, the KNOW-CKD will provide a stepping stone for future personalized medicine.
- Details on the design, patient enrollment, investigator group, research publications, and annual report are available at the website of the KNOW-CKD study (http://www.know-ckd.org).
- Ethics Statement
- The present study protocol was reviewed and approved by the institutional review boards at each participating center: Seoul National University Hospital (1104-089-359); Seoul National University Bundang Hospital (B-1106/129-008); Yonsei University Severance Hospital (4-2011-0163); Kangbuk Samsung Medical Center (2011-01-076); Seoul St. Mary’s Hospital (KC11OIMI0441); Gil Hospital (GIRBA2553); Eulji General Hospital (201105-01); Chonnam National University Hospital (CNUH-2011-092); Pusan Paik Hospital (11-091).
SUMMARY AND CONCLUSION
SUPPLEMENTAL MATERIALS
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This study was supported by the Research Program funded by the Korean Disease Control and Prevention Agency (KDCA) (2011E3300300, 2012E3301100, 2013E3301600, 2013E3301601, 2013E3301602, 2016E3300200, and 2019E320100).
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTION
Conceptualization: Oh KH, Park SK, Kim J, Ahn C. Data curation: Oh KH, Kim J. Formal analysis: Oh KH, Kim J. Funding acquisition: Ahn C, Oh KH. Methodology: Park SK. Project administration: Oh KH. Visualization: Oh KH, Kim J. Writing – original draft: Oh KH. Writing – review & editing: Oh KH, Kim J, Park SK, Ahn C.
Notes
| Variables | Total CKD patients | Diabetic CKD patients | Non-diabetic CKD patients | p-value3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| Event no. | Incidence rates | Standardized incidence rates2 | Event no. | Incidence rates | Standardized incidence rates | Event no. | Incidence rates | Standardized incidence rates | ||
| ESKD | 635 | 54.2 | 47.4 | 307 | 94.0 | 119.3 | 328 | 39.0 | 36.4 | <0.001 |
|
|
||||||||||
| ESKD or eGFR halving | 830 | 75.0 | 67.7 | 364 | 119.7 | 155.2 | 466 | 58.2 | 55.3 | <0.001 |
|
|
||||||||||
| eGFR halving | 579 | 48.0 | 46.0 | 230 | 64.1 | 86.7 | 349 | 41.4 | 39.9 | <0.001 |
|
|
||||||||||
| 3-point MACE | 91 | 6.7 | 4.0 | 54 | 12.8 | 8.3 | 37 | 4.0 | 2.5 | <0.001 |
|
|
||||||||||
| 4-point MACE | 115 | 8.5 | 4.9 | 68 | 16.3 | 9.8 | 47 | 5.0 | 3.2 | <0.001 |
|
|
||||||||||
| Myocardial infarction | 20 | 1.5 | 0.8 | 13 | 3.0 | 1.1 | 7 | 0.7 | 0.5 | 0.003 |
|
|
||||||||||
| Unstable angina | 29 | 2.1 | 1.0 | 17 | 4.0 | 1.7 | 12 | 1.3 | 0.8 | 0.003 |
|
|
||||||||||
| Congestive heart failure | 14 | 1.0 | 0.5 | 8 | 1.9 | 0.7 | 6 | 0.6 | 0.4 | 0.048 |
|
|
||||||||||
| Ischemic stroke | 33 | 2.4 | 1.3 | 20 | 4.7 | 2.9 | 13 | 1.4 | 0.8 | 0.001 |
|
|
||||||||||
| Hemorrhagic stoke | 14 | 1.0 | 0.6 | 5 | 1.2 | 0.4 | 9 | 1.0 | 0.6 | 0.733 |
|
|
||||||||||
| Any death | 157 | 11.4 | 7.0 | 89 | 20.5 | 10.7 | 68 | 7.2 | 5.2 | <0.001 |
|
|
||||||||||
| All composite outcomes | 992 | 93.6 | 78.9 | 439 | 156.6 | 173.2 | 552 | 70.9 | 64.3 | <0.001 |
KNOW-CKD, KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease; CKD, chronic kidney disease; ESKD, end-stage kidney disease; eGFR, estimated glomerular filtration rate; MACE, major adverse cardiovascular events; 3-point MACE, fatal cardiac events+acute myocardial infarction+stroke (ischemic, hemorrhagic); 4-point MACE, fatal cardiac events+acute myocardial infarction+stroke (ischemic, hemorrhagic)+unstable angina.
1 Median follow-up 6.15 years (range, 0.00 to 9.49).
2 Standardized to the Korean population as of 2005.
3 From Poisson regression model in the incidence comparisons between event rates in diabetic CKD patients and non-diabetic CKD patients.
| Demographic factors | Total (n=1071) | Stage | p-value | |||
|---|---|---|---|---|---|---|
|
|
||||||
| G3a (n=332) | G3b (n=479) | G4 (n=260) | ||||
| Age (y) | Mean±SD | 66.0±8.2 | 65.5±8.0 | 66.9±8.1 | 64.9±8.3 | 0.0011 |
| Med [Min-Max] | 67 [45–79] | 66 [45–79] | 68 [46–79] | 65 [45–79] | ||
|
|
||||||
| Sex | Male | 749 (69.9) | 257 (77.4) | 328 (68.5) | 164 (63.1) | 0.0012 |
| Female | 322 (30.1) | 75 (22.6) | 151 (31.5) | 96 (36.9) | ||
|
|
||||||
| Diabetes | Yes | 665 (62.1) | 181 (54.5) | 312 (65.1) | 172 (66.2) | 0.0032 |
| No | 406 (37.9) | 151 (45.5) | 167 (34.9) | 88 (33.8) | ||
- 1. Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 2013;158(11):825-830ArticlePubMed
- 2. GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020;395(10225):709-733PubMedPMC
- 3. Kang YU, Bae EH, Ma SK, Kim SW. Determinants and burden of chronic kidney disease in a high-risk population in Korea: results from a cross-sectional study. Korean J Intern Med 2016;31(5):920-929ArticlePubMedPMCPDF
- 4. Kim S, Lim CS, Han DC, Kim GS, Chin HJ, Kim SJ, et al. The prevalence of chronic kidney disease (CKD) and the associated factors to CKD in urban Korea: a population-based cross-sectional epidemiologic study. J Korean Med Sci 2009;24(Suppl 1):S11-S21ArticlePubMedPMC
- 5. Ji E, Kim YS. Prevalence of chronic kidney disease defined by using CKD-EPI equation and albumin-to-creatinine ratio in the Korean adult population. Korean J Intern Med 2016;31(6):1120-1130ArticlePubMedPMCPDF
- 6. Jin DC, Yun SR, Lee SW, Han SW, Kim W, Park J, et al. Lessons from 30 years’ data of Korean end-stage renal disease registry, 1985–2015. Kidney Res Clin Pract 2015;34(3):132-139ArticlePubMedPMC
- 7. Oh KH, Park SK, Park HC, Chin HJ, Chae DW, Choi KH, et al. KNOW-CKD (KoreaN cohort study for Outcome in patients With Chronic Kidney Disease): design and methods. BMC Nephrol 2014;15: 80ArticlePubMedPMCPDF
- 8. Kang E, Han M, Kim H, Park SK, Lee J, Hyun YY, et al. Baseline general characteristics of the Korean chronic kidney disease: report from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD). J Korean Med Sci 2017;32(2):221-230ArticlePubMedPMCPDF
- 9. Feldman HI, Appel LJ, Chertow GM, Cifelli D, Cizman B, Daugirdas J, et al. The chronic renal insufficiency cohort (CRIC) study: design and methods. J Am Soc Nephrol 2003;14(7 Suppl 2):S148-S153ArticlePubMed
- 10. Lash JP, Go AS, Appel LJ, He J, Ojo A, Rahman M, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol 2009;4(8):1302-1311ArticlePubMedPMC
- 11. Imai E, Matsuo S, Makino H, Watanabe T, Akizawa T, Nitta K, et al. Chronic Kidney Disease Japan Cohort (CKD-JAC) study: design and methods. Hypertens Res 2008;31(6):1101-1107ArticlePubMed
- 12. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150(9):604-612ArticlePubMedPMC
- 13. Oh KH, Kang M, Kang E, Ryu H, Han SH, Yoo TH, et al. The KNOW-CKD Study: what we have learned about chronic kidney diseases. Kidney Res Clin Pract 2020;39(2):121-135ArticlePubMedPMC
- 14. Ryu H, Kim J, Kang E, Hong Y, Chae DW, Choi KH, et al. Incidence of cardiovascular events and mortality in Korean patients with chronic kidney disease. Sci Rep 2021;11(1):1131ArticlePubMedPMCPDF
- 15. Norton JM, Moxey-Mims MM, Eggers PW, Narva AS, Star RA, Kimmel PL, et al. Social determinants of racial disparities in CKD. J Am Soc Nephrol 2016;27(9):2576-2595ArticlePubMedPMC
- 16. Kang E, Lee J, Kim HJ, Han M, Kim SW, Lee KB, et al. The association between socioeconomic disparities and left ventricular hypertrophy in chronic kidney disease: results from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD). BMC Nephrol 2018;19(1):203ArticlePubMedPMCPDF
- 17. Lee MJ, Park JT, Park KS, Kwon YE, Han SH, Kang SW, et al. Normal body mass index with central obesity has increased risk of coronary artery calcification in Korean patients with chronic kidney disease. Kidney Int 2016;90(6):1368-1376ArticlePubMed
- 18. Lee S, Kang S, Joo YS, Lee C, Nam KH, Yun HR, et al. Smoking, smoking cessation, and progression of chronic kidney disease: results from KNOW-CKD study. Nicotine Tob Res 2021;23(1):92-98ArticlePubMedPDF
- 19. Kang M, Kang E, Ryu H, Hong Y, Han SS, Park SK, et al. Measured sodium excretion is associated with CKD progression: results from the KNOW-CKD study. Nephrol Dial Transplant 2021;36(3):512-519ArticlePubMedPDF
- 20. Joo YS, Koh H, Nam KH, Lee S, Kim J, Lee C, et al. Alcohol consumption and progression of chronic kidney disease: results from the Korean cohort study for outcome in patients with chronic kidney disease. Mayo Clin Proc 2020;95(2):293-305ArticlePubMed
- 21. Sung SA, Hyun YY, Lee KB, Park HC, Chung W, Kim YH, et al. Sleep duration and health-related quality of life in predialysis CKD. Clin J Am Soc Nephrol 2018;13(6):858-865ArticlePubMedPMC
- 22. Lee JY, Park JT, Joo YS, Lee C, Yun HR, Yoo TH, et al. Association of blood pressure with the progression of CKD: findings from KNOW-CKD study. Am J Kidney Dis 2021;78(2):236-245ArticlePubMed
- 23. Muntner P, Newsome B, Kramer H, Peralta CA, Kim Y, Jacobs DR Jr, et al. Racial differences in the incidence of chronic kidney disease. Clin J Am Soc Nephrol 2012;7(1):101-107ArticlePubMedPMC
- 24. Mehrotra R, Kermah D, Fried L, Adler S, Norris K. Racial differences in mortality among those with CKD. J Am Soc Nephrol 2008;19(7):1403-1410ArticlePubMedPMC
- 25. Dienemann T, Fujii N, Orlandi P, Nessel L, Furth SL, Hoy WE, et al. International Network of Chronic Kidney Disease cohort studies (iNET-CKD): a global network of chronic kidney disease cohorts. BMC Nephrol 2016;17(1):121ArticlePubMedPMCPDF
- 26. Alencar de Pinho N, Levin A, Fukagawa M, Hoy WE, Pecoits-Filho R, Reichel H, et al. Considerable international variation exists in blood pressure control and antihypertensive prescription patterns in chronic kidney disease. Kidney Int 2019;96(4):983-994ArticlePubMed
- 27. Orlandi PF, Huang J, Fukagawa M, Hoy W, Jha V, Oh KH, et al. A collaborative, individual-level analysis compared longitudinal outcomes across the International Network of Chronic Kidney Disease (iNETCKD) cohorts. Kidney Int 2019;96(5):1217-1233ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Kidney Health Plan 2033 in Korea: bridging the gap between the present and the future
Do Hyoung Kim, Young Youl Hyun, Jin Joo Cha, Sua Lee, Hyun Kyung Lee, Jong Wook Choi, Su-Hyun Kim, Sang Youb Han, Cheol Whee Park, Eun Young Lee, Dae Ryong Cha, Sung Gyun Kim, Chun Soo Lim, Sun-Hee Park
Kidney Research and Clinical Practice.2024; 43(1): 8. CrossRef - Associations between Chronic Kidney Disease and Migraine Incidence: Findings from a Korean Longitudinal Big Data Study
Mi Jung Kwon, Jwa-Kyung Kim, Min-Jeong Kim, Dae Myoung Yoo, Na-Eun Lee, Kyeong Min Han, Nan Young Kim, Ho Suk Kang, Hyo Geun Choi, Eun Soo Kim
Journal of Personalized Medicine.2024; 14(4): 356. CrossRef - Characteristics of Patients with Heart Failure and Advanced Chronic Kidney Disease (Stages 4–5) Not Undergoing Renal Replacement Therapy (ERCA-IC Study)
Sandra Valdivielso Moré, Miren Vicente Elcano, Anna García Alonso, Sergi Pascual Sanchez, Isabel Galceran Herrera, Francesc Barbosa Puig, Laia C. Belarte-Tornero, Sonia Ruiz-Bustillo, Ronald O. Morales Murillo, Clara Barrios, Joan Vime-Jubany, Nuria Farre
Journal of Clinical Medicine.2023; 12(6): 2339. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite



