Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 53(3); 2020 > Article
-
Special Section: COVID-19Brief Report
The Delay in Confirming COVID-19 Cases Linked to a Religious Group in Korea -
Hyung-Ju Kim
 , Hyun-Seong Hwang
, Hyun-Seong Hwang , Yong-Hyuk Choi
, Yong-Hyuk Choi , Hye-Yeon Song
, Hye-Yeon Song , Ji-Seong Park
, Ji-Seong Park , Chae-Young Yun
, Chae-Young Yun , Sukhyun Ryu
, Sukhyun Ryu
-
Journal of Preventive Medicine and Public Health 2020;53(3):164-167.
DOI: https://doi.org/10.3961/jpmph.20.088
Published online: April 8, 2020
Department of Preventive Medicine, Konyang University College of Medicine, Daejeon, Korea
- Corresponding author: Sukhyun Ryu, MD, PhD Department of Preventive Medicine, Konyang University College of Medicine, 158 Gwanjeodong-ro, Seogu, Daejeon 35365, Korea E-mail: gentryu@onehealth.or.kr
Copyright © 2020 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- As of March 3, 2020, the Shincheonji religious group accounted for the majority of Korean cases of coronavirus disease 2019 (COVID-19). Nonetheless, the most likely cause of the broad spread of COVID-19 among members of the Shincheonji religious group remains largely unknown.
-
Methods
- We obtained data of laboratory-confirmed cases related to the Shincheonji religious group from press releases by Korean public health authorities and news reports. We measured the period from the date of illness onset to the date of COVID-19 confirmation.
-
Results
- We analysed data from 59 cases (median age, 30 years). The estimated median period between the date of symptom onset and the date of COVID-19 confirmation was 4 days (95% confidence interval, 1-12).
-
Conclusions
- There was a delay in COVID-19 confirmation from the date of illness onset among the cases linked to the Shincheonji religious group. This delay likely contributed to the occurrence of many cases of COVID-19 in the group.
- On January 20, 2020, the first case of coronavirus disease 2019 (COVID-19) in Korea was identified in a Chinese person who travelled from Wuhan, China [1]. On February 18, 2020, the first case related to the Shincheonji religious group in Daegu was identified, following which massive contact tracing with an active screening program was implemented for that group. As the number of laboratory-confirmed cases of COVID-19 increased among members of the Shincheonji religious group, the Korean public health authorities announced a serious crisis alert on February 23, 2020. As of March 3, 2020, Korea had the second highest number of confirmed cases of COVID-19 following China.
- Given the high proportion of cases related to the Shincheonji religious group among all Korean cases (2992 of 5621 as of March 3, 2020) [2], we conducted a preliminary investigation of the time delay from illness onset to COVID-19 confirmation among members of the group.
INTRODUCTION
- Data Sources
- Data were obtained from the daily COVID-19 situation reports from the Korea Centers for Disease Control and Prevention, municipal or provincial departments of public health, and from news reports [2]. The epidemiological information of interest included cases’ year of birth, sex, date of illness onset, and origin of infection, including contact history with other laboratory-confirmed cases. We excluded cases with no reported symptoms and cases not linked to the Shincheonji religious group. We extracted data on laboratory-confirmed cases using a structured data-extraction form.
- Statistical Analysis
- We constructed epidemic curves using the date of illness onset and the date of COVID-19 confirmation. Furthermore, we estimated the time delay between the date of illness onset and the date of COVID-19 confirmation by fitting log-normal, gamma, and Weibull distributions using the available data [3]. We identified probabilistic distribution models and evaluated the suitability of the distribution models through the Bayesian information criterion (BIC) prior to the statistical analysis [4,5]. All statistical analyses were performed using R version 3.0.2 (https://cran.r-project.org/) and the R package “MASS” was used to identify the best model fit.
- Ethics Statement
- The need for ethical approval for this study was not necessary, based on the Enforcement Rule of Bioethics and Safety Act No. 13.
METHODS
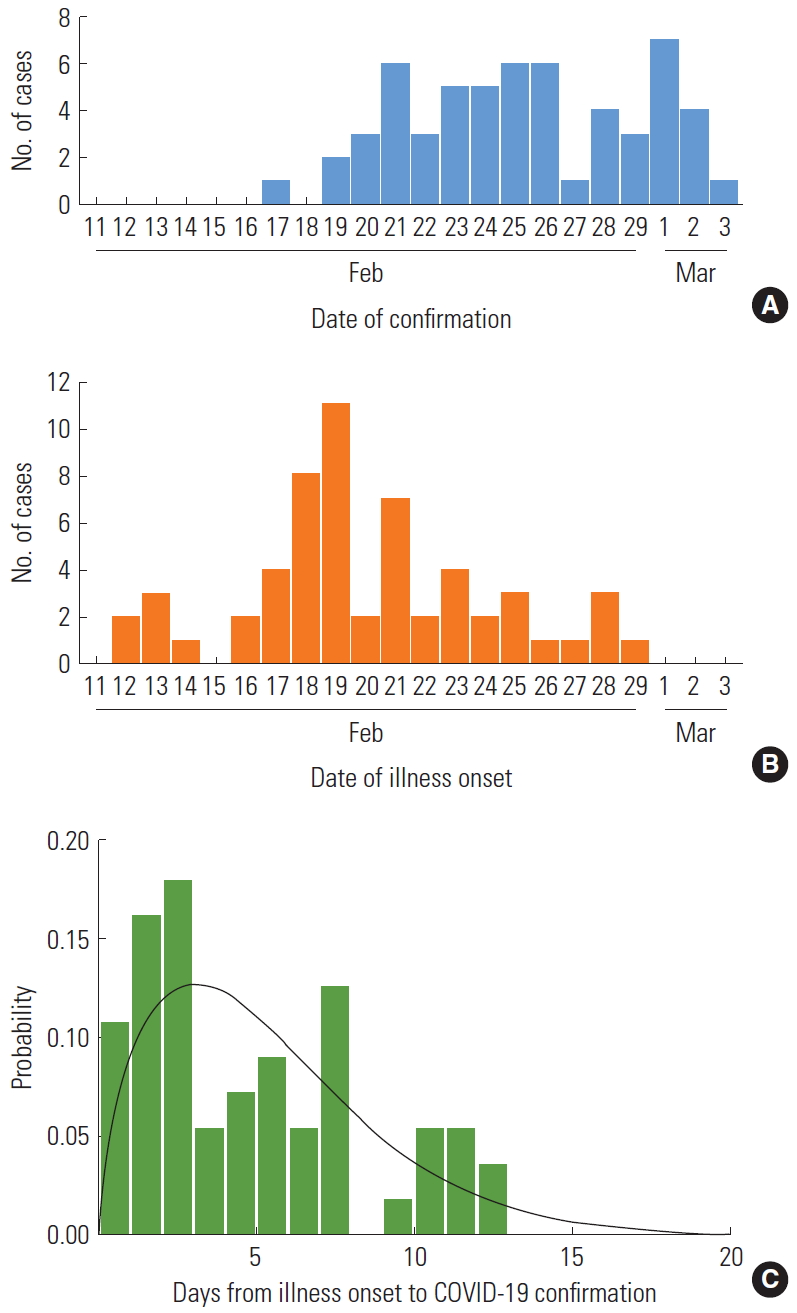
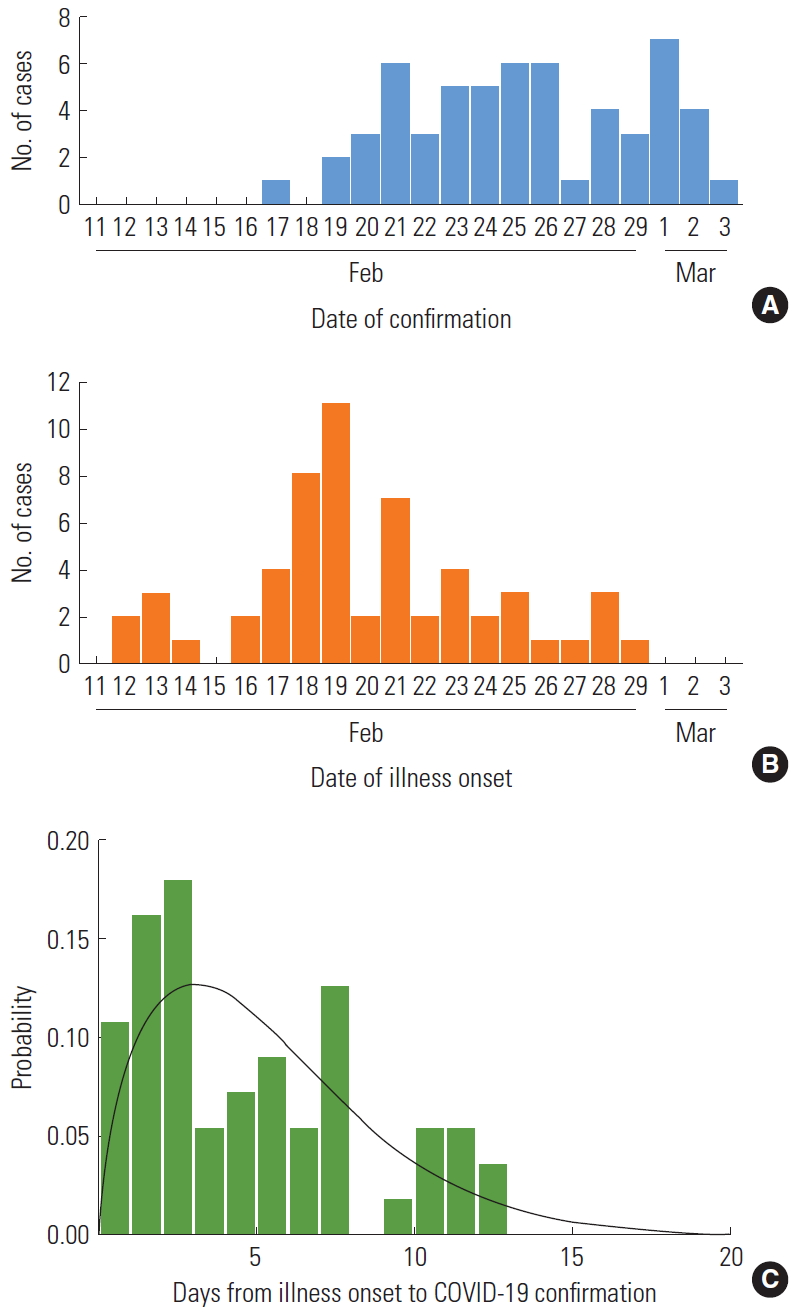
- We obtained a publicly available line list of 57 laboratory-confirmed cases reported between February 20, 2020 and March 3, 2020. The number of cases, as assessed by the date of illness onset, peaked on February 19, 2020 and decreased thereafter (Figure 1A, 1B). Twenty-four cases (42.1%) were male, and the mean age was 37 years (range, 14-77) (Table 1).
- Overall, symptoms were reported in 51 cases. The reported symptoms included cough (23 cases; 45.0% of the sample population), fever (12 cases; 23.5%), sore throat (12 cases; 23.5%), myalgia (11 cases; 21.6%), headache (2 cases; 3.9%), rhinorrhoea (2 cases; 3.9%), and chill (2 cases; 3.9%). The average period between the date of illness onset and the date of COVID-19 confirmation was 5.2 days, with a median of 4 days (range, 0-13).
- The period of time delay was best fit by the gamma distribution (BIC=292.7). Based on our model fit to the distribution, the estimated mean time delay was 5.3 days, with a 95% confidence interval of 1.0 -12.4 days (Figure 1C, Table 2).
RESULTS
- We investigated the cases of COVID-19 related to the Shincheonji religious group in Korea. In the secretive Shincheonji religious group, it is believed that the group’s founder and leader can interpret the secret metaphors in the Holy Bible [6]. The members of the group believe that their spirit and bodies are immortal [7]. This belief may have led to their behaviour of not approaching public health authorities when they had COVID-19-related symptoms (e.g., fever or cough) and to their uncooperative attitude towards epidemiological investigations [8]. This is likely to have contributed to the delayed confirmation of cases, despite the massive nationwide public health campaign regarding COVID-19 that was implemented in early February 2020. A previous study demonstrated that early detection of possible cases and prompt interventions are important to help preventing a large number of cases [9]. Therefore, this delay may have resulted in the broad spread of COVID-19 related to the Shincheonji religious group. In this group, worshippers kneel on the floor and hold worship services with a distance of about 10 cm between worshippers. Furthermore, they usually share lunch boxes after the worship [10,11]. Therefore, the method of worship may have also contributed to the transmission of COVID-19.
- In our study, fever and cough were the most common symptoms, which is consistent with findings of previous studies conducted in China [12,13]. However, the proportion of cases having fever or cough was lower than that in a previous study of hospitalised patients.
- In response to the surge of cases of COVID-19 related to the Shincheonji religious group, the Korean National Assembly approved the Corona Three Act on February 26, 2020 [14]. This act encoded revisions of the Korean laws on infection prevention, quarantine, and medicine; specifically, the regulations regarding cases of infectious diseases were revised to mandate testing and quarantining of individuals suspected of having COVID-19 by national law. The enactment of the Corona Three Act was a significant event in Korea in that it was the first pangovernmental measure to prevent the spread of infectious diseases.
- Our study is the first to analyse the confirmed cases of COVID-19 related to the Shincheonji religious group in Korea, which accounts for the largest proportion of cases of COVID-19 in Korea. However, the cases in our study are a sample collected from the publicly available data related to the Shincheonji religious group, which may have affected the study results. The date of illness onset may differ from the actual date of symptom onset as the data was based on each patient’s memory; therefore, it should be noted that this factor may have led to recall bias in our study.
- In conclusion, using publicly available data, we estimated a mean delay of 5 days between illness onset to isolation of COVID-19 cases among a religious group in Korea. Additional studies to measure the time interval between symptom onset and isolation of cases among different clusters of COVID-19 are needed to help to evaluate the effectiveness of public health interventions against the spread of COVID-19 in the community.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Conceptualization: SR. Methodology: SR. Formal analysis: HJK, HSH, SR. Data curation: HJK, HSH, YHC, HYS, JSP, CYY. Funding acquisition: None. Validation: SR. Writing - original draft preparation: HJK, HSH, YHC, HYS, JSP, CYY, SR. Writing - review and editing: SR.
Notes
| Characteristics | n (%) |
|---|---|
| Sex | |
| Male | 24 (42.1) |
| Female | 33 (57.9) |
| Age (y) | |
| 10-19 | 4 (7.0) |
| 20-29 | 26 (45.6) |
| 30-39 | 4 (7.0) |
| 40-49 | 9 (15.8) |
| 50-59 | 8 (14.0) |
| 60-69 | 5 (8.8) |
| 70-79 | 1 (1.7) |
|
Estimated distribution |
|||
|---|---|---|---|
| Weibull | Log-normal | Gamma | |
| Mean±SD (95% CI) | 5.3±1.5 (0.8, 12.0) | 5.5±4.8 (1.2, 14.4) | 5.3±3.7 (1.0, 12.4) |
| BIC | 293.0 | 294.6 | 292.7 |
- 1. Ryu S, Chun BC; Korean Society of Epidemiology 2019-nCoV Task Force Team. An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol Health 2020;42: e2020006ArticlePubMedPMCPDF
- 2. Korea Centers for Disease Control and Prevention. Press release: the updates on COVID-19 in Korea. [cited 2020 Mar 16]. Available from: https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030
- 3. Nishiura H. Early efforts in modeling the incubation period of infectious diseases with an acute course of illness. Emerg Themes Epidemiol 2007;4: 2ArticlePubMedPMCPDF
- 4. Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill 2015;20(25):7-13ArticlePubMed
- 5. Nishiura H. Determination of the appropriate quarantine period following smallpox exposure: an objective approach using the incubation period distribution. Int J Hyg Environ Health 2009;212(1):97-104ArticlePubMed
- 6. Tan L. Shincheonji members helped believer “escape” family. NZME; 2017 Apr 4 [cited 2020 Mar 16]. Available from: https://www.nzherald.co.nz/nz/news/article.cfm?c_id=1&objectid=11817395
- 7. Ahn S. Criticism of Shincheonji doctrine [dissertation]. Seoul: Chongshin University; 2017. (Korean)
- 8. Borowiec S. How South Korea’s coronavirus outbreak got so quickly out of control. TIME; 2020 Feb 24 [cited 2020 Mar 16]. Available from: https://time.com/5789596/south-korea-coronavirus-outbreak/
- 9. Ryu S, Kim BI, Chun BC. An outbreak of respiratory tract infection due to Respiratory Syncytial Virus-B in a postpartum center. J Infect Chemother 2018;24(9):689-694ArticlePubMed
- 10. Hancocks P, Seo Y. How novel coronavirus spread through the Shincheonji religious group in South Korea. CNN; 2020 Feb 28 [cited 2020 Mar 16]. Available from: https://edition.cnn.com/2020/02/26/asia/shincheonji-south-korea-hnk-intl/index.html
- 11. Choi W. “Sit too closely” unique worship contribue the superspread. TV Chosun; 2020 Feb 20 [cited 2020 Mar 16]. Available from: http://news.tvchosun.com/site/data/html_dir/2020/02/20/2020022090106.html (Korean)
- 12. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382(18):1708-1720ArticlePubMed
- 13. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395(10223):507-513ArticlePubMedPMC
- 14. Koh J. What is corona three act. Dongascience; 2020 Feb 26 [cited 2020 Mar 16]. Available from: http://dongascience.donga.com/news.php?idx=34612 (Korean)
REFERENCES
Figure & Data
References
Citations

- Outbreaks of COVID-19 in indoor places of worship: a systematic review
F Bert, G Lo Moro, A Peano, C Previti, R Siliquini
Perspectives in Public Health.2024; 144(2): 86. CrossRef - Healthcare policies, precautionary measures and outcomes of mass gathering events in the era of COVID-19 pandemic: Expedited review
Ahmed A. Alahmari, Anas A. Khan, Fahad A. Alamri, Yasir S. Almuzaini, Alia K. Habash, Hani Jokhdar
Journal of Infection and Public Health.2024; 17: 27. CrossRef - Does social empathy moderate fear-induced minority blaming during the COVID-19 pandemic?
Nari Yoo, Sou Hyun Jang
Social Science & Medicine.2024; 346: 116719. CrossRef - The Role of Religious Belief in COVID-19 Vaccine Hesitancy
Muzzamel Hussain Imran, Xin Leng, Mujahid Iqbal
Pastoral Psychology.2024;[Epub] CrossRef - The impact of the COVID-19 pandemic on the rehabilitation therapy of children and adolescents with cerebral palsy: a nationwide, health insurance data-based study
Jieun Shin, Mi Jin Hong, Jong Bum Park, Yung Jin Lee
Frontiers in Public Health.2024;[Epub] CrossRef - Evidence for transmission of SARS-CoV-2 at religious mass gatherings: A systematic review
Ndiaw Goumballa, Van Thuan Hoang, Jaffar A. Al-Tawfiq, Cheikh Sokhna, Philippe Gautret
New Microbes and New Infections.2024; 60-61: 101442. CrossRef - COVID-19 outbreak in a religious village community in Republic of Korea and risk factors for transmission
Jiae Shim, Eunju Lee, Eunyoung Kim, Yeonhwa Choi, Giseok Kang, Bryan Inho Kim
Osong Public Health and Research Perspectives.2023; 14(2): 110. CrossRef - Bridging science and spirituality: the intersection of religion and public health in the COVID-19 pandemic
Shahana Ayub, Gibson O. Anugwom, Tajudeen Basiru, Vishi Sachdeva, Nazar Muhammad, Anil Bachu, Maxwell Trudeau, Gazal Gulati, Amanda Sullivan, Saeed Ahmed, Lakshit Jain
Frontiers in Psychiatry.2023;[Epub] CrossRef - The impact of the COVID-19 pandemic on chlamydia infection in South Korea: a comparison between the pre-pandemic and during-pandemic periods
Achangwa Chiara, Sukhyun Ryu, Jae-Heon Jung, Se-Min Hwang
Frontiers in Public Health.2023;[Epub] CrossRef - Self-Quarantine Noncompliance During the COVID-19 Pandemic in South Korea
Sukhyun Ryu, Youngsik Hwang, Hongbi Yoon, Byung Chul Chun
Disaster Medicine and Public Health Preparedness.2022; 16(2): 464. CrossRef - The role of religion in mitigating the COVID-19 pandemic: the Malaysian multi-faith perspectives
Min Min Tan, Ahmad Farouk Musa, Tin Tin Su
Health Promotion International.2022;[Epub] CrossRef - Serial Intervals and Case Isolation Delays for Coronavirus Disease 2019: A Systematic Review and Meta-Analysis
Sheikh Taslim Ali, Amy Yeung, Songwei Shan, Lin Wang, Huizhi Gao, Zhanwei Du, Xiao-Ke Xu, Peng Wu, Eric H Y Lau, Benjamin J Cowling
Clinical Infectious Diseases.2022; 74(4): 685. CrossRef - “A Divine Infection”: A Systematic Review on the Roles of Religious Communities During the Early Stage of COVID-19
Mikyung Lee, Heejun Lim, Merin Shobhana Xavier, Eun-Young Lee
Journal of Religion and Health.2022; 61(1): 866. CrossRef - Perceptions and Behaviors of Patients with Inflammatory Bowel Disease during the COVID-19 Crisis
Yoo Jin Lee, Kyeong Ok Kim, Min Cheol Kim, Kwang Bum Cho, Kyung Sik Park, Byeong Ik Jang
Gut and Liver.2022; 16(1): 81. CrossRef - The impact of contact tracing and testing on controlling COVID-19 outbreak without lockdown in Hong Kong: An observational study
Hsiang-Yu Yuan, Colin Blakemore
The Lancet Regional Health - Western Pacific.2022; 20: 100374. CrossRef - Early warning of a COVID-19 surge on a university campus based on wastewater surveillance for SARS-CoV-2 at residence halls
Yuke Wang, Pengbo Liu, Haisu Zhang, Makoto Ibaraki, Jamie VanTassell, Kelly Geith, Matthew Cavallo, Rebecca Kann, Lindsay Saber, Colleen S. Kraft, Morgan Lane, Samuel Shartar, Christine Moe
Science of The Total Environment.2022; 821: 153291. CrossRef - Association of Angiotensin Receptor Blockers With the Risk of COVID-19 in Korea
Dong-Hyuk Cho, Jimi Choi, Jun Gyo Gwon
CardioMetabolic Syndrome Journal.2022; 2(1): 60. CrossRef - The COVID-19 pandemic, an environmental neurology perspective
J. Reis, A. Buguet, G.C. Román, P.S. Spencer
Revue Neurologique.2022; 178(6): 499. CrossRef - Clinical Time Delay Distributions of COVID-19 in 2020–2022 in the Republic of Korea: Inferences from a Nationwide Database Analysis
Eunha Shim, Wongyeong Choi, Youngji Song
Journal of Clinical Medicine.2022; 11(12): 3269. CrossRef - Healthcare Workforce Response to The Coronavirus Disease Outbreak in Daegu, Korea: A Multi-Center, Cross-Sectional Survey
Hyun Hee Kwon, Hye In Kim, Ki Tae Kwon, Soyoon Hwang, Shin-Woo Kim, Yoonjung Kim, Hyun ah Kim, Miri Hyun, Hyo-Lim Hong, Min Jung Kim, Jian Hur, Kyung Soo Hong
Infection & Chemotherapy.2022; 54(2): 298. CrossRef - Religion, politics and COVID-19 risk perception among urban residents in Malawi
Emmanuel Chilanga, Mastano Dzimbiri, Patrick Mwanjawala, Amanda Keller, Ruth Agather Mbeya
BMC Public Health.2022;[Epub] CrossRef - New Zealand Religious Community Responses to COVID-19 While Under Level 4 Lockdown
Theis Oxholm, Catherine Rivera, Kearly Schirrman, William James Hoverd
Journal of Religion and Health.2021; 60(1): 16. CrossRef - Impact of comorbidity burden on mortality in patients with COVID-19 using the Korean health insurance database
Soo Ick Cho, Susie Yoon, Ho-Jin Lee
Scientific Reports.2021;[Epub] CrossRef - Transmission dynamics and control of two epidemic waves of SARS-CoV-2 in South Korea
Sukhyun Ryu, Sheikh Taslim Ali, Eunbi Noh, Dasom Kim, Eric H. Y. Lau, Benjamin J. Cowling
BMC Infectious Diseases.2021;[Epub] CrossRef - A Well-Structured Follow-Up Program is Required after Recovery from Coronavirus Disease 2019 (COVID-19); Release from Quarantine is Not the End of Treatment
Keun-Mi Lee, Hae-Jin Ko, Geon Ho Lee, A-Sol Kim, Dong-Wook Lee
Journal of Clinical Medicine.2021; 10(11): 2329. CrossRef - Preparedness for containing COVID-19 outbreak in mass religious gathering with non-pharmaceutical interventions (NPIs)
Chen-Yang Hsu, Ya-Mei Chen, Chiu-Wen Su, Mei-Sheng Ku, Yeol Kim, Tim Jensen, Dih-Ling Luh
Journal of the Formosan Medical Association.2021; 120: S57. CrossRef - Temporal Changes in the Risk of Superspreading Events of Coronavirus Disease 2019
Jun-Sik Lim, Eunbi Noh, Eunha Shim, Sukhyun Ryu
Open Forum Infectious Diseases.2021;[Epub] CrossRef - Effect of Non-lockdown Social Distancing and Testing-Contact Tracing During a COVID-19 Outbreak in Daegu, South Korea, February to April 2020: A Modeling Study
Yi-Hsuan Chen, Chi-Tai Fang, Yu-Ling Huang
International Journal of Infectious Diseases.2021; 110: 213. CrossRef - Finding disease outbreak locations from human mobility data
Frank Schlosser, Dirk Brockmann
EPJ Data Science.2021;[Epub] CrossRef - The Priority of the Church’s Ministry during a Pandemic
Ardi Raharjo Sastrohartoyo, Rubin Adi Abraham, Jantje Haans, Tjahyadi Chandra
Evangelikal: Jurnal Teologi Injili dan Pembinaan Warga Jemaat.2021; 5(2): 164. CrossRef - Suppression of an Outbreak of COVID-19 without Lockdown: The Challenge of Inefficient Contact Tracing and Testing
Hsiang-Yu Yuan, Colin Blakemore
SSRN Electronic Journal .2021;[Epub] CrossRef - Estimation of the Excess COVID-19 Cases in Seoul, South Korea by the Students Arriving from China
Sukhyun Ryu, Sheikh Taslim Ali, Jun-Sik Lim, Byung Chul Chun
International Journal of Environmental Research and Public Health.2020; 17(9): 3113. CrossRef - Asymptomatic transmission of SARS‐CoV‐2 and implications for mass gatherings
Justin Wong, Sirajul Adli Jamaludin, Mohammad Fathi Alikhan, Liling Chaw
Influenza and Other Respiratory Viruses.2020; 14(5): 596. CrossRef - Incubation period of the coronavirus disease 2019 (COVID-19) in Busan, South Korea
Hansol Lee, Kyungtae Kim, Kwonkyu Choi, Sangbum Hong, Hyunjin Son, Sukhyun Ryu
Journal of Infection and Chemotherapy.2020; 26(9): 1011. CrossRef - Hajj and Umrah Mass Gatherings and COVID-19 Infection
Van-Thuan Hoang, Philippe Gautret, Ziad A. Memish, Jaffar A. Al-Tawfiq
Current Tropical Medicine Reports.2020; 7(4): 133. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite