Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 46(4); 2013 > Article
-
Original Article
Use of Drug-eluting Stents Versus Bare-metal Stents in Korea: A Cost-minimization Analysis Using Population Data - Hae Sun Suh1,2, Hyun Jin Song1,3, Eun Jin Jang1, Jung-Sun Kim4, Donghoon Choi1,4, Sang Moo Lee1
-
Journal of Preventive Medicine and Public Health 2013;46(4):201-209.
DOI: https://doi.org/10.3961/jpmph.2013.46.4.201
Published online: July 31, 2013
1National Evidence-based Healthcare Collaborating Agency, Seoul, Korea.
2College of Pharmacy and Yonsei Institute of Pharmaceutical Sciences, Yonsei University, Incheon, Korea.
3School of Pharmacy, Sungkyunkwan University, Suwon, Korea.
4Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea.
- Corresponding author: Sang Moo Lee, MD, PhD. 174 Yulgok-ro, Jongno-gu, Seoul 110-450, Korea. Tel: +82-2-2174-2850, Fax: +82-2-741-7060, lsmlight@daum.net
Copyright © 2013 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- The goal of this study was to perform an economic analysis of a primary stenting with drug-eluting stents (DES) compared with bare-metal stents (BMS) in patients with acute myocardial infarction (AMI) admitted through an emergency room (ER) visit in Korea using population-based data.
-
Methods
- We employed a cost-minimization method using a decision analytic model with a two-year time period. Model probabilities and costs were obtained from a published systematic review and population-based data from which a retrospective database analysis of the national reimbursement database of Health Insurance Review and Assessment covering 2006 through 2010 was performed. Uncertainty was evaluated using one-way sensitivity analyses and probabilistic sensitivity analyses.
-
Results
- Among 513 979 cases with AMI during 2007 and 2008, 24 742 cases underwent stenting procedures and 20 320 patients admitted through an ER visit with primary stenting were identified in the base model. The transition probabilities of DES-to-DES, DES-to-BMS, DES-to-coronary artery bypass graft, and DES-to-balloon were 59.7%, 0.6%, 4.3%, and 35.3%, respectively, among these patients. The average two-year costs of DES and BMS in 2011 Korean won were 11 065 528 won/person and 9 647 647 won/person, respectively. DES resulted in higher costs than BMS by 1 417 882 won/person. The model was highly sensitive to the probability and costs of having no revascularization.
-
Conclusions
- Primary stenting with BMS for AMI with an ER visit was shown to be a cost-saving procedure compared with DES in Korea. Caution is needed when applying this finding to patients with a higher level of severity in health status.
- Primary percutaneous coronary intervention has been established as the treatment of choice for patients with acute ST-segment elevation myocardial infarction (STEMI) which is a sub-class of acute myocardial infarction (AMI) and usually requires an immediate intervention [1]. Patients with STEMI usually admitted through an emergency room (ER) visit. The use of bare-metal stents (BMS) has been associated with improved clinical outcomes by reducing the risk of reocclusion and reinfarction compared with balloon angioplasty [2]. However, the risk of restenosis remains higher with the use of BMS, and the use of drug-eluting stents (DES) is expected to reduce restenosis [3].
- In a recent meta-analysis of 14 randomized controlled trials involving 7654 patients with STEMI, the use of DES significantly reduced revascularization compared with the use of BMS without increasing mortality or stent thrombosis [4]. DES, which were introduced in 2003, are more often used relative to BMS in South Korea compared with other countries, and DES have a higher purchase cost than BMS. Half a decade has passed since DES were introduced, and there is a need to weigh the clinical benefits of DES versus BMS against the related real-world costs.
- For this reason, the objective of this study is to perform an economic analysis of DES compared with BMS in patients with AMI admitted through an ER visit from the perspective of the Korean health care system using real-world data. We aim to evaluate the comparative value of DES and BMS given the higher purchase cost of DES and lower probability of having revascularization after inserting DES vs. BMS.
INTRODUCTION
- Model Overview
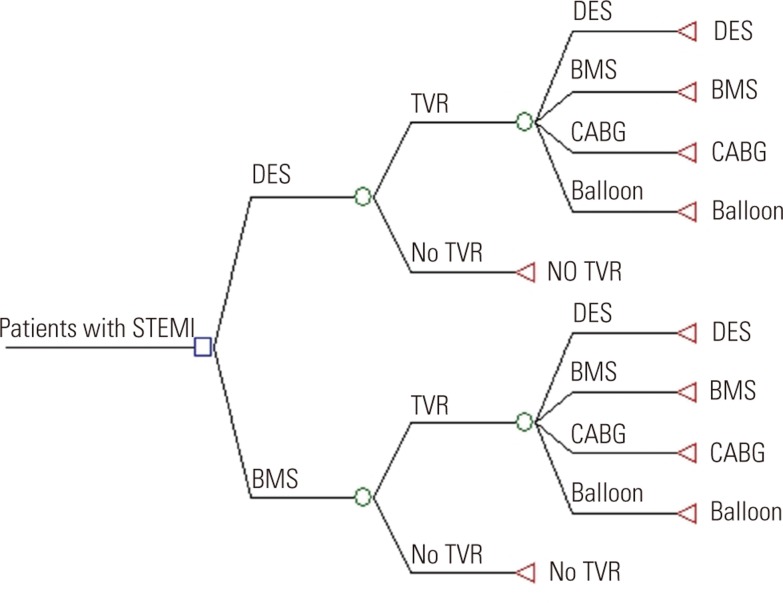
- This analysis modeled the clinical pathways of patients with AMI admitted through ER visits and receiving DES or BMS to estimate total incremental costs between the use of DES and BMS using a decision analytic model (Figure 1). We assumed that any repeat intervention within one year of the original stenting procedure was due to restenosis. The target population was patients with AMI admitted through ER visits who had received stents for the first time, who can be presumed to have experienced STEMI. We used a cost-minimization approach because the mortality, which is a major clinical outcome in this population, was not significantly different between the use of DES and BMS based on a meta-analysis in a recent systematic review. This meta-analysis with 7654 patients from 14 randomized clinical trials found that the primary clinical outcome of death was not significantly different between patients using DES and those using BMS for STEMI (relative risk [RR], 0.88; 95% confidence interval [CI], 0.70 to 1.10) [4]. We employed a societal perspective and used a two-year time period to reflect the data and trends more realistically although most STEMI patients require an emergency procedure and revascularization occurs within one year. The outcome measure was a cost difference in 2011 Korean won (KRW) currency.
- Claims Database Analyses
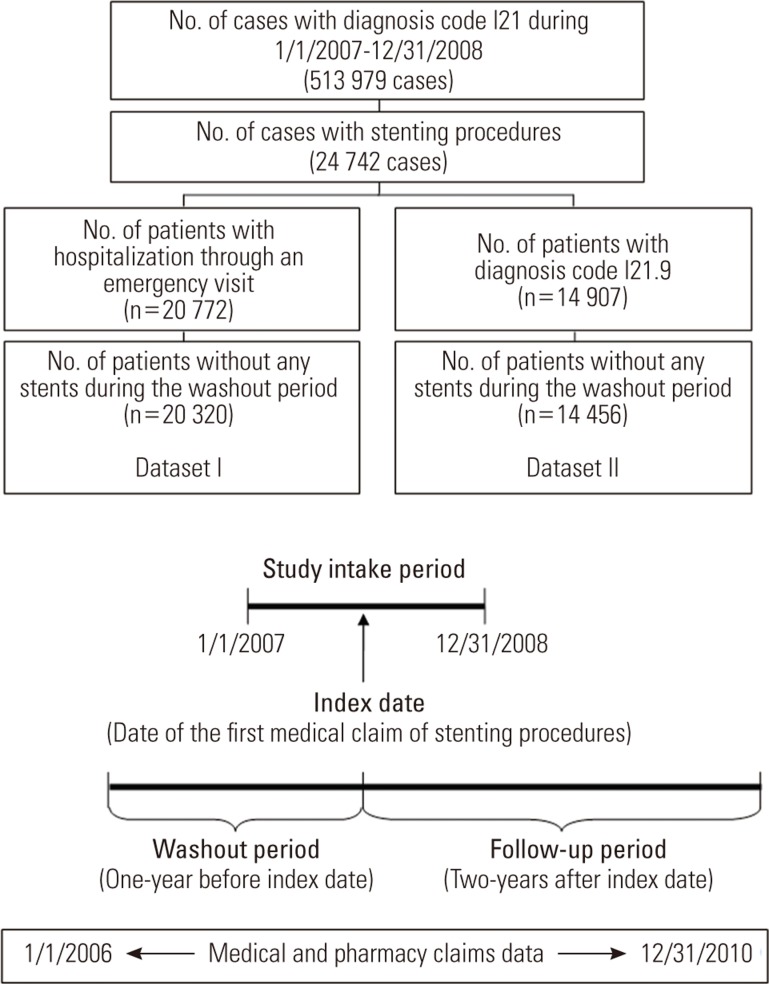
- To derive the costs and probabilities of the model parameters, we analyzed the Health Insurance Review and Assessment (HIRA) claims database, which is the national claims database. All of the records between January 1, 2006 and December 30, 2010 were extracted for all of the patients who had a diagnosis of AMI during a two-year intake period between January 1, 2007 and December 31, 2008. We had a one-year washout period, a two-year study intake period, and a two-year follow-up period (Figure 2). Identification of subjects with AMI was based on the International Classification of Diseases, tenth revision, clinical modification (ICD-10-CM) billing codes of I21. We used both procedure codes (M6551-2, M6561-4, M6601-5, and M6611-3 for stenting procedure) and material codes (J5083 for DES; J5231 and J5232 for BMS) to identify patients with AMI who received different types of stents during the intake period. The date of the first claim of stenting between January 2007 and December 2008 was defined as the index date. The stent naïve patients were defined as patients who did not receive stents during the one-year washout period before the index date. We excluded patients who received both DES and BMS for revascularization. Because there were no specific diagnosis codes for STEMI, we defined STEMI patients by identifying patients with AMI who were hospitalized through an emergency visit or had claims for emergency management (AC101, AC103, and AC105) based on consultation with clinical experts (dataset I). We also identified STEMI patients using the diagnosis code for "unspecified acute myocardial infarction" (ICD-10 code: 21.9), as some major general hospitals used this code for STEMI patients. We used this group as a separate dataset (dataset II) to check the robustness of the economic analysis results as part of our sensitivity analyses.
- The institutional review board of the National Evidence-based Healthcare Collaborating Agency approved the study and waived the need for consent because the researchers used existing data from which subjects cannot be identified directly or through identifiers linked to the subjects.
- Estimating Probabilities of Model Parameters
- We estimated the probabilities of model parameters from population-based data and a systematic review performed previously. The technical details of this systematic review are fully described in another article [4]. The probabilities of target vessel revascularization were derived from a previous meta-analysis comparing DES with BMS in STEMI patients in randomized controlled trials (RR, 0.48; 95% CI, 0.41 to 0.56). We performed a separate analysis to reflect the real world outcome in Korea using a large-scale observational study comparing DES with BMS in patients with STEMI (hazard ratio at year 1, 0.15; 95% CI, 0.08 to 0.30) [5].
- The probabilities of recurrent procedures of DES, BMS, coronary artery bypass graft (CABG), and balloon angioplasty were estimated from claims that occurred within one year after the initial stenting at the index date. We used procedure codes to identify these four procedures (O1641-2, OA641-2, O1647, OA647, O0161-9, and O0170-1 for CABG; M6593-7 for balloon angioplasty). The probabilities of transitioning from DES to DES (group I), from DES to BMS (group II), DES to CABG (group III), DES to balloon (group IV), BMS to DES (group V), BMS to BMS (group VI), BMS to CABG (group VII), and BMS to balloon (group VIII) were estimated from a national claims database analysis.
- Estimating Costs of Model Parameters
- We estimated the costs of model parameters from population-based data for each group (group I to group VIII) and groups without revascularization after inserting DES or BMS. Thus, we estimated costs for ten groups in total. The two-year aggregate costs consisted of costs paid by national health insurance, copayments by patients, uninsured costs, and non-medical direct costs. Costs paid by national health insurance included costs related to surgery (DES, BMS, CABG, and balloon), hospitalization stays, tests before and after surgery, physician fees, medications such as anticoagulants administered before and after surgery, treatments for complications, and follow-up visits. For follow-up costs after the initial stenting procedure and before repeated procedures, we considered the costs incurred in certain specialty areas such as internal medicine, neurology, thoracic and cardiovascular surgery, diagnostic radiology, laboratory medicine, nuclear medicine, and emergency medicine.
- We computed uninsured costs based on a published report that presents the proportion of uninsured medical costs among the total medical costs spent in the disease area of cardiovascular disease including chronic rheumatic heart disease (ICD-10 code of I05-I09), hypertension (I10-I15), and ischemic heart disease (I20-I25). We used the uninsured proportion of medical and pharmacy costs in 2010 (19.9%) [6]. Non-medical direct costs included transportation costs for patients to visit hospitals. The total number of hospital visits was assumed to be the sum of one visit for admission, one visit within one month after surgery, and then one visit every three months based on clinical experts' opinion. We estimated transportation costs by multiplying the total number of hospital visits by the average round-trip transportation costs for admission (10 600 KRW) and outpatient visits (8600 KRW) in 2005 extrapolated to a 2011 value using the consumer price index in transportation (116.8 in 2009 based on 2005) [7,8]. If a patient gets revascularization, (s)he has to visit the hospital more often than a patient without revascularization (two inpatient visits and six outpatient visits for patients with revascularization; one inpatient visit and three outpatient visits for patients without revascularization). This resulted in the difference in the transportation costs between DES and BMS.
- Sensitivity and Sub-group Analyses
- We performed univariate sensitivity analyses for all cost and probability parameters of the model to determine the robustness of the model results. The range used for each cost parameter was based on the mean and standard deviation (SD) obtained from the claims database analysis. We used the mean value plus one SD as the upper limit and mean minus one SD as the lower limit. For each probability parameter, the range was based on 25% of the values in the base model. A multivariate sensitivity analysis using a probabilistic Monte Carlo simulation was also performed using gamma distributions for cost parameters and triangular distributions for probability parameters with 10 000 trials per simulation. The parameters of the gamma distributions were based on the mean and SD obtained from the claims database analysis. For triangular distributions, the likeliest values were based on the claims database analysis, and the minimum and maximum values were based on five clinical experts' opinion from three major hospitals in Korea. To check the robustness of the economic analysis results in terms of the way we defined STEMI patients in the claims database analysis, we used the results from dataset II and performed another set of an economic analyses. We also performed a sub-group analysis by restricting the analysis to patients who received only one stent to check the robustness of the economic analysis results, given the inability to adjust for the baseline severity of patients receiving DES and BMS. In this way, we were able to select patients who had a similar baseline disease severity and partly overcome the limitations of the claims database not containing clinical variables. This subgroup analysis was based on the assumption that the patients with more severe conditions would have more than two stents inserted. Analyses were performed using SAS statistical software version 9.2 (SAS Inc., Cary, NC, USA) and TreeAge Pro 2009 (TreeAge Software Inc., Williamstown, MA, USA).
METHODS
- Our base model estimates, the ranges of values used in the sensitivity analyses, and our data sources are presented in Table 1. We took the baseline efficacy parameter from a recent systematic review with a meta-analysis where the probabilities of the repeat target vessel revascularization for DES and BMS were 5.4% and 11.8%, respectively [4]. We used the HIRA database involving 24 742 stenting incident cases with a diagnosis code of AMI to obtain the rest of the parameter values for the base model. The mean lengths of hospitalization for repeated procedures with DES were 5.5 days (SD, 4.6 days; median, 4.0 days) in patients with initial DES and 5.1 days (SD, 4.3 days; median, 4.0 days) in patients with initial BMS. The ages at the index date did not differ significantly between the patients with initial DES (mean age with 62.0 years) and those with initial BMS (mean age with 62.8 years). Similarly, the proportion of gender was not significantly different between the two groups (p-value: 0.4556).
- From a societal perspective using dataset I, the two-year average cost for patients with initial DES use was 11 065 528 KRW/person. The two-year cost for those with initial BMS use was 9 647 647 KRW/person. The expected two-year cost per patient was 1 417 882 KRW higher for DES-treated patients compared with BMS-treated patients. As shown in Table 2, the majority of costs occurred in the first year after surgery. The proportion of second-year costs was 4.5% in patients with initial DES use and 5.4% in those with BMS. Notably, the second-year cost after surgery was slightly higher in patients with initial BMS use versus DES use, which was the opposite of the findings regarding the total costs and the first-year cost, but the difference in magnitude was trivial. When we performed a subgroup analysis including patients in whom only one stent was inserted in order to generate comparable patient groups, the two-year cost difference between DES and BMS decreased to 817 833 KRW/person (by about 42%) compared with the cost difference between the two groups in dataset I.
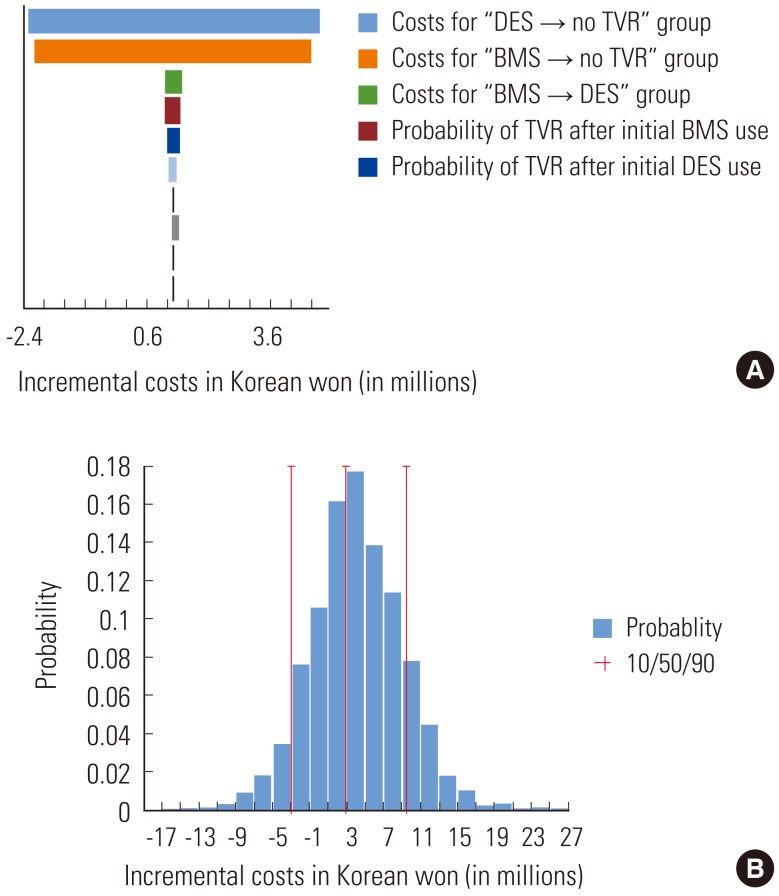
- As shown in the tornado diagram in Figure 3, the incremental costs between DES and BMS use were insensitive to varying probabilities of target vessel revascularization after the initial DES or BMS use and varying costs for different types of repeated procedures. However, this economic model was very sensitive to the incurred costs in patients without repeated procedures after the initial DES or BMS use. The qualitative conclusions of the results changed according to these costs. We also performed a multivariate sensitivity analysis using a probabilistic Monte Carlo simulation. Above the 19.5 percentile of the distribution of incremental costs, the use of DES to treat AMI admitted through an ER visit incurred higher costs compared with the use of BMS. The direction of cost differences between two stents became opposite below the 19.0 percentile of the distribution of incremental costs between DES and BMS.
RESULTS
- This economic analysis suggests that the use of DES compared with the use of BMS in patients with AMI admitted through ER visits in South Korea would lead to an increase in costs that would partially be offset by cost savings due to the reduced need for repeated revascularization given that the mortality after the use between DES and BMS is not different. We have conducted several sensitivity analyses and subgroup-analyses to check the robustness of our result. The result of the cost-saving option did not change by most of the parameters. However, the cost-saving option was highly sensitive to the incurred costs in patients without repeated procedures after the initial DES or BMS use. About 80% of the results from the probabilistic Monte Carlo simulation indicated that the use of BMS is the cost-saving option in patients with AMI admitted through ER visits.
- Several economic analyses have been conducted to examine the implications of the use of DES compared with the use of BMS in each country's healthcare system, including Canada, the United Kingdom, the United States of America, Italy, Switzerland, the Netherlands, Australia, and Belgium [3,9-11]. Few studies have concluded that the use of DES is cost-effective when compared with BMS, and most studies concluded that the use of DES is not cost-effective for all patients or lower risk groups, but is (or might be) cost-effective in some high-risk population such as patients with diabetes, small vessels, or long lesions. Unlike our study, these studies were not limited to patients with AMI.
- The strength of our analysis is that we used the real-world population-based data that covers almost all of the Korean population to derive parameter values of costs and transition probabilities in patients with AMI admitted through ER visits who had initial stenting procedures. The analysis was based on individual data reflecting real and contemporary practice. To get the estimates for stent naïve users, we used a one-year washout period. We defined patients with STEMI by using the diagnosis code of AMI cases who were hospitalized through an emergency department visit or had claims for emergency management due to the absence of codes for STEMI. Because there was an uncertainty in the way we defined STEMI patients, we used another approach to define STEMI patients (dataset II) and re-ran the entire economic analysis. Our results were robust regardless of the way we defined patients with STEMI.
- To overcome the limitation of using a claims database that does not include clinical variables, we performed a sub-group analysis by confining patients who received only one stent to produce comparable patient groups in terms of disease severity. As expected, the cost difference between patients with DES and those with BMS decreased by about 42% because patients in two groups became more homogeneous than patients with any number of stents inserted. However, the cost-saving option was still the BMS. Furthermore, we have run a separate analysis to reflect the real world data in Koreans by using the target vessel revascularization rate comparing DES and BMS in patients with STEMI from the study of Park et al. [5]. The cost-saving option appeared to be using BMS, but the magnitude of cost difference decreased by almost 50% when compared with the results from dataset I and II. This is because the hazard ratio of target vessel revascularization comparing DES and BMS was 0.15 (95% CI, 0.08 to 0.30) at year 1. The effectiveness of DES versus BMS was shown to be higher in Koreans with STEMI compared with the efficacy of DES versus BMS from randomized controlled trials in a Western population (RR, 0.48; 95% CI, 0.41 to 0.56) [4]. Several Korean studies [5,12-17] have investigated the outcomes of stents, but we used the Park et al. group's study result because it compared DES and BMS in a relatively large-scale group of STEMI patients. The other studies compared different types of DES or compared DES and BMS in specific patient groups (i.e., renal insufficiency) or overall patient groups (i.e., all AMI including STEMI). Although the magnitude of the cost difference between the two groups decreased by half, our results on the cost-saving option were robust in several subgroup analyses.
- Several limitations to this study need to be acknowledged. First, the study results carry the common limitations of claims data because the analyses are based on the national claims database. Clinical information about the types of blood vessel regions where stents were inserted (i.e., small vessels, long lesions), the level of severity, and whether the revascularization was due to stent restenosis were missing. Due to the absence of clinical variables, we were not able to define patient groups according to varying degrees of severity. To partly resolve this issue, we performed a sub-group analysis by focusing on patients who received only one stent. These patient groups would have higher probability of having a comparable disease risk and level of severity. In addition, because the patients who received only one stent might have less severity than the patients who received two stents or more, there is a possibility that the costs differences between patients with DES and those with BMS might not occur. The results showed that the cost-saving option was using BMS. Further studies are needed to find cost-saving options between DES and BMS in different types of high-risk groups who are prone to undergoing additional revascularizations and experiencing worse outcomes. In addition, there is a possibility that we might have included patients with NSTEMI (non ST-segment elevation myocardial infarction) in our analysis data because we did not have clinical data to identify patients with STEMI precisely. However, we performed a sensitivity analysis to define the patient population by the I21.9 code and the results were similar. This code is defined as the unspecified AMI and is often used as a code when patients have STEMI based on clinical experts' opinions from three major hospitals. Although we tried several approaches to identify STEMI patients, this limitation is difficult to overcome perfectly because we do not have clinical variables in the claims database. Second, in general, the validity issue of administrative database coding cannot be easily resolved because this database is constructed for reimbursement purposes and not for clinical purposes. However, the HIRA claims data has a higher reliability than any other data in Korea for estimating health care utilization and costs. The results from the HIRA data are generalizable and representative because the national claims data covers almost the whole population of Korea. Moreover, the accuracy of the diagnosis codes tend to be higher for claims of severe conditions than of mild conditions [18]. Third, we employed a cost-minimization approach because the major clinical outcome, which was mortality, was not significantly different between patients with DES and those with BMS based on the meta-analysis of randomized clinical trials. Other clinical outcomes such as target vessel revascularization or target lesion revascularization were significantly lower in patients with DES vs. BMS, which was reflected in the model [4,19]. Stent thrombosis was not significantly different between the two groups although there is some concern that DES might be associated with an increased risk of stent thrombosis over the long term [20,21]. Because the most important clinical outcome was mortality in this patient group, based on a discussion with clinical experts, we chose a cost-minimization approach over a cost-effectiveness or cost-utility approach, as suggested in the economic evaluation guideline by the Health Insurance Review and Assessment Service. However, caution is needed when choosing the cost-saving option between two stents because the results are based on the assumption that important clinical effects are not significantly different between the two stents. For example, the decreased rate of target vessel/lesion revascularization could be great benefit to a certain patient group. In this case, although the difference in revascularization probability is reflected in the model, the cost-utility approach might be needed to quantify the benefits of decreased revascularization in different ways, such as incorporating the improved health-related quality of life due to reduced target vessel revascularization after using DES compared with BMS. A carefully designed study deriving the utility of target vessel revascularization in a Korean population might be needed. Finally, we were not able to include the costs incurred in patients who used more than three stents. Currently, the government reimburses up to three stents used for patients. Thus, the HIRA data will only include the claims for the first three stents used. This means that our cost estimates might be underestimated.
- In conclusion, this economic analysis provides the best data available to date on the cost-saving option between DES and BMS in patients with AMI admitted through ER visits who are stent naïve users in Korea. The use of DES to treat AMI admitted through ER visits incurred higher costs compared with the use of BMS. Although this result was sensitive to the costs incurred in patients without repeated revascularizations after their initial stenting procedures, the use of BMS was shown to be the probable cost-saving option from the Monte Carlo simulation. Further studies are needed to examine the cost-saving options in different types of high-risk groups who are prone to having more revascularizations.
DISCUSSION
ACKNOWLEDGEMENTS
- 1. Kushner FG, Hand M, Smith SC Jr, King SB 3rd, Anderson JL, Antman EM, et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2009;120(22):2271-2306. 19923169ArticlePubMed
- 2. Nordmann AJ, Hengstler P, Leimenstoll BM, Harr T, Young J, Bucher HC. Clinical outcomes of stents versus balloon angioplasty in non-acute coronary artery disease. A meta-analysis of randomized controlled trials. Eur Heart J 2004;25(1):69-80. 14683745ArticlePubMed
- 3. Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al. Drug-eluting stents: a systematic review and economic evaluation. Health Technol Assess 2007;11(46):iii. xi-221. 17999841Article
- 4. Suh HS, Song HJ, Choi JE, Jang EJ, Son HJ, Lee SM, et al. Drug-eluting stents versus bare-metal stents in acute myocardial infarction: a systematic review and meta-analysis. Int J Technol Assess Health Care 2011;27(1):11-22. 21262083ArticlePubMed
- 5. Park KW, Kang SH, Chung WY, Lee HY, Park JS, Kang HJ, et al. 'Real world' comparison of drug-eluting stents vs bare metal stents in the treatment of unselected patients with acute ST-segment elevation myocardial infarction. Circ J 2010;74(6):1111-1120. 20453391ArticlePubMed
- 6. National Health Insurance Corporation. Examination of healthcare expenditure for patients with health insurance in 2010. Seoul: National Health Insurance Corporation; 2011. p. 172 (Korean)
- 7. Korea Centers for Disease Control and Prevention. The Korea National Health and Nutrition Examination Survey (KNHANES III). Seoul: Korea Centers for Disease Control and Prevention; 2005. p. 174. p. 177 (Korean)
- 8. Korean Statistical Information Service. Consumer price index in transportation. 2011. cited 2012 Nov 15. Available from: http://kosis.kr (Korean)
- 9. Lord SJ, Howard K, Allen F, Marinovich L, Burgess DC, King R, et al. A systematic review and economic analysis of drug-eluting coronary stents available in Australia. Med J Aust 2005;183(9):464-471. 16274347ArticlePubMedPDF
- 10. Neyt M, De Laet C, De Ridder A, Van Brabandt H. Cost effectiveness of drug-eluting stents in Belgian practice: healthcare payer perspective. Pharmacoeconomics 2009;27(4):313-327. 19485427ArticlePubMed
- 11. Ong AT, Daemen J, van Hout BA, Lemos PA, Bosch JL, van Domburg RT, et al. Cost-effectiveness of the unrestricted use of sirolimus-eluting stents vs. bare metal stents at 1 and 2-year follow-up: results from the RESEARCH Registry. Eur Heart J 2006;27(24):2996-3003. 17114234ArticlePubMed
- 12. Cho Y, Yang HM, Park KW, Chung WY, Choi DJ, Seo WW, et al. Paclitaxel-versus sirolimus-eluting stents for treatment of ST-segment elevation myocardial infarction: with analyses for diabetic and nondiabetic subpopulation. JACC Cardiovasc Interv 2010;3(5):498-506. 20488406ArticlePubMed
- 13. Kim KH, Koo BK, Min HS, Park SK, Kim CH, Park KW, et al. Comparison of drug-eluting versus bare-metal stent implantation in ST-elevation myocardial infarction patients with renal insufficiency: results from the national registry in Korea. Int J Cardiol 2012;154(1):71-77. 20888053ArticlePubMed
- 14. Park K, Park KW, Rha SW, Bae JH, Hur SH, Park JS, et al. Comparison of 5-year clinical outcomes between sirolimus-versus paclitaxel-eluting stent: Korean multicenter network analysis of 9000-patient cohort. Circ Cardiovasc Interv 2012;5(2):174-184. 22396583ArticlePubMed
- 15. Park KW, Cho YS, Chung JW, Yeon TJ, Chae IH, Choi DJ, et al. One year clinical and six month angiographic results of drug eluting stents for ST elevation acute myocardial infarction: 'real world' comparison between sirolimus- and paclitaxel-eluting stents. Int J Cardiol 2009;131(3):350-355. 18180056ArticlePubMed
- 16. Park KW, Lim WH, Kim JH, Kang SH, Seo JW, Song YB, et al. Comparison between zotarolimus-eluting stents and first generation drug-eluting stents in the treatment of patients with acute ST-segment elevation myocardial infarction. Int J Cardiol 2013;166(1):118-125. 22062892ArticlePubMed
- 17. Sim DS, Jeong MH, Ahn Y, Kim YJ, Chae SC, Hong TJ, et al. Effectiveness of drug-eluting stents versus bare-metal stents in large coronary arteries in patients with acute myocardial infarction. J Korean Med Sci 2011;26(4):521-527. 21468259ArticlePubMedPMC
- 18. Park BJ, Sung JH, Park KD, Seo SW, Kim SW. Strategies to improve the validity of diagnostic codes of National Health Insurance claims data. Seoul: Health Insurance Review and Assessment Services; 2002. p. vi. p. 118-119 (Korean)
- 19. Brar SS, Leon MB, Stone GW, Mehran R, Moses JW, Brar SK, et al. Use of drug-eluting stents in acute myocardial infarction: a systematic review and meta-analysis. J Am Coll Cardiol 2009;53(18):1677-1689. 19406344ArticlePubMed
- 20. Di Lorenzo E, Sauro R, Varricchio A, Carbone G, Cortese G, Capasso M, et al. Long-Term outcome of drug-eluting stents compared with bare metal stents in ST-segment elevation myocardial infarction: results of the paclitaxel- or sirolimus-eluting stent versus bare metal stent in Primary Angioplasty (PASEO) Randomized Trial. Circulation 2009;120(11):964-972. 19720939ArticlePubMed
- 21. Généreux P, Mehran R. Are drug-eluting stents safe in the long term? CMAJ 2009;180(2):154-155. 19106153ArticlePubMedPMC
REFERENCES
| Model parameters |
Types of initial stenting procedure |
Probabilistic model distribution | Source | |||||
|---|---|---|---|---|---|---|---|---|
|
DES |
BMS |
|||||||
| Values in base model |
Ranges for sensitivity analyses |
Values in base model |
Ranges for sensitivity analyses |
|||||
| Low | High | Low | High | |||||
| Probabilities (%) | ||||||||
| TVR | 5.4 | 4.1 | 6.8 | 11.8 | 8.8 | 14.7 | Triangular | [6] |
| DES | 59.7 | 44.8 | 74.6 | 50.9 | 38.1 | 63.6 | Triangular | HIRA claims data1 |
| BMS | 0.6 | 0.5 | 0.8 | 3.4 | 2.6 | 4.3 | Triangular | |
| CABG | 4.3 | 3.2 | 5.4 | 9.5 | 7.1 | 11.9 | Triangular | |
| Balloon | 35.3 | 26.5 | 44.2 | 36.2 | 27.2 | 45.3 | Triangular | |
| No TVR | 94.6 | 70.9 | 100.0 | 88.2 | 66.2 | 100.0 | Triangular | [6] |
| Costs2 (×103 KRW) | ||||||||
| TVR | HIRA claims data, [7,8,10] | |||||||
| DES | 16 952 | 13 115 | 20 790 | 16 718 | 10 787 | 22 650 | Gamma | |
| BMS | 16 415 | 13 209 | 19 620 | 13 422 | 10 798 | 16 047 | Gamma | |
| CABG | 31 290 | 20 281 | 42 299 | 25 559 | 19 372 | 31 746 | Gamma | |
| Balloon | 17 232 | 12 776 | 21 689 | 13 571 | 9779 | 17 364 | Gamma | |
| No TVR | 10 688 | 6667 | 14 710 | 8760 | 5361 | 12 159 | Gamma | |
DES, drug-eluting stents; BMS, bare-metal stents; TVR, target vessel revascularizations; CABG, coronary artery bypass graft; KRW, Korean won; HIRA, Health Insurance Review and Assessment; Balloon, balloon angioplasty.
1 HIRA claims database, which is population-based data that contains information on all medical and prescription drug claim records of the Korean population (results from dataset I are presented).
2 Two-year aggregate costs consisted of costs paid by national health insurance, copayments paid by patients, uninsured costs, and non-medical direct costs in 2011 KRW.
| Total costs incurred in patients with DES | Total costs incurred in patients with BMS | Cost difference between DES and BMS | |
|---|---|---|---|
| Dataset I (STEMI patients defined by ICD-10 code 21 with emergency visits) | |||
| Total of two years | 11 065 528 | 9 647 647 | 1 417 882 |
| 1st year | 10 884 425 | 9 463 717 | 1 420 708 |
| 2nd year | 495 111 | 519 644 | -24 532 |
| Dataset II (STEMI patients defined by ICD-10 code 21.9) | |||
| Total of two years | 10 955 336 | 9 464 538 | 1 490 798 |
| 1st year | 10 782 129 | 9 254 967 | 1 527 162 |
| 2nd year | 509 317 | 558 718 | -49 401 |
| Dataset I (subgroup analysis: patients inserted with only one stent) | |||
| Total of two years | 10 368 612 | 9 550 778 | 817 833 |
| 1st year | 10 181 185 | 9 375 947 | 805 239 |
| 2nd year | 505 721 | 507 601 | -1880 |
| Dataset I (using real-world data in Korean1) | |||
| Total of two years | 11 168 523 | 10 424 015 | 744 508 |
| 1st year | 10 962 470 | 10 116 455 | 846 015 |
| 2nd year | 537 937 | 746 531 | -208 594 |
Values are presented as KRW/person.
DES, drug-eluting stents; KRW, 2011 Korean won; BMS, bare-metal stents; STEMI, ST-segment elevation myocardial infarction; ICD-10, International Classification of Diseases tenth revision.
1 The rate of target vessel revascularization from Park et al. [5] was used.
Figure & Data
References
Citations

- A cost analysis comparing telepsychiatry to in-person psychiatric outreach and patient travel reimbursement in Northern Ontario communities
Eva Serhal, Tanya Lazor, Paul Kurdyak, Allison Crawford, Claire de Oliveira, Rebecca Hancock-Howard, Peter C Coyte
Journal of Telemedicine and Telecare.2020; 26(10): 607. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite




