Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 46(6); 2013 > Article
-
Original Article
The Economic Burden of Epilepsy in Korea, 2010 - Jaehun Jung1, Hye-Young Seo2, Young Ae Kim2, In-Hwan Oh3, Yo Han Lee1, Seok-Jun Yoon1
-
Journal of Preventive Medicine and Public Health 2013;46(6):293-299.
DOI: https://doi.org/10.3961/jpmph.2013.46.6.293
Published online: November 28, 2013
1Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea.
2Graduate School of Public Health, Korea University, Seoul, Korea.
3Department of Preventive Medicine, Kyung Hee University College of Medicine, Seoul, Korea.
- Corresponding author: Seok-Jun Yoon, MD, PhD. 145 Anam-ro, Seongbuk-gu, Seoul 136-701, Korea. Tel: +82-2920-6412, Fax: +82-2920-7220, yoonsj02@korea.ac.kr
• Received: April 15, 2013 • Accepted: September 16, 2013
Copyright © 2013 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- The purposes of this study were to evaluate the prevalence of epilepsy and to estimate the cost of epilepsy in Korea, 2010.
-
Methods
- This study used a prevalence based approach to calculate the cost of epilepsy. Claims data from the Korean national health insurance and data from the Korea health panel, the Korea National Statistical Office's records of causes of death, and labor statistics were used to estimate the cost of epilepsy. Patients were defined as those who were hospitalized or visited an outpatient clinic during 2010 with a diagnosis of epilepsy (International Classification of Diseases 10th revision codes G40-G41). Total costs of epilepsy included direct medical costs, direct non-medical cost and indirect costs.
-
Results
- The annual prevalence of treated epilepsy was 228 per 100 000 population, and higher in men. The age-specific prevalence was highest for teenagers. The total economic burden of epilepsy was 536 billion Korean won (KW). Indirect cost (304 billion KW) was 1.3 times greater than direct cost (232 billion KW). By gender, the male (347 billion KW) were more burdened than the female (189 billion KW). The estimated cost in young age younger than 20 years old was 24.5% of the total burden of epilepsy.
-
Conclusions
- A significant portion of the economic burden of epilepsy is borne by people in young age. To reduce the economic burden of epilepsy, effective prevention and treatment strategies are needed.
- The International League Against Epilepsy and the International Bureau for Epilepsy defined epilepsy as a disease of brain featured by a state causing at least one epileptic seizure continuously and its neurobiological, cognitive, psychological, and social results [1].
- The epilepsy is the second common disease among chronic nervous diseases next to the stroke, it is known that 3% to 5% of the whole population experiences convulsion during his/her lifetime [2] and it is assumed that there are over 50 million patients with the epilepsy in the world [3]. It has been reported that in the developed countries, prevalence of the epilepsy is 16 to 51 per 100 000 population and there was a trend that the prevalence was higher in an age group below 1 year old and during infancy, decreased gradually with increase of age, and started to increase again from 50 year old. On the other hand, it was reported that in the developing countries, the prevalence was 35 to 111 per 100 000 population and the tendency to increase again from 50 year old was not shown [4]. The prevalence of epilepsy was reported as 4 to 10 per 1000 population in most studies and higher in the developing countries compared that in the developed countries. It is known that at least 70% of patients with epilepsy can achieve long-term remission indicating a state without crisis of epilepsy for 5 years in receiving appropriate treatment [5]. However, morbidity of the patients with epilepsy increases and symptomatic epilepsy reduces life expectancy by 18 years at maximum [6]. In addition, the epilepsy develops relatively early and is accompanied with cognitive disorders and psychiatric and behavioral problems [3].
- For economic burden of epilepsy, it was reported that in United States, direct medical cost per year was 95 billion dollars from 1996 to 2004, corresponding to 0.5% of total health related expenses [7]. For Europe, total burden of epilepsy was 0.2% of gross domestic product (GDP) of the whole Europe as 10 382 billion euro [8]. A study on prevalence and economic burden of epilepsy in Korea was performed using data from the Korean national health insurance by Lee et al. [9] in 2007 and reported that its prevalence was 2.41 per 1000 persons and its direct medical cost was 183 million dollars. Nevertheless as no study on cost of illness study including direct medical cost and indirect cost has been conducted, there is a need to estimate its economic burden at this time point when surgical treatment of epilepsy is going to be popularized.
- Estimating economic burden of illness is one of issues important for decision making in public health areas and the economic burden estimation will be utilized for assessing medical distribution, explaining health state of national people and establishing target of public health [10,11]. Therefore this study intended to identify prevalence of epilepsy by using national health insurance claimed data, estimate its socio-economic cost, and provide the latest data for its socio-economic burden of illness.
INTRODUCTION
- Study Population and Data Sources
- This study estimated economic burden of epilepsy via prevalence approach and used total claimed data of Health Insurance Review and Assessment Service (HIRA) to the Korea National Health Insurance (KNHI) in order to calculate its direct medical cost. Korea provides comprehensive National Health Insurance Service, both KNHI and HIRA, governmental agencies, monitor and supervises total use of medical service using medical health insurance, medical service provider must claim the medical service and drug prescription obligatorily to KNHI and HIRA. In addition, actual state survey data on user paid expenditure of the National Health Insurance Corporation 2010 in order to estimate user paid cost in the direct cost [12]. In order to estimate traffic expenses in the direct non-medical cost, this study used data from 2008 traffic cost survey of medical panel by diseases [13] and cited cost survey report of patient helper by the Korean Patient Helper Society in 2008 to estimate cost for medical care [14]. In addition, in order to estimate indirect cost, 2010 death statistics and 2010 basic statistics survey on wage structure of the Korean National Statistical Office were used [15,16].
- Selection Criteria
- This study was performed to patient defined as those who were hospitalized or visited an outpatient clinic during 2010 with a disease code of epilepsy, which included G40 (epilepsy) and G41 (status epilepticus of the diagnostic codes of the 10th version of the International Classification of Diseases and Related Health Problems (ICD-10) [17]. For the patients visiting outpatient clinic, those who visited medical institutions with same illness at least 3 times during 2010 were selected as patients to avoid over-estimation, while the patients having only 1 hospitalization record were considered as patients with epilepsy.
- Prevalence Estimation and Cost of Illness Studies
- This study measured prevalence subject to total beneficiaries of National Health Insurance in 2010, in which Medical Aid beneficiaries were also included. The treatment prevalence was calculated subject to those who satisfied the selection criteria in 2010 and prevalence by genders and ages were also assessed. This study estimated socio-economic cost of epilepsy to estimate economic burden of the illness, dividing it into direct cost and indirect cost [18]. The above direct cost was defined as cost required for treatment of epilepsy and divided into direct medical cost and direct no-medical cost. The indirect cost was defined as productivity loss from visiting outpatient clinic and in-hospitalization and productivity loss from early death.
- The direct medical cost comprises national health insurance benefit coverage treatment cost, lawful personal share, non-coverage medical expenditure including difference for upper grade bed use and selective medical expenditure, medicine purchasing cost by prescription for outpatients and inpatients. The national health insurance benefit coverage medical expenditure and the lawful personal share were calculated with cost claimed as major diseases such as ICD-10 G40 and G41. The non-coverage medical expenditure was calculated by estimating the mean non-coverage personal share of the epilepsy and its associated disease as 18.1% using data from 2010 actual survey of personal share medical expenditure [12]. For the pharmaceutical expenditure, basis to non-coverage pharmaceutical expenditure in the total pharmaceutical expenditure was insufficient. However the pharmaceutical expenditure of outpatient medical service was calculated using outpatient pharmaceutical expenditure of HIRA, considering that most drugs were involved in the health insurance coverage in Korea and presuming that there was no non-coverage pharmaceutical expenditure to avoid overestimation.
- The direct non-medical cost was composed of traffic expenditure used for visiting medical institutions for outpatient treatment and hospitalization and expenses for patient helper during in-hospitalization period. The traffic expenditure was calculated by substituting 4687.3 Korean won (KW) of mean one-way traffic expenditure of outpatient and 12 719.9 KW of mean one-way traffic expenditure of inpatient and then converting them to 2010 stand price index with standard traffic price index ratio, using 2008 data of medical panel's traffic expenditure of each outpatient and inpatient. Although expenditure of both caregiver and patient were considered, the patient aged within the range of 20 to 60 years old was regarded as visiting without caregiver [13]. The expenses for patient helper of hospitalized patients was calculated by multiplying the number of hospitalization days on the basis of 56 809 KW (2008) of mean expenses for patient helper per day provided by the Korean Patient Helper Society [14]. For outpatients aged below 20 and over 60, the expenditure was calculated by multiplying one third of the expenses for patient helper by the number of use of outpatient clinic.
- In the indirect cost, productivity loss from use of outpatient clinic, hospitalization, and early death was considered. However for the productivity loss from use of outpatient clinic and hospitalization, the patients aged below 20 and over 60 were not considered, regarded them as not participating in economic activities and the productivity loss from early death of population aged over 60 was not considered also. For inpatients, their productivity loss was calculated by multiplying the number of hospitalization days by average wage and for outpatients, one third of multiplication between the number of visits to outpatient clinic and the average wage was acknowledged as their productivity loss. The average wage was applied by 5 year of age groups, using 2010 basic statistics survey on wage structure and the productivity loss from early death was calculated by identifying the number of death from the relevant illness according to the annual report on the cause of death statistics and then converting possible income of each age group to current value with 3% of discount rate [15,16].
METHODS
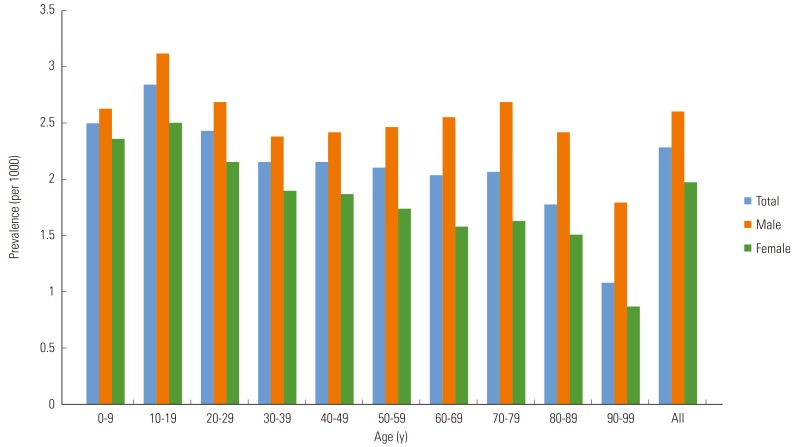
- During 2010, total 115 415 persons used outpatient clinic at least 3 times or were hospitalized at least 1 time due to epilepsy. Total treatment prevalence of epilepsy was 2.28 per 1000 persons, where the prevalence of male (2.60 per 1000 persons) was 1.65 time higher than that of female (1.97 per 1000 persons). By age groups, the age group of 10 to 19 showed the highest prevalence (2.84 per 1000 persons). Although there was a trend that the prevalence of females decreased with increase of age, the male showed a trend that their prevalence increased gradually between their 40's and 70's (Figure 1).
- It was found that the socio-economic burden of illness from epilepsy was 535 990 million KW in 2010. It was found also that the male had greater socio-economic burden of illness (347 400 million KW, 64.8%) than that of the female (188 580 million KW, 35.2%) and by age groups, the age group of 40 to 49 had the greatest socio-economic burden (108 850 million KW, 20.3%) (Table 1). It was shown that by items, the socio-economic burden of epilepsy included 196210 million KW (43.2%) of direct cost and 304 240 KW (56.8%), where the ratio between the direct and the indirect cost was 0.76:1 (Table 2). The direct medical cost accounted for 36.6% of total burden as 196 210 million KW; the ratio of direct medical cost of the female was higher (44.9%) than that of the male (32.1%); and the outpatient pharmaceutical expenditure took the greatest part as 37.4% of the direct medical cost. The direct non-medical cost was 6.6% of total disease burden as 35 550 million KW and the expenses for patient helper took the greatest part as 75.3%. Indirect cost had the highest ratio, 56.8% of total disease burden, as 304 240 million KW. In the indirect cost, the productivity loss from early death accounted for 78.5% of total indirect cost, as 238 900 million KW (Table 2).
RESULTS
- This study measured the prevalence of epilepsy and its economic burden, using the non-coverage rate data of KNHI and the annual report on the cause of death statistics of the National Statistical Office on the basis of 2010 data of HIRA. It was found that the prevalence of epilepsy measured in this study was 2.28 per 1000 persons, which was lower than that of the previous study by Lee et al. [9] (2.41 per 1000 persons) that measured the prevalence of epilepsy using data from KNHI and HIRA in 2007. In addition, as it was also lower than the prevalence measured in global record-based studies (2.7 to 17.6 per 1000 persons) and the prevalence estimated in Door to Door study (2.2 to 41.0 per 1000 persons), following things might be considered. This study used only G40 (epilepsy) and G41 (status epilepticus) code among ICD-10 codes for definition of epilepsy. In addition, this study defined those who visited outpatient clinic at least 3 times as the patient to elevate the accuracy of selection criteria. These have a possibility that the prevalence might be underestimated by excluding ICD-10, R56 (convulsion) code or those who visited outpatient clinic less than 3 times, considering that only single seizure could be judged as epilepsy clinically and medication could be initiated [19]. In this study, it was shown that the prevalence was the highest in the male, under 20 year old and similar to the results of traditional studies in United States and Europe [20-22]. And it was assumed that the higher prevalence of the age group under 20 year old was caused by the feature of epilepsy developing relatively early including hypoxic ischemic encephalopathy in perinatal period and central nervous system infection and trauma in neonatal or infant period [23-25]. Moreover the epilepsy showed a trend that the ratio of male increased, starting from 40 year old, which was assumed because brain injuries from cerebrovascular disease and trauma were major causes of epilepsy in the old man group. This prevalence pattern of epilepsy means that Korean outbreak of epilepsy is not so different from that of the developed countries.
- Total socio-economic burden was 536 billion KW, which corresponds to 0.05% of Korea GDP in 2020 and 0.64% of medical cost of national people in 2010. This was lower than that of the stroke having 4100 billion KW of socio-economic burden in 2010 [26] or the asthma estimated as 960 billion KW [27], but it was shown to have higher burden than the allergic rhinitis with economic burden of illness as 250 billion KW in 2007 [28]. The socio-economic burden from epilepsy was the highest in the age group of 40 to 49 for the male and in the age group of 20 to 29 for the female. The ratio between direct cost and indirect cost of epilepsy was 0.76:1, which was similar to the ratio of traditional foreign studies (57% to 85%) [29] as 56.8% of total socio-economic burden. It is considered that these are caused by the feature of epilepsy developing early in the age group below 20. In addition, the economic burden from epilepsy in the age group below 20 reached to 130 billion KW and accounted for 24.5% of total economic burden of epilepsy. Thus, there is a need for a research for perinatal newborn baby management for prevention of epilepsy in lower age group and additional research on surgical treatment of epilepsy, of which cost-effectiveness was proved via studies by King et al. in 1997 [30] and by Langfitt et al. in 2007 [31].
- In the study by Lee et al. [9] using data in 2007, it was found that the direct medical cost out of non-coverage items was 183 375 thousand US dollars. When comparing same items, it was shown that in spite of narrower definition of epilepsy, there was increase of direct medical cost for 3 years as much as 6.3% as 195 096 thousand US dollars.
- This study provides following information additionally, in comparison to the study by Lee et al. [9] using the data in 2007. While the previous presented prevalence of epilepsy and health insurance coverage in priority, this study calculated the socio-economic burden of epilepsy, dividing further into direct medical cost, direct non-medical cost, and indirect cost. In this study, the non-coverage treatment cost represented by difference for upper grade bed use and selective treatment cost, traffic expenditure and expenses for patient helper involved in the direct non-medical cost, and the indirect cost measuring the productivity loss were estimated for the epilepsy for the first time.
- This study has several limitations as follows. First, definition of disease is narrower than that of previous studies, where for the outpatient, those who visited medical institutes at least 3 times with same disease were defined as the patient. Because the cost was estimated based on the main disease, those who visited medical institute with minor disease might be excluded and the cost might be underestimated. Second, this study estimated the productivity loss via human capital approach, which might have a possibility of overestimation for the productivity loss in comparison with the friction-cost method. On the other hand, this study did not include broad range of participation rate in economic activities including housekeeping and child rearing by gender and age-group, and particularly did not considered productivity loss of the age groups below 20 and over 60. Besides, it did not acknowledged difference of wage level by using the average wage cited from the survey report on labor conditions by employment type. Therefore, there is a possibility for underestimation of the productivity loss. Third, although the epilepsy is one of chronic diseases requiring continuous management and treatment, so productivity loss from the residual disorders should be considered, this study considered only the productivity loss from use of medical service and early death. This should be complemented in a future study. Finally, the cost for treatment assistance from epilepsy and health promotion could not be estimated because of data limitations.
- In spite of these limitations, this study estimated the prevalence of epilepsy and its socio-economic cost by using nationwide data and calculated the direct non-medical coast and the indirect cost out of the direct medical cost for the first time. When a study for loss of epilepsy associated disorder is conducted In addition to this study, it will be used as basic data for cost-effectiveness analysis and decision-making associated with prevention and treatment of epilepsy.
DISCUSSION
ACKNOWLEDGEMENTS
- 1. Fisher RS, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005;46(4):470-472. 15816939ArticlePubMed
- 2. Sridharan R. Epidemiology of epilepsy. Curr Sci 2002;82(6):664-670
- 3. De Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav 2008;12(4):540-546. 18280210ArticlePubMed
- 4. Banerjee PN, Filippi D, Allen Hauser W. The descriptive epidemiology of epilepsy-a review. Epilepsy Res 2009;85(1):31-45. 19369037ArticlePubMedPMC
- 5. Sander JW. The epidemiology of epilepsy revisited. Curr Opin Neurol 2003;16(2):165-170. 12644744ArticlePubMed
- 6. Gaitatzis A, Trimble MR, Sander JW. The psychiatric comorbidity of epilepsy. Acta Neurol Scand 2004;110(4):207-220. 15355484ArticlePubMed
- 7. Yoon D, Frick KD, Carr DA, Austin JK. Economic impact of epilepsy in the United States. Epilepsia 2009;50(10):2186-2191. 19508694ArticlePubMed
- 8. Pugliatti M, Beghi E, Forsgren L, Ekman M, Sobocki P. Estimating the cost of epilepsy in Europe: a review with economic modeling. Epilepsia 2007;48(12):2224-2233. 18088267ArticlePubMed
- 9. Lee SY, Jung KY, Lee IK, Yi SD, Cho YW, Kim DW, et al. Prevalence of treated epilepsy in Korea based on national health insurance data. J Korean Med Sci 2012;27(3):285-290. 22379340ArticlePubMedPMC
- 10. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997;349(9063):1436-1442. 9164317ArticlePubMed
- 11. Stat NC. Healthy people 2000 review, 1995-1996. Hyattsville: Public Health Service; 1996. p. 1-3
- 12. Park JM, Tae YH. Results of survey on medical care cost by patient in Survey on the Benefit Coverage Rate of National Health Insurance in 2010. Seoul: National Health Insurance Corporation; 2011. p. 136-138
- 13. Korea Health Panel. The Korea Health Panel Survey. cited 2011 Aug 18. Available from: http://www.khp.re.kr/english/about_01.jsp
- 14. Korean Guardian Association. The official averaged guardian cost. Seoul: Korean Guardian Association; 2008. p. 3-5
- 15. Ministry of Employment and Labor. 2008 The survey report on labor conditions by employment type. cited 2012 Aug 18. Available from: http://laborstat.molab.go.kr/newWeb/intro/sub1/sub01_02.jsp
- 16. Korea National Statistical Office. Korean Statistical System 2010. cited 2012 Aug 18. Available from: http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&parentId=A
- 17. World Health Organization. ICD-10: international statistical classification of diseases and related health problems. cited 2012 May 5. Available from: http://apps.who.int/classifications/icd10/browse/2010/en
- 18. Jeong YH, Ko SJ. An estimation of economic costs of 5 major diseases. Health Welf Policy Forum 2003;79: 55-65
- 19. Engel J Jr. International League Against Epilepsy (ILAE). A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE Task Force on Classification and Terminology. Epilepsia 2001;42(6):796-803. 11422340ArticlePubMed
- 20. Hauser WA, Annegers JF, Kurland LT. Prevalence of epilepsy in Rochester, Minnesota: 1940-1980. Epilepsia 1991;32(4):429-445. 1868801ArticlePubMed
- 21. Forsgren L. Prevalence of epilepsy in adults in northern Sweden. Epilepsia 1992;33(3):450-458. 1592018ArticlePubMed
- 22. Forsgren L, Beghi E, Oun A, Sillanpää M. The epidemiology of epilepsy in Europe: a systematic review. Eur J Neurol 2005;12(4):245-253. 15804240ArticlePubMed
- 23. Trinka E, Höfler J, Zerbs A. Causes of status epilepticus. Epilepsia 2012;53(Suppl 4):127-138. 22946730ArticlePubMed
- 24. Vezzani A, Balosso S, Ravizza T. Inflammation and epilepsy. Handb Clin Neurol 2012;107: 163-175. 22938970ArticlePubMed
- 25. Besocke AG, Rosso B, Cristiano E, Valiensi SM, García Mdel C, Gonorazky SE, et al. Outcome of newly-diagnosed epilepsy in older patients. Epilepsy Behav 2013;27(1):29-35. 23369763ArticlePubMed
- 26. Kim HJ, Kim YA, Seo HY, Kim EJ, Yoon SJ, Oh IH. The economic burden of stroke in 2010 in Korea. J Korean Med Assoc 2012;55(12):1226-1236Article
- 27. Lee YH, Yoon SJ, Kim EJ, Kim YA, Seo HY, Oh IH. Economic burden of asthma in Korea. Allergy Asthma Proc 2011;32(6):35-40. 22221428ArticlePubMed
- 28. Kim SY, Yoon SJ, Jo MW, Kim EJ, Kim HJ, Oh IH. Economic burden of allergic rhinitis in Korea. Am J Rhinol Allergy 2010;24(5):e110-e113. 21244726ArticlePubMed
- 29. Strzelczyk A, Reese JP, Dodel R, Hamer HM. Cost of epilepsy: a systematic review. Pharmacoeconomics 2008;26(6):463-476. 18489198ArticlePubMed
- 30. King JT Jr, Sperling MR, Justice AC, O'Connor MJ. A cost-effectiveness analysis of anterior temporal lobectomy for intractable temporal lobe epilepsy. J Neurosurg 1997;87(1):20-28. 9202260ArticlePubMed
- 31. Langfitt JT, Holloway RG, McDermott MP, Messing S, Sarosky K, Berg AT, et al. Health care costs decline after successful epilepsy surgery. Neurology 2007;68(16):1290-1298. 17438219ArticlePubMed
REFERENCES
Table 1.Age and sex specific economic burden of epilepsy in Korea, 2010
Table 2.Cost of epilepsy in Korea, 2010
Figure & Data
References
Citations
Citations to this article as recorded by 

- Economic assessment of convulsive status epilepticus: Investigating socioeconomic correlations in hospitalization costs and outcomes in Northern India
Ahmad Ghayas Ansari, Ariba Nasar, Hiba Nasar
IP Indian Journal of Neurosciences.2024; 10(2): 78. CrossRef - Evaluation of persistence and healthcare utilization in patients treated with anti-seizure medications as add-on therapy: A nationwide cohort study in South Korea
Ji Woong Lee, Jung-Ae Kim, Min Young Kim, Sang Kun Lee
Epilepsy & Behavior.2022; 126: 108459. CrossRef - Cost of Illness of Epilepsy and Associated Factors in Patients Attending Adult Outpatient Department of University of Gondar Referral Hospital, Northwest Ethiopia
Piniel Melkamu, Yaregal Animut, Amare Minyihun, Asmamaw Atnafu, Mezgebu Yitayal
Risk Management and Healthcare Policy.2021; Volume 14: 2385. CrossRef - Cost–benefit analysis, cost-effectiveness analysis, and impact of antiepileptic drugs on the risk of fracture in patients with epilepsy: A nationwide cohort study
Hsin-Hsuan Cheng, Pei-Tseng Kung, Bo-Ren Wang, Li-Ting Chiu, Wen-Chen Tsai
Epilepsy & Behavior.2020; 103: 106851. CrossRef - Introducing big data analysis using data from National Health Insurance Service
EunJin Ahn
Korean Journal of Anesthesiology.2020; 73(3): 205. CrossRef - Epilepsy in Asia: Disease burden, management barriers, and challenges
Eugen Trinka, Patrick Kwan, ByungIn Lee, Amitabh Dash
Epilepsia.2019; 60(S1): 7. CrossRef - The Present and Future of Vagus Nerve Stimulation
Jeyul Yang, Ji Hoon Phi
Journal of Korean Neurosurgical Society.2019; 62(3): 344. CrossRef - Costs of informal nursing care for patients with neurologic disorders
Freya Diederich, Hans-Helmut König, Claudia Mietzner, Christian Brettschneider
Neurology.2018; 90(1): 28. CrossRef - The Economic Burden of Hepatitis A, B, and C in South Korea
Changwoo Shon, Hyung-Yun Choi, Jae-Jun Shim, So-Youn Park, Kyung Suk Lee, Seok-Jun Yoon, In-Hwan Oh
Japanese Journal of Infectious Diseases.2016; 69(1): 18. CrossRef - A nationwide epidemiological study of newly diagnosed spine metastasis in the adult Korean population
Seil Sohn, Jinhee Kim, Chun Kee Chung, Na Rae Lee, Eunjung Park, Ung-Kyu Chang, Moon Jun Sohn, Sung Hwan Kim
The Spine Journal.2016; 16(8): 937. CrossRef - The direct costs of epilepsy in Russia. A prospective cost-of-illness study from a single center in Moscow
Alla Guekht, Maria Mizinova, Igor Kaimovsky, Oksana Danilenko, Elisa Bianchi, Ettore Beghi
Epilepsy & Behavior.2016; 64: 122. CrossRef
 KSPM
KSPM



 PubReader
PubReader ePub Link
ePub Link Cite
Cite


