Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 46(6); 2013 > Article
-
Original Article
Cardiovascular Health Metrics and All-cause and Cardiovascular Disease Mortality Among Middle-aged Men in Korea: The Seoul Male Cohort Study - Ji Young Kim1, Young-Jin Ko1, Chul Woo Rhee1, Byung-Joo Park1,2, Dong-Hyun Kim3, Jong-Myon Bae4, Myung-Hee Shin5, Moo-Song Lee6, Zhong Min Li7, Yoon-Ok Ahn1,8
-
Journal of Preventive Medicine and Public Health 2013;46(6):319-328.
DOI: https://doi.org/10.3961/jpmph.2013.46.6.319
Published online: November 28, 2013
1Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea.
2Korea Institute of Drug Safety and Risk Management, Seoul, Korea.
3Department of Social Medicine, Hallym University College of Medicine, Chuncheon, Korea.
4Department of Preventive Medicine, Cheju National University College of Medicine, Jeju, Korea.
5Department of Social and Preventive Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea.
6Department of Preventive Medicine, Ulsan University College of Medicine, Seoul, Korea.
7Department of Epidemiology and Statistics, School of Public Health Sciences, Jilin University, Changchun, China.
8Korean Foundation for Cancer Research, Seoul, Korea.
- Corresponding author: Yoon-Ok Ahn, MD, PhD. 103 Daehak-ro, Jongno-gu, Seoul 110-799, Korea. Tel: +82-2-740-8322, Fax: +82-2-747-4830, yoahn@snu.ac.kr
Copyright © 2013 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- This study estimated the association of cardiovascular health behaviors with the risk of all-cause and cardiovascular disease (CVD) mortality in middle-aged men in Korea.
-
Methods
- In total, 12 538 men aged 40 to 59 years were enrolled in 1993 and followed up through 2011. Cardiovascular health metrics defined the following lifestyle behaviors proposed by the American Heart Association: smoking, physical activity, body mass index, diet habit score, total cholesterol, blood pressure, and fasting blood glucose. The cardiovascular health metrics score was calculated as a single categorical variable, by assigning 1 point to each ideal healthy behavior. A Cox proportional hazards regression model was used to estimate the hazard ratio of cardiovascular health behavior. Population attributable risks (PARs) were calculated from the significant cardiovascular health metrics.
-
Results
- There were 1054 total and 171 CVD deaths over 230 690 person-years of follow-up. The prevalence of meeting all 7 cardiovascular health metrics was 0.67%. Current smoking, elevated blood pressure, and high fasting blood glucose were significantly associated with all-cause and CVD mortality. The adjusted PARs for the 3 significant metrics combined were 35.2% (95% confidence interval [CI], 21.7 to 47.4) and 52.8% (95% CI, 22.0 to 74.0) for all-cause and CVD mortality, respectively. The adjusted hazard ratios of the groups with a 6-7 vs. 0-2 cardiovascular health metrics score were 0.42 (95% CI, 0.31 to 0.59) for all-cause mortality and 0.10 (95% CI, 0.03 to 0.29) for CVD mortality.
-
Conclusions
- Among cardiovascular health behaviors, not smoking, normal blood pressure, and recommended fasting blood glucose levels were associated with reduced risks of all-cause and CVD mortality. Meeting a greater number of cardiovascular health metrics was associated with a lower risk of all-cause and CVD mortality.
- The leading causes of death globally are non-communicable diseases (NCD) including cardiovascular disease (CVD), cancer, diabetes, and chronic respiratory disease, which accounted for 63% of 57 million deaths total worldwide in 2008. The largest proportion (48%) of NCD deaths globally is caused by CVD (International Classification of Disease, tenth revision [ICD-10] codes I01-I99) [1]. In Korea, circulatory system diseases are the second most common cause of death, accounting for an even greater proportion of the mortality rate in each of the last 2 years. Cardio-cerebrovascular diseases were the leading causes of circulatory system disease deaths in 2011 [2].
- Behavioral risk factors including current smoking, physical inactivity, unhealthy diet, and excessive alcohol consumption are responsible for about 80% of cases of coronary heart disease and cerebrovascular disease [3]. These CVD risk factors are related to 4 major physio-metabolic changes: elevated blood pressure, increased weight, hyperglycemia, and dyslipidemia [1]. Meanwhile, individuals with a greater number of cardiovascular health habits have a significantly lower CVD mortality rate than those with fewer such health habits [4-6].
- In 2010, the American Heart Association (AHA) published recommendations aimed at reducing deaths from all CVDs and stroke, and at improving the cardiovascular health of the population as a whole. To measure progress toward these prevention-related goals, the AHA defined the construct of "ideal cardiovascular health" on the basis of 7 metrics: smoking habit, body mass index (BMI), nutritional intake, physical activity level, blood pressure, blood glucose level, and total cholesterol level [7].
- In Korea in 2009, the Korea Centers for Disease Control Prevention proposed "Nine healthy life habits for prevention and management of cardio-cerebrovascular diseases" [8]. However, these recommendations have insufficiently detailed goals for and quantitative measures of a healthy lifestyle to evaluate the effectiveness of preventive measures at the individual and population levels. In 2012, using data from US-National Health and Nutritional Examination Surveys (NHANES) linked to mortality, Yang et al. [9] categorized the population by awarding up to 7 cardiovascular health scores on the basis of healthy behaviors; thus, ≥6 points reflects the increasingly well recognized low-risk group. The emphasis on maintaining healthy habits rather than recognizing and treating high-risk individuals offers a highly desirable message for health promotion for the general population. Despite their implications, the AHA's metrics have not been broadly studied or previously applied to an Asian population. Therefore, in this study, we assessed the 7 cardiovascular health metrics among middle-aged men in Korea and estimated the combined association and population-attributable risk (PAR) of these cardiovascular health behaviors with respect to the risks of all-cause and CVD mortality.
INTRODUCTION
- Study Population
- The study cohort was taken from the Seoul Male Cohort Study, which was initiated in January 1993. Detailed descriptions of the design of the Seoul Male Cohort Study have been reported previously [10-13]. A total 14 533 cohort participants, male sex, 40 to 59 years of age, and residing in or near Seoul, South Korea, completed comprehensive baseline surveys and conducted health examinations of the Korea Medical Insurance Corporation in 1992 [13]. Survey questionnaires were only measured once at the cohort construction. Of the 14 533 subjects, we excluded subjects who self-reported having a medical history of cerebrovascular disease (n=86) or myocardial infarction (n=243), or a BMI <18.5 at baseline (n=191) [9]. Regarding the health behavior, we also excluded participants missing data on 1 or more of the cardiovascular health metrics (n=1475). In the end, 12 538 subjects were included among the study participants. This study was approved by the institutional review board of Seoul National University College of Medicine/Seoul National University Hospital (C-1301-015-454).
- Mortality Assessment
- Participants were followed from January 1, 1993 to December 31, 2011. Information on the date and causes of death was obtained from mortality microdata by the National Statistics Office. Causes of death are indicated by ICD-10 codes. Mortality from total CVD was defined by the ICD-10 codes, I01-I99 [1,14].
- Definitions of Cardiovascular Health Metrics
- To define cardiovascular health metrics, the following 7 cardiovascular health behaviors proposed by the AHA were applied and modified for our analysis [7]: smoking, physical activity, BMI, healthy diet score, total cholesterol, blood pressure, and fasting blood glucose. All 7 cardiovascular health behaviors were measured once at the time of the baseline surveys in cohort recruitment.
- Smoking
- We used the categories of never, former and current smoker [7]. Time since smoking cessation was assessed at baseline in 1992.
- Physical activity
- To assess physical activity, the following question was asked during the baseline survey: "In the past year, how many hours a week have you spent on vigorous and moderate exercise?" We classified the subjects as ideal level if they engaged in any physical activity for ≥150 min/wk at moderate intensity, ≥75 min/wk at vigorous intensity, or ≥150 min/wk at moderate or vigorous intensity [7,9].
- Body mass index
- BMI (kg/m2) was calculated as weight (kg) divided by the squared height (m2). For the BMI, intermediate and poor health were defined by overweight (25> BMI ≥23) and obesity (BMI ≥25), respectively [15].
- Healthy diet score
- We modified healthy diet components on the basis of Korean dietary pattern. The healthy diet score (range, 0 to 5) was calculated by summing the following dietary items, assigning 1 point each for the consumption of fruits or vegetables (≥450 g/d), fish (≥2 times/wk), brown rice (≥1 serving/d), sodium (≤ 2000 mg/d), and sugar-sweetened beverages (sugar-sweetened coffee ≤1 time/d and soft drink ≤1 L/wk). The healthy diet score was estimated on the basis of the semi-quantitative food frequency questionnaire (FFQ) and the Korean Nutrient Database compiled by the Korean Nutrition Society to estimate the daily sodium intake [16]. The development and validation of the FFQ are described elsewhere [17]. For analyses, we dichotomized the scores as <2 or ≥2 components [9] because of the small number of participants with scores ≥3 (n=32).
- Total cholesterol, blood pressure, and fasting blood glucose
- The ideal levels of total cholesterol, blood pressure, and fasting blood glucose were defined according to current clinical practice guidelines. We classified the total cholesterol level into 3 categories: <200, 200-239, and ≥240 mg/dL [18]. Ideal blood pressure was <120/80 mmHg, and ideal fasting blood glucose was <100 mg/dL, which are consistent with their respective optimal threshold levels [19,20].
- Cardiovascular health metrics score
- We calculated a cardiovascular health metrics score by recoding the 7 metrics as dichotomous variables, awarding 1 point for ideal vs. 0 points otherwise with the exception of the healthy diet score: (healthy diet components ≥2 [1 point] vs. <2 [0 points]) [9]. All of the subjects were classified as meeting 0-7 cardiovascular health metrics. The sum of these scores indicates how many individual measures a participant had at the ideal level.
- Other Lifestyle Factors
- Other demographic and lifestyle factors included in our analyses were age, education attainment, alcohol consumption, sleep hours, and family history of CVD (yes/no). The subjects were divided into 5-year cohorts at entry: 40 to 44, 45 to 49, 50 to 54, and 55 to 59 years. Educational attainment was classified as high school or lower, and some college or higher. Alcohol consumption was assessed at the baseline survey: "Have you ever drunk alcohol?" Alcohol drinking was classified as current, former, and never. For sleep hours, participants were asked to report their mean daily sleep hours in the past year; responses were classified into 3 categories: ≤5, 6-7, and ≥8 hours. There were also questions about past medical history, including whether the subjects had CVD or myocardial infarction.
- Statistical Analyses
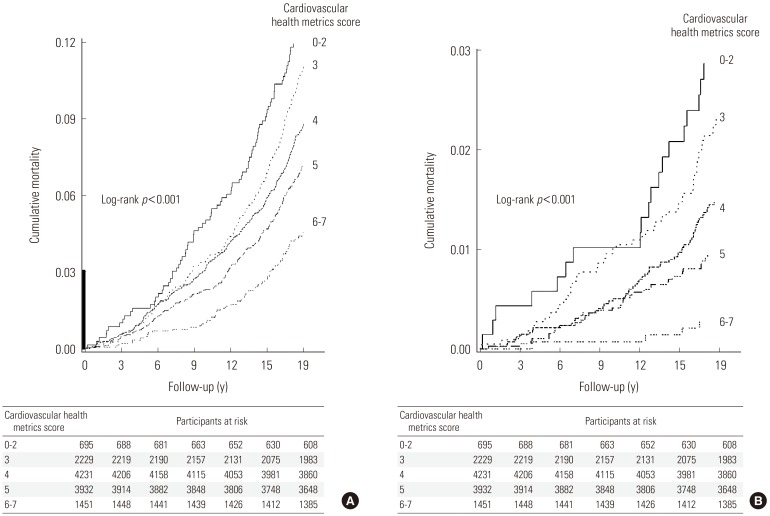
- To evaluate associations and compare differences between 2 groups, we used the χ2 test or t-test. We used Cox proportional hazards regression models to estimate the hazard ratios (HRs) for all-cause and CVD mortality associated with cardiovascular health metrics. Multivariable HRs were adjusted for age, educational attainment, alcohol drinking, sleep hours, family history of CVD, and other cardiovascular health metrics. Variables with p<0.1 in the univariate analysis were selected as potential confounders. We calculated adjusted PARs using available macro estimates of the proportions of all-cause and CVD mortality in this cohort that would have hypothetically been avoided [21-23]. To calculate the HRs with the cardiovascular health metrics score, we used participants with a score of 0-2 as the reference because of few of the participants who had a score of 0 (n=6) or 1 (n=77); we also combined participants with a score of 6 or 7 (n=84) into a single group for robust estimation. The person-years of follow-up were measured from the time of entry into the study until the date of death or December 31, 2011. Age-adjusted all-cause and CVD mortality rates (per 1000 person-years) were calculated using the direct method of standardization with age distribution of the whole cohort as the standard. A p-value for trends was calculated using a Satterthwaite adjusted F-test. Kaplan-Meier survival curves were drawn for cumulative all-cause and CVD mortality according to the cardiovascular health metrics scores. All of the tests were 2-tailed, and the level of significance was set at p<0.05. Analyses were conducted using SAS version 9.3 (SAS Inc., Cary, NC, USA).
METHODS
- The general characteristics of the subjects and the 7 cardiovascular health metrics are shown in Table 1. Smoking, physical activity, blood pressure, and fasting blood glucose were significantly different between the living and deceased cohorts. There were 1054 deaths in total, 564 (53.5%) due to cancer (C00-C97), and 171 (16.2%) due to CVD during 230 690 person-years of follow-up. Non-smoking, normal blood pressure, and fasting blood glucose <100 mg/dL were independently associated with significantly lower risks of all-cause and CVD mortality (Table 2). Adjusted PARs for all-cause mortality ranged from 1.2% (95% confidence interval [CI], 0% to 2.9%) for fasting blood glucose (≥100 mg/dL) to 29.2% (95% CI, 22.2% to 35.9%) for current smoking. The adjusted PARs for the 3 significant metrics combined were 35.2% (95% CI, 21.7% to 47.4%) and 52.8% (95% CI, 22.0% to 74.0%) for all-cause and CVD mortality, respectively (Table 3). Among participants who had ≤2 cardiovascular health metrics, the age-standardized absolute risks were 6.83 deaths per 1000 person-years for all-cause mortality and 1.62 for CVD mortality; among participants who had ≥6 cardiovascular health metrics, the corresponding risks were 2.52 deaths per 1000 person-years for all-cause mortality and 0.16 for CVD mortality (p<0.001 for trend). The adjusted HRs for the cardiovascular health metrics scores of the participants with the highest scores compared to those with the lowest scores were 0.42 (95% CI, 0.31 to 0.59) and 0.10 (95% CI, 0.03 to 0.29) for all-cause and CVD mortality, respectively (Table 4). Figure 1 shows the Kaplan-Meier curves for cumulative all-cause and CVD mortality among participants with cardiovascular health metrics scores of 0-2, 3, 4, 5, and ≥6. A greater number of cardiovascular health metrics was associated with lower risks of all-cause and CVD mortality (p<0.001 for trend). Regarding the risk of cancer death, participants without current smoking status had a significantly lower risk of all-cancer mortality (adjusted HR, 0.60; 95% CI, 0.50 to 0.72). However, a greater number of cardiovascular health metrics was not associated with lower risk of all-cancer mortality (data not shown).
RESULTS
- In this prospective cohort study, we evaluated the associations of individual and combined cardiovascular health metrics based on the definitions of the AHA with all-cause and total CVD mortality in healthy middle-aged men in Korea participating in the Seoul Male Cohort Study. Three of the 7 cardiovascular health behaviors-non-smoking status, normal blood pressure, and ideal fasting blood glucose-were significantly associated with reduced risks of all-cause and total CVD mortality compared to the presence of none of these factors. Furthermore, having a greater number of cardiovascular health metrics reduced the risk of all-cause and CVD mortality.
- Our findings are concordant with those of previous studies on the association between combined low-risk lifestyle factors and all-cause or CVD mortality [9,14,24-26]. In their recent analyses of 13 312 American adults aged ≥20 years using data from the US-NHANES, Yang et al. [9] report that among the 7 cardiovascular health metrics recommended by the AHA, not smoking, ideal and intermediate physical activity, normal blood pressure, and HbA1c <5.7% were independently associated with significant reductions of all-cause and CVD mortality. Yang et al. [9] also reported the adjusted HRs of all-cause and CVD mortality comparing participants who met ≥6 vs. ≤1 cardiovascular health metrics as 0.49 (95% CI, 0.33 to 0.74) and 0.24 (95% CI, 0.13 to 0.47), respectively. These results are very similar to the magnitudes of association in the present study. However, comparing the participants of both studies, a significantly higher proportion of participants met ≥6 cardiovascular health metrics in the present study than in the previous study (n=1451/12 538 [11.6%] vs. n=957/13 312 [7.2%]). In contrast, the proportion of participants who met 0-1 metric was lower in the present study (n=83/12 538 [0.66%] vs. n=1236/13 312 [9.3%]). Furthermore, the proportion of subjects with ideal cardiovascular health was higher in the present population than in the US-NHANES population [9]. This difference could be accounted for by differences in gender, mean age, and racial diversity. In addition, participants of the present study were government employees, school teachers, and pensioners at the time of the recruitment. Although the subjects of this study were part of general population in Korea, they might have had more healthy behaviors or higher socioeconomic status than the US-NHANES population. Nevertheless, the simple cardiovascular health metrics score was closely related to all-cause and total CVD mortality in both studies.
- The EPIC-Norfolk study reported that the combination of four healthy behaviors (i.e., non-smoking, being physically active, having moderate alcohol intake, and plasma vitamin C >50 mmol/L) is associated with lower risks of all-cause and CVD mortality [24]. Yun et al. [25] report that among 59 941 Koreans who visited a health promotion center, having a high unhealthy lifestyle score increased the risk of all-cause mortality. Further, current smoking and physical inactivity were independently associated with an increased risk of mortality. In the Japan Collaborative Cohort study, Eguchi et al. [14] report that the HRs of total CVD mortality for 7-8 vs. 0-2 points for combined healthy lifestyle behaviors on a scale of 0 to 8 were 0.36 (95% CI, 0.22 to 0.58) for men. In the Singapore Chinese Health Study, CVD mortality rates decreased sharply with an increasing number of protective lifestyle behaviors (i.e., dietary habit pattern, physical activity, alcohol intake, usual sleep time, smoking status, and BMI) [26].
- Not all of the individual metrics contributed to the reduction in risk. Physical activity, BMI, healthy diet, and total cholesterol were not significantly associated to all-cause or CVD mortality in the present study. However, some studies have provided evidence supporting the benefits of a healthy diet and physical activity for all-cause mortality or CVD incidence [27-29]. For the healthy dietary habits, few participants (n=547/12 538 [4.4%]) had the intermediate level of healthy diet (≥2 components) and only 1 participant had the ideal healthy diet (≥4 components). A significantly larger proportion of US-NHANES participants (n=3067/13 312 [23.0%]) achieved the intermediate dietary health level than our study participants [9]. However, the AHA's healthy diet recommendation based on the Dietary Approaches to Stop Hypertension-type eating plan was different from the Korean food items and diet pattern. The use of a simple index of minimum daily intake of fruits and milk or maximum daily intake of sodium could be easy to apply [14]. To develop a more valid and suitable healthy diet score related to CVD, further studies are required among Koreans. Regarding the BMI, a recent meta-analysis indicates that the BMI does not improve risk prediction for first-onset CVD when additional information exists on blood pressure, diabetes mellitus history, and cholesterol measures [30]. Jee et al. [31] reported that smoking was an independent risk factor for CVD and that a low cholesterol level had no protective benefit against smoking-related atherosclerotic CVD. Eguchi et al. [14] found that the protective effect of each health behavior in men is generally larger among non-smokers than in smokers. The prevalence of current smokers among our participants (51.3%) is nearly twice that reported in the US-NHANES population (26.6%) [9]. Lack of a protective benefit of some healthy behaviors could potentially be explained by remarkably higher proportions of current smokers in the present study.
- In the present study, smoking was associated with the largest PARs for all-cause and CVD mortality. Even though the prevalence of smoking among Koreans has declined over the last 15 years, nearly half (47.3%) of Korean men aged ≥19 years were still current cigarette smokers in 2011 [32]. Focusing on promoting smoking cessations would further reduce CVD death. Based on our analysis, if all cohort members quit smoking, and decreased their blood pressure and fasting blood glucose, an estimated 52.8% of CVD s death would be avoided.
- It should be noted that when estimating the combined effect of the 7 cardiovascular health metrics on mortality risk, we categorized participants on the basis of their number of healthy lifestyle factors independent of statistical significance. Lifestyle behaviors may act synergistically to increase or reduce the risk of disease or death. However, existing biological or epidemiological evidence is not enough to measure these synergistic mechanisms into reliable estimates [33]. Health behaviors comprise multiple dimensions and causal processes. Thus, using a combined lifestyle analysis may elucidate the relationships between individual health behaviors [34].
- The present study has certain limitations. First, the baseline measurements of the survey questionnaire including cardiovascular health metrics were only performed once at the time of cohort recruitment. We were unable to quantify the effects of changes in these lifestyle habits on all-cause and CVD mortality during follow-up. This could lead to non-differential misclassifications, resulting in the underestimation of associations. Second, our study evaluated the associations between cardiovascular health metrics and CVD mortality, and not incidence. CVDs or other diseases may induce lifestyle changes and consequently mortality risks. To minimize this effect, we excluded subjects with a history of myocardial infarction or CVDs. Third, when calculating the cardiovascular health metrics score, we excluded 1705 subjects who had missing information on ≥1 metric. This is likely to result in a selection bias. However, there was no significant difference in risk factors between individuals with complete and incomplete health metrics scores. Fourth, the baseline FFQ was not consistent with the AHA's healthy diet definition. There is insufficient information about the standard ideal healthy diet associated with CVD mortality in the Korean population. Fifth, individual cardiovascular health metrics risks were dichotomized, which could limit the interpretation of the effects of different healthy behaviors. However, applying equivalent weights to these health factors may have resulted in conservative estimates. The use of the simple score algorithm facilitated study interpretation and provided clear information about the general population.
- Despite these limitations, our study has several advantages. First, this was a prospective cohort study of mortality with a long follow-up (19 years). Second, the results of a baseline questionnaire survey administered to disease-free participants at health examinations were analyzed, allowing the determination of clear causal relationships. Third, our study surveyed a number of detailed health behavior variables and potential confounders for CVD at baseline recruitment, including family history of CVD. Fourth, we estimated adjusted PARs for individual and combined cardiovascular health metrics significantly reducing the risks of all-cause and CVD mortality. These findings suggest that health gains are achievable when adults move from poor to intermediate and intermediate to ideal health with respect to most health metrics at the population level.
- In conclusion, in this prospective cohort study, 3 individual cardiovascular health behaviors-non-smoking status, normal blood pressure, and recommended fasting blood glucose level-were significantly associated with reduced risks of all-cause and total CVD mortality. Meeting a greater number of cardiovascular health metrics was reduced the risk of all-cause and CVD mortality, but the prevalence of having all 7 cardiovascular health behaviors was low in the study population. Comprehensive primordial and primary prevention strategies promoting healthy lifestyles by increasing the prevalence of desirable healthy behaviors will improve the cardiovascular health status of the general population.
DISCUSSION
ACKNOWLEDGEMENTS
- 1. World Health Organization. World health statistics 2012. cited 2013 June 24. Available from: http://www.who.int/gho/publications/world_health_statistics/EN_WHS2012_Full.pdf
- 2. Korea National Statistical Office. 2011 Annual report on the cause of death statistics. Seoul: Korea National Statistical Office; 2012. p. 6-7 (Korean)
- 3. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. p. 28
- 4. Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation 2012;125(8):987-995. 22291126ArticlePubMedPMC
- 5. Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med 2012;366(4):321-329. 22276822ArticlePubMedPMC
- 6. Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol 2011;57(16):1690-1696. 21492767ArticlePubMedPMC
- 7. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation 2010;121(4):586-613. 20089546ArticlePubMed
- 8. Korea Centers for Disease Control and Prevention. Nine healthy life habits for prevention and management of cardio-cerebrovascular diseases. 2009. cited 2013 Jun 24. Available from: http://www.cdc.go.kr/CDC/notice/CdcKrIntro0504.jsp?menuIds=HOME001-MNU0004-MNU0015-MNU0110&cid=11063
- 9. Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012;307(12):1273-1283. 22427615ArticlePubMedPMC
- 10. Shin MH, Kim DH, Bae JM, Lee HK, Lee MS, Noh JY, et al. The effect of coffee consumption on serum total cholesterol level in healthy middle-aged men. Korean J Prev Med 1994;27(2):200-216. (Korean)
- 11. Lee MS, Kang WC, Kim DH, Bae JM, Shin MH, Lee YJ, et al. Methodologic considerations on the cohort study of risk factors of stomach cancer: on the incompleteness of case ascertainment. Korean J Epidemiol 1997;19(2):152-160. (Korean)
- 12. Bae JM, Ahn YO. A nested case-control study on the high-normal blood pressure as a risk factor of hypertension in Korean middle-aged men. J Korean Med Sci 2002;17(3):328-336. 12068135ArticlePubMedPMC
- 13. Rhee CW, Kim JY, Park BJ, Li ZM, Ahn YO. Impact of individual and combined health behaviors on all causes of premature mortality among middle aged men in Korea: the Seoul Male Cohort Study. J Prev Med Public Health 2012;45(1):14-20. 22389754ArticlePubMedPMCPDF
- 14. Eguchi E, Iso H, Tanabe N, Wada Y, Yatsuya H, Kikuchi S, et al. Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women: the Japan collaborative cohort study. Eur Heart J 2012;33(4):467-477. 22334626ArticlePubMed
- 15. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363(9403):157-163. 14726171ArticlePubMed
- 16. Ahn Y, Paik HY, Ahn YO. Item non-responses in mailed food frequency questionnaires in a Korean male cancer cohort study. Asia Pac J Clin Nutr 2006;15(2):170-177. 16672200PubMed
- 17. Kim MK, Lee SS, Ahn YO. Reproducibility and validity of a self-administered semiquantitative food frequency questionnaire among middle-aged men in Seoul. Korean J Community Nutr 1996;1(3):376-394. (Korean)
- 18. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106(25):3143-3421. 12485966ArticlePubMed
- 19. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289(19):2560-2572. 12748199ArticlePubMed
- 20. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2007;30(Suppl 1):S42-S47. 17192378ArticlePubMedPDF
- 21. Spiegelman D, Hertzmark E, Wand HC. Point and interval estimates of partial population attributable risks in cohort studies: examples and software. Cancer Causes Control 2007;18(5):571-579. 17387622ArticlePubMed
- 22. Hertzmark E, Wand H, Spiegelman D. The SAS PAR macro. 2012. cited 2013 June 20. Available from: http://www.hsph.harvard.edu/donna-spiegelman/files/2012/09/par_documentation-_march_2012.pdf
- 23. Bruzzi P, Green SB, Byar DP, Brinton LA, Schairer C. Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epidemiol 1985;122(5):904-914. 4050778ArticlePubMed
- 24. Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med 2008;5(1):e12. 18184033ArticlePubMedPMC
- 25. Yun JE, Won S, Kimm H, Jee SH. Effects of a combined lifestyle score on 10-year mortality in Korean men and women: a prospective cohort study. BMC Public Health 2012;12: 673. 22900981ArticlePubMedPMC
- 26. Odegaard AO, Koh WP, Gross MD, Yuan JM, Pereira MA. Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women: the Singapore Chinese health study. Circulation 2011;124(25):2847-2854. 22104554ArticlePubMedPMC
- 27. Tamakoshi A, Tamakoshi K, Lin Y, Yagyu K, Kikuchi S. JACC Study Group. Healthy lifestyle and preventable death: findings from the Japan Collaborative Cohort (JACC) Study. Prev Med 2009;48(5):486-492. 19254743ArticlePubMed
- 28. Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 2010;122(4):406-441. 20625115ArticlePubMedPMC
- 29. Behrens G, Fischer B, Kohler S, Park Y, Hollenbeck AR, Leitzmann MF. Healthy lifestyle behaviors and decreased risk of mortality in a large prospective study of U.S. women and men. Eur J Epidemiol 2013;28(5):361-372. 23532745ArticlePubMed
- 30. Emerging Risk Factors Collaboration. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet 2011;377(9771):1085-1095. 21397319ArticlePubMedPMC
- 31. Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. JAMA 1999;282(22):2149-2155. 10591337ArticlePubMed
- 32. Korea Centers for Disease Control and Prevention. Korea health statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Cheongwon: Korea Centers for Disease Control and Prevention; 2012. p. 22-23 (Korean)
- 33. Kim S, Popkin BM, Siega-Riz AM, Haines PS, Arab L. A cross-national comparison of lifestyle between China and the United States, using a comprehensive cross-national measurement tool of the healthfulness of lifestyles: the Lifestyle Index. Prev Med 2004;38(2):160-171. 14715207ArticlePubMed
- 34. Jiao L, Mitrou PN, Reedy J, Graubard BI, Hollenbeck AR, Schatzkin A, et al. A combined healthy lifestyle score and risk of pancreatic cancer in a large cohort study. Arch Intern Med 2009;169(8):764-770. 19398688ArticlePubMedPMC
REFERENCES
| Variables | All-cause death (n = 1054) | Live cohort (n = 11 484) | p-value | |
|---|---|---|---|---|
| Age (y) | Mean±SD | 50.0±5.2 | 47.3±5.0 | <0.001 |
| 40-44 | 203 (19.3) | 4247 (37.0) | <0.001 | |
| 45-49 | 258 (24.5) | 3383 (29.5) | ||
| 50-54 | 349 (33.1) | 2675 (23.3) | ||
| 55-59 | 244 (23.1) | 1179 (10.3) | ||
| Education attainment | ≥College1 | 579 (54.9) | 6158 (53.6) | <0.001 |
| ≤High school | 475 (45.1) | 5325 (46.4) | ||
| Missing | 0 (0.0) | 1 (0.01) | ||
| Family history of CVD | No | 856 (81.2) | 9245 (80.5) | 0.42 |
| Yes | 166 (15.8) | 1945 (16.9) | ||
| Missing | 32 (3.0) | 294 (2.6) | 0.01 | |
| Alcohol drinking | Never | 212 (20.1) | 2785 (24.3) | |
| Former | 101 (9.6) | 930 (8.1) | ||
| Current | 717 (68.0) | 7466 (65.0) | ||
| Missing | 24 (2.3) | 303 (2.6) | 0.002 | |
| Sleep hours | 8 Hours or more | 270 (25.6) | 2985 (26.0) | |
| 6-7 Hours | 722 (68.5) | 8093 (70.5) | ||
| 5 Hours or less | 57 (5.4) | 370 (3.2) | ||
| Missing | 5 (0.5) | 36 (0.3) | ||
| Cardiovascular health metrics | ||||
| Smoking | Never | 162 (15.4) | 2757 (24.0) | <0.001 |
| Former (quit >12 mo) | 176 (16.7) | 2463 (21.4) | ||
| Former (quit ≤12 mo) | 37 (3.5) | 515 (4.5) | ||
| Current | 679 (64.4) | 5749 (50.1) | ||
| Physical activity2 | Ideal | 410 (38.9) | 4740 (41.3) | 0.002 |
| Intermediate | 394 (37.4) | 4542 (39.5) | ||
| None | 250 (23.7) | 2202 (19.2) | ||
| BMI (kg/m2) | ≥18.5 and <23 | 469 (44.5) | 4944 (43.0) | 0.62 |
| ≥23 and <25 | 336 (31.9) | 3811 (33.2) | ||
| ≥25 | 249 (23.6) | 2729 (23.8) | ||
| Healthy diet score components3 | ≥2 | 38 (3.6) | 509 (4.4) | 0.21 |
| <2 | 1016 (96.4) | 10 975 (95.6) | ||
| Total cholesterol (mg/dL) | <200 | 554 (52.6) | 5991 (52.2) | 0.41 |
| 200-239 | 350 (33.2) | 3996 (34.8) | ||
| ≥240 | 150 (14.2) | 1497 (13.0) | ||
| Blood pressure (mmHg) | <120/80 | 607 (57.6) | 7481 (65.1) | <0.001 |
| 120-139/80-89 | 222 (21.1) | 2296 (20.0) | ||
| ≥140/≥90 | 225 (21.3) | 1707 (14.9) | ||
| Fasting blood glucose (mg/dL) | <100 | 1011 (95.9) | 11 216 (97.7) | 0.002 |
| 100-125 | 15 (1.4) | 102 (0.9) | ||
| ≥126 | 28 (2.7) | 166 (1.4) | ||
| No. of cardiovascular health metrics | 0 | 1 (0.1) | 5 (0.04) | <0.001 |
| 1 | 8 (0.8) | 69 (0.6) | ||
| 2 | 78 (7.4) | 534 (4.6) | ||
| 3 | 246 (23.3) | 1983 (17.3) | ||
| 4 | 371 (35.2) | 3860 (33.6) | ||
| 5 | 284 (26.9) | 3648 (31.8) | ||
| 6 | 60 (5.7) | 1307 (11.4) | ||
| 7 | 6 (0.6) | 78 (0.7) |
Values are presented as number (%).
CVD, cardiovascular disease; BMI, body mass index; SD, standard deviation.
1 University dropouts included.
2 Ideal physical activity (moderate intensity ≥150 min/wk, or at vigorous intensity ≥75 min/wk, or moderate + vigorous intensity ≥150 min/wk; intermediate physical activity (1.149 min/wk at moderate intensity, or 1-74 min/wk at vigorous intensity, or 1-149 min/wk at moderate + vigorous intensity).
3 Healthy diet components: fruits and vegetables (≥450 g/d), fish (≥2 times/wk), sodium (<2000 mg/d), brown rice (≥1 time/d), sugar-sweetened beverages (sugar-sweetened coffee ≤1 time/d and soft drink ≤1 L/wk).
| Cardiovascular health metrics | Participant (n = 12 538) |
All-cause mortality |
CVD mortality |
||||
|---|---|---|---|---|---|---|---|
| All deaths (n = 1054) | Crude HR (95% CI) | Adjusted HR1 (95% CI) | CVD deaths (n = 171) | Crude HR (95% CI) | Adjusted HR1 (95% CI) | ||
| Current smoking*** | |||||||
| Yes | 6428 (51.3) | 679 | 1.00 | 1.00 | 114 | 1.00 | 1.00 |
| No | 6110 (48.7) | 375 | 0.57 (0.50, 0.64) | 0.57 (0.50, 0.66) | 57 | 0.52 (0.38, 0.70) | 0.45 (0.32, 0.63) |
| Physical activity | |||||||
| No | 2452 (19.6) | 250 | 1.00 | 1.00 | 42 | 1.00 | 1.00 |
| Yes | 10 086 (80.4) | 804 | 0.77 (0.67, 0.89) | 0.89 (0.77, 1.03) | 129 | 0.74 (0.52, 1.04) | 0.87 (0.60, 1.26) |
| BMI (kg/m2) | |||||||
| ≥23 | 7125 (56.8) | 585 | 1.00 | 1.00 | 103 | 1.00 | 1.00 |
| ≥18.5 and <23 | 5413 (43.2) | 469 | 1.06 (0.94, 1.19) | 1.06 (0.93, 1.20) | 68 | 0.87 (0.64, 1.18) | 0.91 (0.66, 1.26) |
| Healthy diet score components | |||||||
| <2 | 11 991 (95.6) | 1016 | 1.00 | 1.00 | 167 | 1.00 | 1.00 |
| ≥2 | 547 (4.4) | 38 | 0.82 (0.59, 1.13) | 0.81 (0.57, 1.14) | 4 | 0.52 (0.19, 1.41) | 0.44 (0.14, 1.39) |
| Total cholesterol (mg/dL) | |||||||
| ≥200 | 1647 (13.1) | 150 | 1.00 | 1.00 | 29 | 1.00 | 1.00 |
| <200 | 10 891 (86.9) | 904 | 0.91 (0.76, 1.08) | 0.95 (0.79, 1.13) | 142 | 0.74 (0.49, 1.10) | 0.82 (0.54, 1.24) |
| Blood pressure (mmHg)*** | |||||||
| ≥120/≥80 | 4450 (35.5) | 447 | 1.00 | 1.00 | 97 | 1.00 | 1.00 |
| <120/<80 | 8088 (64.5) | 607 | 0.74 (0.65, 0.83) | 0.83 (0.73, 0.94) | 74 | 0.41 (0.31, 0.56) | 0.45 (0.33, 0.62) |
| Fasting blood glucose (mg/dL)*** | |||||||
| ≥100 | 311 (2.5) | 43 | 1.00 | 1.00 | 11 | 1.00 | 1.00 |
| <100 | 12 227 (97.5) | 1011 | 0.58 (0.42, 0.78) | 0.66 (0.48, 0.91) | 160 | 0.36 (0.19, 0.66) | 0.49 (0.26, 0.92) |
| Cardiovascular health metrics | Participants n=12 538 |
All-cause mortality |
|||
|---|---|---|---|---|---|
| All deaths n = 1054 | Adjusted PAR1 (95% CI) | CVD deaths n = 171 | Adjusted PAR1 (95% CI) | ||
| One cardiovascular health metric | |||||
| Current smoking (yes) | 6428 | 679 | 29.2 (22.2, 35.9) | 114 | 30.9 (13.7, 46.2) |
| Blood pressure (≥120/≥80 mmHg) | 4450 | 447 | 7.3 (1.0, 13.5) | 97 | 28.1 (10.6, 43.9) |
| Fasting blood glucose (≥100 mg/dL) | 311 | 43 | 1.2 (0.0, 2.9) | 11 | 5.0 (0.0, 11.2) |
| Combination of two cardiovascular health metrics | |||||
| Current smoking (yes) and blood pressure (≥120/≥80 mm Hg) | 2139 | 285 | 34.5 (23.3, 44.7) | 66 | 50.6 (24.0, 70.1) |
| Current smoking (yes) and fasting blood glucose (≥100 mg/dL) | 172 | 29 | 30.1 (20.6, 39.0) | 4 | 34.3 (11.1, 54.0) |
| Blood pressure (yes) and fasting blood glucose (≥100 mg/dL) | 160 | 27 | 8.4 (0.0, 17.4) | 8 | 31.3 (8.4, 51.0) |
| Combination of three cardiovascular health metrics | |||||
| Current smoking (yes) and blood pressure (≥120/≥80 mmHg) and fasting blood glucose (≥100 mg/dL) | 88 | 16 | 35.2 (21.7-47.4) | 2 | 52.8 (22.0-74.0) |
PAR, population-attributable risk; CVD, cardiovascular disease; CI, confidence interval; HR, hazard ratio.
1 For age, educational attainment, alcohol consumption, sleep hours, family history of CVD, and all other cardiovascular health metrics.
The individual PARs cannot be calculated for the cardiovascular health metrics with adjusted HRs ≥1.0 and statistically non-significant HRs.
where t denotes a stratum of unique combinations of levels of all background risk factors not under study, t=1,…, T; RR2t is the relative risk in combination t relative to the lowest risk level, where RR2,1=1; s indicates an index exposure group defined by each of the unique combinations of the levels of the index risk factors, i.e., the risk factors to which the PAR applies, s=1,…, S; and RR1s is the relative risk corresponding to combinations relative to the lowest risk combination, RR 1,1=1.
The joint prevalence of exposure groups and stratum t is denoted by Pst and Pt=ΣSs=1 Pst.
| Characteristic |
No. of cardiovascular health metrics |
p-trends1 | ||||
|---|---|---|---|---|---|---|
| 0-2 | 3 | 4*** | 5*** | 6-7*** | ||
| All-cause mortality | ||||||
| All deaths (n = 1054) | 87 | 246 | 371 | 284 | 66 | |
| No. of participants (n = 12 538) | 695 | 2229 | 4231 | 3932 | 1451 | |
| Total person-years | 12 522 | 40 689 | 77 637 | 72 697 | 27 145 | |
| Mortality rate (1000 PY)2 | 6.83 | 5.95 | 4.83 | 3.99 | 2.52 | <0.001 |
| Crude HR (95% CI) | 1 | 0.87 (0.68, 1.11) | 0.68 (0.54, 0.86) | 0.56 (0.44, 0.71) | 0.35 (0.25, 0.48) | <0.001 |
| Adjusted HR3 (95% CI) | 1 | 0.93 (0.73, 1.21) | 0.76 (0.59, 0.96) | 0.65 (0.51, 0.84) | 0.42 (0.31, 0.59) | <0.001 |
| CVD mortality | ||||||
| CVD deaths (n = 171) | 21 | 50 | 60 | 36 | 4 | |
| No. of participants (n = 12 538) | 695 | 2229 | 4231 | 3932 | 1451 | |
| Total person-years | 12 522 | 40 689 | 77 637 | 72 697 | 27 145 | |
| Mortality rate (1000 PY)2 | 1.62 | 1.20 | 0.78 | 0.51 | 0.16 | <0.001 |
| Crude HR (95% CI) | 1.00 | 0.73 (0.44, 1.22) | 0.46 (0.28, 0.75) | 0.29 (0.17, 0.50) | 0.09 (0.03, 0.25) | <0.001 |
| Adjusted HR3 (95% CI) | 1.00 | 0.77 (0.46, 1.29) | 0.46 (0.27, 0.76) | 0.31 (0.18, 0.53) | 0.10 (0.03, 0.29) | <0.001 |
HR, hazard ratio; CVD, cardiovascular disease; PY, person-years; CI, confidence interval.
1 For trends across the categories of cardiovascular health metrics scores based on a Satterthwaite adjusted F-test.
2 Adjusted for age.
3 For age, educational attainment, alcohol consumption, and family history of CVD.
*** p<0.001.
Figure & Data
References
Citations

- Ideal cardiovascular health and cardiovascular-related events: a systematic review and meta-analysis
Femke te Hoonte, Merve Spronk, Qi Sun, Kangrui Wu, Shiqi Fan, Ziyi Wang, Michiel L Bots, Yvonne T Van der Schouw, Alicia Uijl, Robin W M Vernooij
European Journal of Preventive Cardiology.2024; 31(8): 966. CrossRef - Parent–Offspring Associations of Ideal Cardiovascular Health Metrics: Findings From the 2014 to 2021 Korea National Health and Nutrition Examination Survey
Manh Thang Hoang, Sun Jae Jung, Hokyou Lee, Hyeon Chang Kim
Journal of the American Heart Association.2024;[Epub] CrossRef - Dietary Patterns and Cardiovascular Diseases in Asia: A Systematic Review and Meta-Analysis
Gladys Huiyun Lim, Nithya Neelakantan, Yu Qi Lee, Su Hyun Park, Zhi Heng Kor, Rob M van Dam, Mary Foong-Fong Chong, Airu Chia
Advances in Nutrition.2024; : 100249. CrossRef - Ideal cardiovascular health and risk of death in a large Swedish cohort
Lijie Ding, Marta Ponzano, Alessandra Grotta, Hans-Olov Adami, Fuzhong Xue, Ylva Trolle Lagerros, Rino Bellocco, Weimin Ye
BMC Public Health.2024;[Epub] CrossRef - Ideal cardiovascular health and mortality: pooled results of three prospective cohorts in Chinese adults
Yanbo Zhang, Canqing Yu, Shuohua Chen, Zhouzheng Tu, Mengyi Zheng, Jun Lv, Guodong Wang, Yan Liu, Jiaxin Yu, Yu Guo, Ling Yang, Yiping Chen, Kunquan Guo, Kun Yang, Handong Yang, Yanfeng Zhou, Yiwen Jiang, Xiaomin Zhang, Meian He, Gang Liu, Zhengming Chen,
Chinese Medical Journal.2023; 136(2): 141. CrossRef - Ideal cardiovascular health and all-cause or cardiovascular mortality in a longitudinal study of the Thai National Health Examination Survey IV and V
Wichai Aekplakorn, Nareemarn Neelapaichit, Suwat Chariyalertsak, Pattapong Kessomboon, Sawitri Assanangkornchai, Surasak Taneepanichskul, Somkiat Sangwatanaroj, Wasin Laohavinij, Jiraluck Nonthaluck
Scientific Reports.2023;[Epub] CrossRef - Life's Essential 8 and 10-Year and Lifetime Risk of Atherosclerotic Cardiovascular Disease in China
Cheng Jin, Jianxin Li, Fangchao Liu, Xia Li, Ying Hui, Shouhua Chen, Furong Li, Gang Wang, Fengchao Liang, Xiangfeng Lu, Shouling Wu, Dongfeng Gu
American Journal of Preventive Medicine.2023; 64(6): 927. CrossRef - Vasomotor and other menopause symptoms and the prevalence of ideal cardiovascular health metrics among premenopausal stage women
Hye Rin Choi, Yoosoo Chang, Yejin Kim, Yoosun Cho, Min-Jung Kwon, Jeonggyu Kang, Ria Kwon, Ga-Young Lim, Kye-Hyun Kim, Hoon Kim, Yun Soo Hong, Jihwan Park, Di Zhao, Juhee Cho, Eliseo Guallar, Hyun-Young Park, Seungho Ryu
Menopause.2023; 30(7): 750. CrossRef - Ideal Cardiovascular Health and Risk of Cardiovascular Events or Mortality: A Systematic Review and Meta-Analysis of Prospective Studies
Milan Radovanovic, Janko Jankovic, Stefan Mandic-Rajcevic, Igor Dumic, Richard D. Hanna, Charles W. Nordstrom
Journal of Clinical Medicine.2023; 12(13): 4417. CrossRef - Time spent in a better cardiovascular health and risk of cardiovascular diseases and mortality: a prospective cohort study
Qiuyue Tian, Shuohua Chen, Xiaoni Meng, Haotian Wang, Cancan Li, Deqiang Zheng, Lijuan Wu, Aitian Wang, Shouling Wu, Youxin Wang
Journal of Translational Medicine.2023;[Epub] CrossRef - Adding Estimated Cardiorespiratory Fitness to the Framingham Risk Score and Mortality Risk in a Korean Population-Based Cohort Study
Inhwan Lee, Jeonghyeon Kim, Hyunsik Kang
International Journal of Environmental Research and Public Health.2022; 19(1): 510. CrossRef - Ideal Cardiovascular Health Metrics and Risk of Incident Early-Onset Vasomotor Symptoms Among Premenopausal Women
Hye Rin Choi, Yoosoo Chang, Yejin Kim, Yoosun Cho, Jeonggyu Kang, Min-Jung Kwon, Ria Kwon, Ga-Young Lim, Kye-Hyun Kim, Hoon Kim, Yun Soo Hong, Jihwan Park, Di Zhao, Juhee Cho, Eliseo Guallar, Hyun-Young Park, Seungho Ryu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): 2666. CrossRef - Ideal Cardiovascular Health: Distribution, Determinants and Relationship with Health Status among People Living with HIV in Urban Tanzania
Theresia A. Ottaru, Gideon P. Kwesigabo, Zeeshan Butt, Adovich S. Rivera, Pilly Chillo, Helen Siril, Lisa R. Hirschhorn, Matthew J. Feinstein, Claudia Hawkins
Global Heart.2022; 17(1): 74. CrossRef - Spousal concordance of ideal cardiovascular health metrics: findings from the 2014–2019 Korea National Health and Nutrition Examination Survey
Manh Thang Hoang, Hokyou Lee, Hyeon Chang Kim
Clinical Hypertension.2022;[Epub] CrossRef - Further understanding of ideal cardiovascular health score metrics and cardiovascular disease
Erin D. Michos, Sadiya S. Khan
Expert Review of Cardiovascular Therapy.2021; 19(7): 607. CrossRef - Demographic and socioeconomic inequalities in ideal cardiovascular health: A systematic review and meta-analysis
Janko Janković, Stefan Mandić-Rajčević, Maša Davidović, Slavenka Janković, Kathleen Finlayson
PLOS ONE.2021; 16(8): e0255959. CrossRef - Evaluation of Dietary Patterns and All-Cause Mortality
Laural K. English, Jamy D. Ard, Regan L. Bailey, Marlana Bates, Lydia A. Bazzano, Carol J. Boushey, Clarissa Brown, Gisela Butera, Emily H. Callahan, Janet de Jesus, Richard D. Mattes, Elizabeth J. Mayer-Davis, Rachel Novotny, Julie E. Obbagy, Elizabeth B
JAMA Network Open.2021; 4(8): e2122277. CrossRef - Comparison of four healthy lifestyle scores for predicting cardiovascular events in a national cohort study
Ming-Chieh Tsai, Tzu-Lin Yeh, Hsin-Yin Hsu, Le-Yin Hsu, Chun-Chuan Lee, Po-Jung Tseng, Kuo-Liong Chien
Scientific Reports.2021;[Epub] CrossRef - Association of the Duration of Ideal Cardiovascular Health Through Adulthood With Cardiometabolic Outcomes and Mortality in the Framingham Offspring Study
Laura Corlin, Meghan I. Short, Ramachandran S. Vasan, Vanessa Xanthakis
JAMA Cardiology.2020; 5(5): 549. CrossRef - Cardiovascular health metrics and all-cause mortality and mortality from major non-communicable chronic diseases among Chinese adult population
Bixia Gao, Fang Wang, Ming Zhu, Jinwei Wang, Maigeng Zhou, Luxia Zhang, Minghui Zhao
International Journal of Cardiology.2020; 313: 123. CrossRef - Lifestyle risk score and mortality in Korean adults: a population-based cohort study
Dong Hoon Lee, Jin Young Nam, Sohyeon Kwon, NaNa Keum, Jong-Tae Lee, Min-Jeong Shin, Hannah Oh
Scientific Reports.2020;[Epub] CrossRef - Cardiovascular Health and Stroke in Older British Men
Ayesha Ahmed, Snehal M. Pinto Pereira, Lucy Lennon, Olia Papacosta, Peter Whincup, Goya Wannamethee
Stroke.2020; 51(11): 3286. CrossRef - Geographical variations in cardiovascular health in China: A nationwide population-based survey of 74,726 adults
Mei Zhang, Yu Shi, Oumin Shi, Zhenping Zhao, Xiao Zhang, Chun Li, Zhengjing Huang, Liyun Zhao, Limin Wang, Yichong Li, Xinhua Li
The Lancet Regional Health - Western Pacific.2020; 3: 100033. CrossRef - Patterns of change in cardiovascular risks of Korean male workers: a 10-year cohort analysis using the National Health Insurance Service–National Sample Cohort (NHIS-NSC) 2.0 database
Hosihn Ryu, Jiyeon Jung, Jihyun Moon
BMJ Open.2020; 10(11): e038446. CrossRef - Ideal Cardiovascular Health Status and Risk of Cardiovascular Disease or All-Cause Mortality in Chinese Middle-Aged Population
Ying Dong, Guang Hao, Zengwu Wang, Xin Wang, Zuo Chen, Linfeng Zhang
Angiology.2019; 70(6): 523. CrossRef - Status of cardiovascular health in the Republic of Serbia: Results from the National Health Survey
Janko Janković, Maša Davidović, Vesna Bjegović-Mikanović, Slavenka Janković, Olivia Manfrini
PLOS ONE.2019; 14(3): e0214505. CrossRef - Low levels of ideal cardiovascular health in a semi-urban population of Western Nepal: a population-based, cross-sectional study
Bishal Gyawali, Shiva Raj Mishra, Salim S Virani, Per Kallestrup
Heart Asia.2019; 11(1): e011131. CrossRef - Lifestyle Risk Factors and All-Cause and Cardiovascular Disease Mortality: Data from the Korean Longitudinal Study of Aging
Inhwan Lee, Shinuk Kim, Hyunsik Kang
International Journal of Environmental Research and Public Health.2019; 16(17): 3040. CrossRef - Aspirin for Primary Prevention of Cardiovascular Disease
Ji Hye Kim, Min Jung Shim, So-Young Lee, Jisu Oh, Sang Hoon Kim
Journal of Lipid and Atherosclerosis.2019; 8(2): 162. CrossRef - Optimal information networks: Application for data-driven integrated health in populations
Joseph L. Servadio, Matteo Convertino
Science Advances.2018;[Epub] CrossRef - Ideal cardiovascular health and incidence of atherosclerotic cardiovascular disease among Chinese adults: the China-PAR project
Chao Han, Fangchao Liu, Xueli Yang, Jichun Chen, Jianxin Li, Jie Cao, Ying Li, Chong Shen, Ling Yu, Zhendong Liu, Xianping Wu, Liancheng Zhao, Dongshen Hu, Xiangfeng Lu, Xigui Wu, Dongfeng Gu
Science China Life Sciences.2018; 61(5): 504. CrossRef - Life's Simple 7 and the risk of atrial fibrillation: The Multi-Ethnic Study of Atherosclerosis
Oluseye Ogunmoroti, Erin D. Michos, Konstantinos N. Aronis, Joseph A. Salami, Ron Blankstein, Salim S. Virani, Erica S. Spatz, Norrina B. Allen, Jamal S. Rana, Roger S. Blumenthal, Emir Veledar, Moyses Szklo, Michael J. Blaha, Khurram Nasir
Atherosclerosis.2018; 275: 174. CrossRef - Prevalence of the cardiovascular health status in adults: A systematic review and meta-analysis
Y. Peng, S. Cao, Z. Yao, Z. Wang
Nutrition, Metabolism and Cardiovascular Diseases.2018; 28(12): 1197. CrossRef - Low Prevalence of AHA-Defined Ideal Cardiovascular Health Factors: A Study of Urban Indian Men and Women
Balkishan Gupta, Rajeev Gupta, Krishna K. Sharma, Arvind Gupta, Tulika G. Mahanta, Prakash C. Deedwania
Global Heart.2017; 12(3): 219. CrossRef - Ideal cardiovascular health is associated with self-rated health status. The Polish Norwegian Study (PONS)
Marta Manczuk, Georgeta Vaidean, Mahshid Dehghan, Rajesh Vedanthan, Paolo Boffetta, Witold A. Zatonski
International Journal of Cardiology.2017; 230: 549. CrossRef - Favorable Cardiovascular Health Is Associated With Lower Health Care Expenditures and Resource Utilization in a Large US Employee Population
Chukwuemeka U. Osondu, Ehimen C. Aneni, Javier Valero-Elizondo, Joseph A. Salami, Maribeth Rouseff, Sankalp Das, Henry Guzman, Adnan Younus, Oluseye Ogunmoroti, Theodore Feldman, Arthur S. Agatston, Emir Veledar, Barry Katzen, Chris Calitz, Eduardo Sanche
Mayo Clinic Proceedings.2017; 92(4): 512. CrossRef - High Level Physical Activity and Prevalence of Cardiovascular Disease Using the Korea National Health and Nutrition Examination Survey Data, 2007-2013
Kyounghoon Park, Byung-Joo Park
Journal of Preventive Medicine and Public Health.2017; 50(5): 320. CrossRef - Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: A meta‐analysis of prospective studies
Leilei Guo, Shangshu Zhang
Clinical Cardiology.2017; 40(12): 1339. CrossRef - Life's Simple 7 and Incident Heart Failure: The Multi‐Ethnic Study of Atherosclerosis
Oluseye Ogunmoroti, Ebenezer Oni, Erin D. Michos, Erica S. Spatz, Norrina B. Allen, Jamal S. Rana, Salim S Virani, Ron Blankstein, Konstantinos N. Aronis, Roger S. Blumenthal, Emir Veledar, Moyses Szklo, Michael J. Blaha, Khurram Nasir
Journal of the American Heart Association.2017;[Epub] CrossRef - Estimates of Mortality Benefit From Ideal Cardiovascular Health Metrics: A Dose Response Meta‐Analysis
Ehimen C. Aneni, Alessio Crippa, Chukwuemeka U. Osondu, Javier Valero‐Elizondo, Adnan Younus, Khurram Nasir, Emir Veledar
Journal of the American Heart Association.2017;[Epub] CrossRef - Traditional Risk Factors of Acute Coronary Syndrome in Four Different Male Populations – Total Cholesterol Value Does Not Seem To Be Relevant Risk Factor
J. A. HUBACEK, V. STANEK, M. GEBAUEROVA, V. ADAMKOVA, V. LESAUSKAITE, D. ZALIADUONYTE-PEKSIENE, A. TAMOSIUNAS, A. SUPIYEV, A. KOSSUMOV, A. ZHUMADILOVA, J. PITHA
Physiological Research.2017; : S121. CrossRef - Association of Life's Simple 7 and presence of cardiovascular disease in general Australians
Yang Peng, Zhiqiang Wang
Open Heart.2017; 4(2): e000622. CrossRef - A Systematic Review of the Prevalence and Outcomes of Ideal Cardiovascular Health in US and Non-US Populations
Adnan Younus, Ehimen C. Aneni, Erica S. Spatz, Chukwuemeka U. Osondu, Lara Roberson, Oluseye Ogunmoroti, Rehan Malik, Shozab S. Ali, Muhammad Aziz, Theodore Feldman, Salim S. Virani, Wasim Maziak, Arthur S. Agatston, Emir Veledar, Khurram Nasir
Mayo Clinic Proceedings.2016; 91(5): 649. CrossRef - Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: A meta-analysis
Na Fang, Menglin Jiang, Yu Fan
International Journal of Cardiology.2016; 214: 279. CrossRef - Ideal Cardiovascular Health Metrics and Incident Hyperuricemia
Zheng Li, Lingmin Meng, Zhe Huang, Liufu Cui, Weijuan Li, Jingsheng Gao, Zhanqi Wang, Rui Zhang, Jing Zhou, Ge Zhang, Shuohua Chen, Xiaoming Zheng, Hongliang Cong, Xiang Gao, Shouling Wu
Arthritis Care & Research.2016; 68(5): 660. CrossRef - Association between ideal cardiovascular health and the atherogenic index of plasma
Shiwei Shen, Yun Lu, Huajin Qi, Feng Li, Zhenhai Shen, Liuxin Wu, Chengjian Yang, Ling Wang, Kedong Shui, Yaping Wang, Dongchang Qiang, Jingting Yun, Xiaofeng Weng
Medicine.2016; 95(24): e3866. CrossRef - Prevalence and distribution of ideal cardiovascular health metrics and association with metabolic syndrome in Japanese male workers
Masao Kanauchi, Kimiko Kanauchi
International Journal of Cardiology.2016; 221: 428. CrossRef - Changes in Cardiovascular Health Status and the Risk of New-Onset Hypertension in Kailuan Cohort Study
Fei Gao, Xiaoxue Liu, Xizhu Wang, Shouhua Chen, Jihong Shi, Ying Zhang, Shouling Wu, Jun Cai, Vincenzo Lionetti
PLOS ONE.2016; 11(7): e0158869. CrossRef - Association Between Life's Simple 7 and Noncardiovascular Disease: The Multi‐Ethnic Study of Atherosclerosis
Oluseye Ogunmoroti, Norrina B. Allen, Mary Cushman, Erin D. Michos, Tatjana Rundek, Jamal S. Rana, Ron Blankstein, Roger S. Blumenthal, Michael J. Blaha, Emir Veledar, Khurram Nasir
Journal of the American Heart Association.2016;[Epub] CrossRef - Comparison of Prevalence- and Smoking Impact Ratio-Based Methods of Estimating Smoking-Attributable Fractions of Deaths
Kyoung Ae Kong, Kyung-Hee Jung-Choi, Dohee Lim, Hye Ah Lee, Won Kyung Lee, Sun Jung Baik, Su Hyun Park, Hyesook Park
Journal of Epidemiology.2016; 26(3): 145. CrossRef - Status of Cardiovascular Health in Chinese Adults
Yufang Bi, Yong Jiang, Jiang He, Yu Xu, Limin Wang, Min Xu, Mei Zhang, Yichong Li, Tiange Wang, Meng Dai, Jieli Lu, Mian Li, Chung-Shiuan Chen, Shenghan Lai, Weiqing Wang, Linhong Wang, Guang Ning
Journal of the American College of Cardiology.2015; 65(10): 1013. CrossRef - Understanding and Improving Cardiovascular Health: An Update on the American Heart Association's Concept of Cardiovascular Health
Christina M. Shay, Holly S. Gooding, Rosenda Murillo, Randi Foraker
Progress in Cardiovascular Diseases.2015; 58(1): 41. CrossRef - Prevalência de saúde cardiovascular ideal na população brasileira - Pesquisa Nacional de Saúde (2013)
Gustavo Velasquez-Melendez, Mariana Santos Felisbino-Mendes, Fernanda Penido Matozinhos, Rafael Claro, Crizian Saar Gomes, Deborah Carvalho Malta
Revista Brasileira de Epidemiologia.2015; 18(suppl 2): 97. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


