The Association Among Individual and Contextual Factors and Unmet Healthcare Needs in South Korea: A Multilevel Study Using National Data
Article information
Abstract
Objectives
The objective of this study is to investigate associations between contextual characteristics and unmet healthcare needs in South Korea after accounting for individual factors.
Methods
The present study used data from the 2012 Korean Community Health Survey (KCHS) of 228 902 adults residing within 253 municipal districts in South Korea. A multilevel analysis was conducted to investigate how contextual characteristics, defined by variables that describe the regional deprivation, degree of urbanity, and healthcare supply, are associated with unmet needs after controlling for individual-level variables.
Results
Of the surveyed Korean adults, 12.1% reported experiencing unmet healthcare needs in the past. This figure varied with the 253 districts surveyed, ranging from 2.6% to 26.2%. A multilevel analysis found that the association between contextual characteristics and unmet needs varied according to the factors that caused the unmet needs. The degree of urbanity was associated with unmet need due to “financial burden” (odds ratio [OR], 0.53; 95% confidence interval [CI], 0.42 to 0.66 for rural vs. metropolitan), but not unmet need due to “service not available when needed.” There were no significant associations between these unmet need measures and regional deprivation. Among individual-level variables, income level showed the highest association with unmet need due to “financial burden” (OR, 5.63; 95% CI, 4.76 to 6.66), while employment status showed a strong association with unmet need due to “service not available when needed.”
Conclusions
Our finding suggests that different policy interventions should be considered for each at-risk population group to address the root cause of unmet healthcare needs.
INTRODUCTION
Although the Korean government contributed to making healthcare more accessible by establishing universal healthcare coverage in 1989, the rate of unmet healthcare needs in South Korea (hereafter Korea) remains high due to high levels of out-of-pocket payment caused by limited benefit coverage [1]. According to the Korea National Health and Nutrition Examination Survey (KNHANES), in Korea, the rate of unmet healthcare needs has decreased from 22.8% in 2008 to 16.7% in 2012 [2]. However, as of 2012, compared to the average 6.4% rate of unmet healthcare needs in 28 countries in the European Union, the rate in Korea is almost three times higher and the gap based on income levels has not decreased [2,3].
Existing studies pertaining to unmet healthcare needs have focused primarily on identifying the prevalence of self-reported unmet healthcare needs and analyzing individual-level predictors. According to studies conducted in the US, where unmet healthcare need research is the most active, health insurance coverage and income level were the greatest predictors of unmet healthcare needs [4-6]. Income level was a strong predictor of unmet healthcare needs even in Canada and European countries adopting universal healthcare. In addition, gender, self-reported health, educational level, and chronic diseases status were associated with unmet healthcare needs [4-10].
On the other hand, regional contextual characteristics have been gaining attention as a potential determinant of healthcare utilization [11]. In order to more accurately identify the effects of contextual characteristics, it is worth taking a closer look at the multilevel analysis method. Multilevel analysis is considered a very useful method in studying the association between individuals’ health and contextual characteristics, in that it allows simultaneous examination of the effects of higher-level and lower-level predictors. Despite the scarcity of studies on contextual-level correlates of variables of unmet need, some studies have confirmed the influence of regional socioeconomic characteristics on unmet healthcare need even when controlling for individual-level characteristics [1,7,12,13]. Nevertheless, the region-level variables examined in these studies were limited to the number of hospital beds and physicians [1], or the samples were drawn from a single state [12,13], making it difficult to generalize the findings. A US study [7] examined the association between unmet healthcare needs and material deprivation measured by poverty rate, unemployment rate, and educational level. However, the study failed to incorporate the concept of social deprivation, which has emerged as a valuable index in recent years. As such, it falls short of reflecting complex regional characteristics influencing residents’ health.
In this context, more complex measures, namely deprivation indices, that include various factors such as income, employment, education, crime, housing environment, and social networks were developed. Prior studies have proven that the deprivation index is associated with mortality and life expectancy [14,15] as well as physical and mental health status, including subjective health status [16-19]. Moreover, a few studies have demonstrated associations between the index and health service use, including medical and dental visits [16,20,21]. These studies reported that the average health status was poor and healthcare use was higher in regions with severe deprivation.
The present study, which concerns the association between unmet healthcare needs and contextual characteristics, is differentiated from existing studies in the following ways. First, a multilevel analysis was used to consider, simultaneously, the effects of both individual and contextual characteristics on unmet healthcare needs. Second, for the regional characteristics variable, the study adopted a composite deprivation index, which integrates a region’s material and social deprivation. This study is the first Korean study examining the association between a regional deprivation index and unmet healthcare needs. Third, the reasons for unmet healthcare needs, which vary by individual, include financial burden, time constraints, and mildness of symptoms; despite the fact that the effects on regional variables and policy-based intervention measures are expected to vary depending on these reasons [4], most preceding studies failed to distinguish these issues in their analyses. This study conducted a multilevel analysis for each individual cause of unmet healthcare needs.
METHODS
Conceptual Model
The objective of this study is to estimate the associations of contextual characteristics such as deprivation or other indicators of socioeconomic context with individual-level outcomes (unmet healthcare needs) after adjustment for individual-level measures. We also hypothesized that an association between contextual characteristics and unmet healthcare needs would vary for two common reasons (“financial burden” and “service not available when needed”).
Despite the myriad of available studies pertaining to region-level characteristics and health outcomes, most studies in their analyses have used widely available yet limited data sources such as the population census data to extract contextual variables in the absence of conceptual frameworks [22]. In order to gain a comprehensive understanding of the individual-level or region-level variables that influence unmet healthcare needs, the present study uses Andersen and Davidson’s healthcare utilization behavior model [11]. This framework is built upon Andersen’s initial model [23], which contains three sets of predictive factors in explaining individual characteristics influencing healthcare utilization behavior: predisposing, enabling, and need factors. The present study incorporates communities’ contextual characteristics as a determinant of healthcare utilization behavior, which is subsequently categorized into predisposing, enabling, and need factors. Based on this new model, contextual factors known and predicted to be associated with unmet healthcare needs by previous studies are selected for the analysis model.
Data Sources
This study used data from the 2012 Korean Community Health Survey (KCHS) by the Korea Centers for Disease Control and Prevention (KCDC) [24,25]. The KCHS was selected as a source of national certified statistics (No. 10118). This nationwide health survey covers information on demographic and socioeconomic characteristics, health status, and healthcare utilization. The 2012 KCHS was conducted on an average of 900 subjects selected by the probability proportional to sampling method and the systematic sampling method among adults aged 19 years or older living in each area of Korea from August to October 2012. The KCHS was administered by trained interviewers in face-to-face interviews. Data was drawn from 228 921 individuals from 253 districts nationwide included in the 2012 KCHS; we omitted 19 individuals who did not provide important information including unmet healthcare needs. Finally, a total of 228 902 individuals were analyzed in this study. Eligible contextual-level data were collected from various sources.
Measures
Outcome variables
We measured subjective unmet need for healthcare based on the KCHS question: “During the past year, was there ever a time when you wanted medical care but could not get it?” A “yes” response was treated as a definition of an experience of unmet need. Regarding the question, “What are the causes of your unmet healthcare need,” “service not available when needed” (35.8%) was the most prevalent response, followed by “financial burden” (22.8%), “mildness of symptoms” (15.9%), “transportation issues” (8.4%), and “difficult to get an appointment” (2.3%). Of these responses, the two most prevalent were added as outcome variables.
Individual-level variables
Variables for access-relevant characteristics of individuals consisted of the three domains from our conceptual model. Predisposing factors included age, gender, and educational attainment. Enabling factors included having private health insurance, social support indicated by current cohabitation with spouse, current employment status, and income level. Income was divided into five levels according to respondents’ ‘monthly average household equivalent income,’ which was calculated by dividing household income by the square root of the number of household members [26]. Need variables were represented by the number of self-reported medical comorbidities including hypertension, diabetes, coronary artery disease, stroke, asthma, and arthritis. Depression history and self-reported health status were considered need factors in predicting healthcare access [27,28]. Additionally, current smoking status was analyzed as a health behavior factor [13].
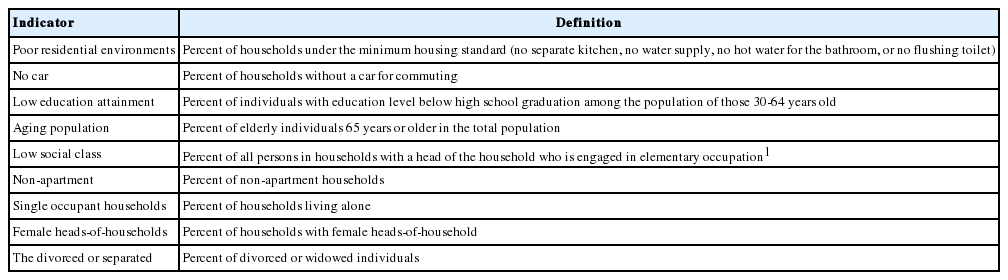
Contextual-level variables
For the contextual predisposing condition, we included the regional deprivation index and the degree of urbanity. To characterize regional deprivation, we used the composite regional deprivation index (RDI) for Korea, which was recently calculated by Kim et al. [29] using 10% of the sample survey from the 2010 census, along with district-level data. To summarize how the RDI is calculated, a total of 16 potential deprivation indices predicted to reflect regional socioeconomic statuses in Korea were obtained from the census data. Upon a distribution test, those showing irregular distribution were converted for a factor analysis. The factor analysis found that residential density and unemployment rate had negative values and, as such, were eliminated. The rate of non-homeowner status was also found to be extremely low in rural areas, and, as such, it was eliminated. As for the indices with similar implications, those with the highest factor loading values were adopted for the analysis [29]. Table 1 shows the final subordinate composition measures. The RDI was constructed by summing up the Z-standardized scores of each variable. In this study, the RDI was divided into five categories according to the score quintile. This index was found to have sufficient validity by Kim et al. [29] and previous studies have reported that the RDI index is more suitable in Korea than the Townsend or Carstairs indices, which were developed in England [29,30]. In addition, several studies have suggested that the degree of urbanity, as a region-level socioeconomic variable influencing unmet healthcare need, may influence health status and hence the need for healthcare [7,13]. Therefore, the present study incorporated urbanity, which is designated by the government (metropolitan, urban, and rural), as a contextual predisposing variable, in addition to the regional deprivation index. This study used the governmental administrative district system based on population size, industrial structure, and lifestyle to divide the autonomous areas into “metropolitan,” for districts affiliated with major cities; “urban,” for districts affiliated with cities other than major cities; and “rural,” for counties affiliated with some parts of major cities (e.g., Ongjin County in Incheon City) and provinces [31].
For the contextual enabling characteristics that may impede or facilitate individuals’ health service utilization, we selected variables pertaining to healthcare supply. So far, research into the association between supply-side factors and unmet healthcare need is sparse, and the results of available studies do not indicate a clear association [1,7,12]. To measure regional healthcare supplies, we used the number of physicians per 1000 residents in 2012 and the number of hospital beds per 1000 residents in 2011 [1,12,13]. Each variable was divided into quartiles.
Statistical Analysis
Due to the hierarchical structure of the data with 228 902 individuals (level 1) nested within 253 districts (level 2), we merged district and individual-level data using local address codes of the municipal districts and conducted a multilevel logistic regression analysis [32]. This study applied a random intercept model instead of a random coefficients regression model because the major explanatory variable, the RDI was not random for each of the 253 districts, and each region had a single fixed value. The two-level random intercept model was fit to the null model. We examined the series of models by adding contextual-level and individual-level variables. First, model 1 examined the effects of contextual-level predisposing variables (regional deprivation and degree of urbanity). Then, model 2 was analyzed, adding contextual-level enabling variables (the number of physicians and hospital beds per 1000 residents) into model 1. Finally, to examine the associations of contextual characteristics with individual-level unmet healthcare needs after adjustment for individual-level confounders, model 3 was analyzed, adding the individual-level variables into model 2. The sample for the community health survey was extracted by complex sample design. Thus, adjusted weights, which were provided by the KCHS, were included in the two-level designs to account for the design effect [32,33].
This study used two steps to determine whether there were any explanatory variables that created a multicollinearity problem. First, correlation coefficients were calculated for the explanatory variables to perform a preliminary evaluation of multicollinearity. Second, the variation inflation factor for each explanatory variable was calculated in the regression model to identify any with a value ≥3. The two evaluation steps showed that there were no variables suspected to have multicollinearity; therefore, explanatory variables presented in the study results were included in the model.
Descriptive statistics were conducted in SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) and HLM version 7.0 (Scientific Software International Inc., Lincolnwood, IL, USA) was used to conduct the multilevel analyses.
RESULTS
Baseline Characteristics of the Study Population
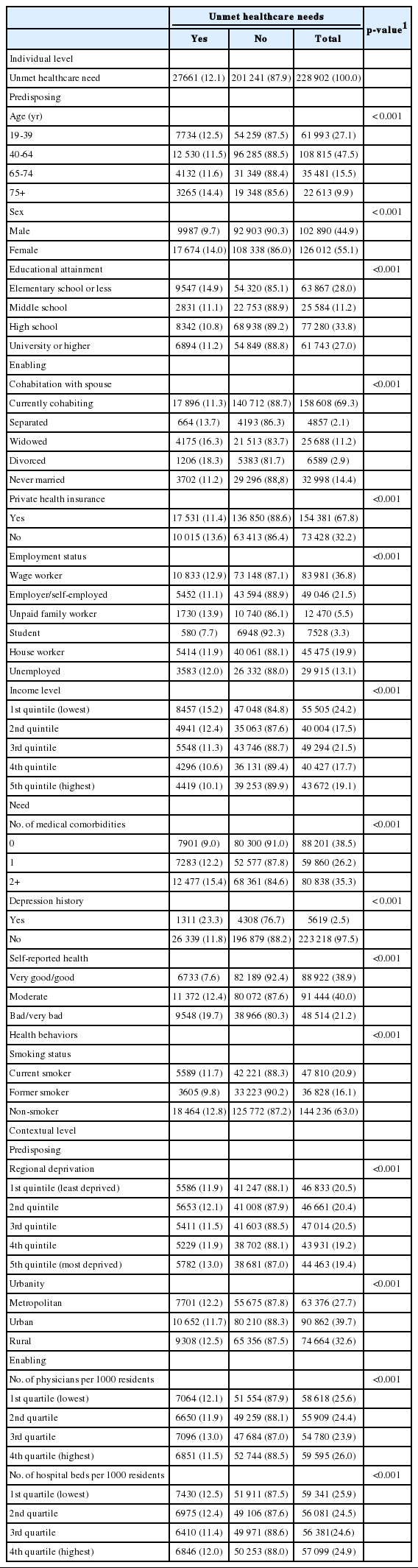
Table 2 shows the distribution of rates of unmet healthcare needs for 253 municipal districts in Korea. The mean rate of unmet healthcare needs in these districts was 12.1%, ranging from a minimum of 2.6% to a maximum of 26.2%, highlighting the disparity across districts in Korea.
Table 3 shows the rates of unmet healthcare needs based on individual-level and contextual-level variables. Unmet need was higher among individuals over 75 years of age, women, individuals with less than elementary education, divorced and widowed individuals, and individuals with lower household income. Individuals residing in the most deprived community were found to experience a greater level of unmet need compared with their counterparts residing in the least deprived community.
Multilevel Analysis Results
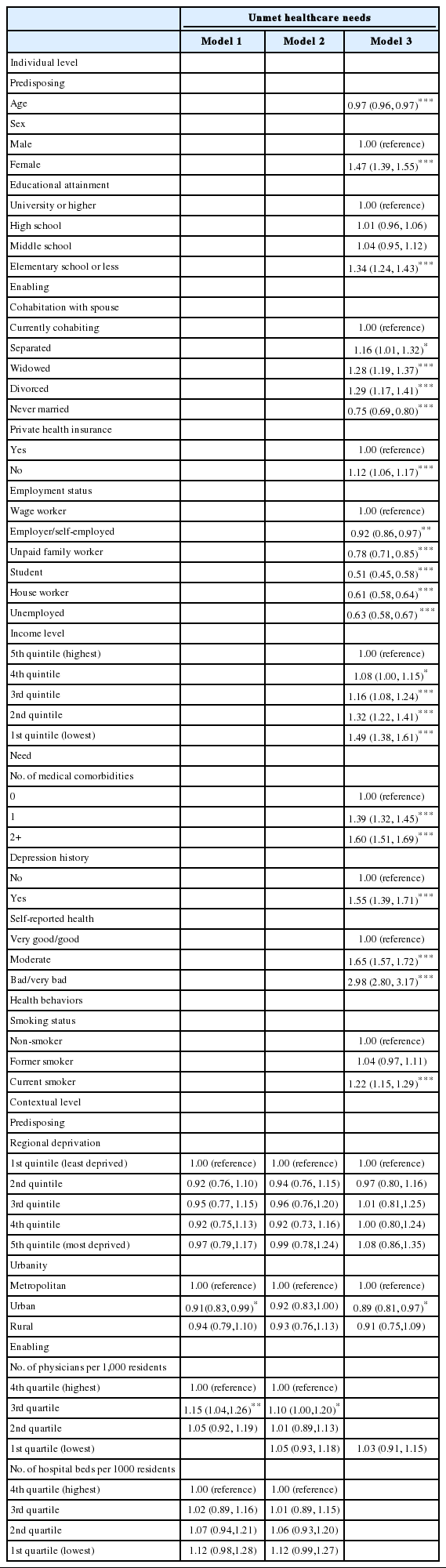
Table 4 displays the results of a multilevel logistic regression analysis performed to examine the association between individuals’ unmet healthcare needs and contextual characteristics. In the final model, urbanity among contextual variables was significantly related to unmet healthcare need; urban residents showed a reduced probability of experiencing unmet healthcare need compared to metropolitan residents (odds ratio [OR], 0.89; 95% confidence interval [CI], 0.81 to 0.97). In the case of individual-level variables, all subordinate variables were found to have a significant association with unmet need. In particular, bad or very bad self-reported health was associated with odds of unmet healthcare needs that were 2.98 times greater than very good or good self-reported health (95% CI, 2.80 to 3.17).
Table 5 displays the results of a multilevel analysis performed to test the hypothesis that the association between regional contextual variables and unmet need will vary with the causes of unmet needs. First, in cases where unmet healthcare needs occurred due to “financial burden,” regional deprivation and the degree of urbanity were associated with unmet healthcare need in model 1. However, in model 3, in which all individual-level variables were included, the association between regional deprivation and unmet need became non-significant, while urbanity variables remained statistically significant. In this model, the individual-level variable associated with the highest OR was the income level. Compared with the highest income level, the lowest income level showed 5.63 times higher odds of experiencing unmet healthcare need (95% CI, 4.76 to 6.66).

Difference of multilevel analysis results of unmet healthcare needs due to financial burden and unavailability of service when needed among Korean adults
On the other hand, in the case of unmet need due to “service not available when needed,” the significant regional variable was the number of physicians per 1000 residents. This showed an inverse relationship with unmet healthcare in only the third quartile (OR, 1.18; 95% CI, 1.04 to 1.32). The individual-level variable associated with the highest OR was bad or very bad self-reported health (OR, 2.53; 95% CI, 2.26 to 2.81), followed in order by two or more complex diseases, and female. Employment status also showed a strong relationship with unmet healthcare: the odds of the unemployed experiencing unmet healthcare was 84% lower than that for wage workers (95% CI, 0.12 to 0.19).
DISCUSSION
The present study began with the hypothesis that contextual characteristics will have a significant association with unmet healthcare need even after controlling for individuals’ compositional characteristics. In other words, we expected a region’s socioeconomic status would have a contextual effect beyond individual-level socioeconomic status on unmet healthcare need. KCHS data obtained from 228 902 individuals from 253 districts in Korea were analyzed through a multilevel analysis. Importantly, this study differed from existing, standard logistic regression analyses because the model took into account regional variation in the dependent variables (level 2), that is, unmet healthcare needs. Another reason for multilevel analysis was that 228 802 individuals belonged to 253 districts, which may not be independent of each other. For example, in the “unmet healthcare needs” model, whether someone experiences such needs may be determined by their district affiliation. This can lead to significant differences between districts, resulting in errors; this would be contrary to the assumptions in traditional methodology, and multilevel analysis would be required. To determine the fitness of multilevel analysis, an evaluation was performed, based on the null hypothesis that variance in the intercept model of unmet healthcare needs is 0 (Ho:τ00=0). Since the null hypothesis was rejected, it was confirmed that the multilevel model was fit.
While considerable research has been conducted on unmet healthcare needs in Korea using recent panel data, these studies have focused on individual determinants of unmet needs for healthcare [34-36]. The study conducted by Heo et al. [1] is the sole study examining contextual determinants of unmet needs in Korea. However, this study utilized only province-level data (from 16 provinces) of healthcare supply factors (number of hospital beds and physicians) as regional variables. The present study is important because 253 districts were analyzed, and contextual predisposing condition variables (composite deprivation index, urbanity) were used in the analysis, in addition to healthcare supply factors. In addition, unlike a number of previous studies on unmet healthcare needs that did not distinguish the cause of unmet healthcare needs [6-10,12,13,27], or only included ‘unmet healthcare needs for financial reasons’ [34], to the best of our knowledge, this is the only study to perform a multilevel analysis, classifying unmet healthcare needs by main cause.
The primary finding of this study is that, compared to regions with lower deprivation, living in regions with higher material and social deprivation is not significantly associated with an increased probability of unmet healthcare needs. In the case of the model of unmet need due to “financial burden,” the statistical significance of the regional deprivation index was observed in models 1 and 2, for which individual level variables were not included. However, such an association became nonsignificant in the final model. The following reasons may explain this finding. First, the association between the deprivation index and unmet need observed in models 1 and 2 may be attributable to individuals’ compositional characteristics. This pattern is consistent with some previous work, in which most of the association of deprivation and health was explained by individual rather than area factors [17,22,37]. Second, the use of the composite measure may have offset the influence of subordinate indices [19]. In contrast to the present study, which used a composite deprivation index combining separate indicators into one index, a US study measuring separate indices such as poverty rate [12,13] confirmed that region-level variables and unmet need were correlated even after controlling for individual-level variables. Comparing the present study’s results against such findings, it can be inferred that regional deprivation was nonsignificant in the present study because of the use of the composite measure. However, as opposed to focusing on identifying the separate regional variables that influence unmet healthcare need, the present study focused on investigating the effects of the overall nature of the regional socioeconomic context on individuals’ unmet needs. Follow-up studies further investigating the potential association between unmet healthcare need and regional deprivation via various measures of regional characteristics would be beneficial in that results can be compared to gain more specific and useful insight into the topic.
Whereas the association between the regional deprivation index and unmet need was nonsignificant, urbanity variables were found to be significantly correlated with unmet need due to “financial burden.” Specifically, living in metropolitan areas increased the likelihood of experiencing unmet healthcare needs over living in rural or urban areas. Such a finding is contrasted against the finding of a US study that reported that living in a metropolitan statistical area was not correlated with unmet healthcare needs [7] or that of another prior study that found living in smaller urban areas (population less than one million) to be more highly correlated with unmet healthcare needs than living in more populous urban areas [13]. Heo et al. [1] suggested several possible causes behind the high unmet need in major Korean cities despite the concentration of healthcare resources. Areas with a surplus of private hospital beds tend to competitively acquire more beds or highly expensive equipment and encourage services not covered by insurance, which consequently increases the cost of care. The high unmet healthcare need in these areas is thought to be attributed to the low insurance coverage and high out-of-pocket payment burden imposed on Korean healthcare consumers. According to these results, it can be inferred that individuals with low socioeconomic status residing in metropolitan areas are at an elevated risk of unmet healthcare need than their counterparts residing in rural areas [18,37].
The numbers of hospital beds and physicians, which were included in the analysis model as contextual enabling conditions either impeding or facilitating healthcare utilization, were not found to be correlated with unmet healthcare need, a finding that is supported by prior studies [3,13,14]. Korea has the highest number of doctor consultations per capita among all Organization for Economic Cooperation and Development (OECD) nations and doctor accessibility is almost twice the OECD average as of 2011. The number of hospital beds per capita is also the highest of all OECD nations, with over nine beds per 1000 people as of 2011 [38]. Therefore, it is possible that the number of physicians or hospital beds is not a significant factor influencing individuals’ healthcare accessibility in Korea.
Although the associations between contextual-level variables and unmet healthcare needs were nonsignificant in this study, all of the individual-level variables were significantly associated with unmet needs. In particular, the strongest predictor of unmet need was self-reported health, a finding supported by prior studies [1,5,27]. However, when the reasons for unmet health needs were classified as “financial burden” and “service not available when needed,” there were considerable differences in the significance and the strength of correlations. For unmet healthcare needs caused by “financial burden,” the average monthly household equivalent income and subjective health status had the highest and second highest OR, respectively. This result is consistent with those of a previous study that analyzed factors related to unmet healthcare needs caused by financial reasons, using the Korea Welfare Panel data (between 2005 and 2006), and found that poorer households and poorer objective health status were associated with a higher risk of experiencing unmet healthcare needs [34]. Conversely, where the reason for unmet healthcare was cited as “service not available when needed,” the average monthly household equivalent income was not significant in some bands, though employment status was one of the strongest predictors. More specifically, employed individuals, particularly wageworkers, were more likely to experience unmet healthcare needs compared to those who were unemployed. Considering previous reviews regarding the occurrence of unmet need in Korea [39], “service not available when needed” may be attributed to Korea’s labor system, which is characterized by the longest working hours of all OECD nations [40]. In fact, according to a survey conducted by the Korea Health Panel, which incorporated a more clearly defined set of terms in investigating unmet healthcare needs, “no time to visit a clinic or hospital” topped the responses at 39.1%, followed by “financial burden of treatment” at 22.3%, similar to the present study’s findings. As of 2011, the average annual hours worked per Korean worker is 470 hours longer than that of the OECD average. The figure translates into 2.74 more months than the OECD average [40]. Such long average annual working hours are likely to impede workers from getting regular health check-ups or treatment [34,35]. In summary of these findings, ultimately, a different policy approach is needed for each at-risk population group to address the root cause of unmet healthcare need. First of all, for the socioeconomically disadvantaged population, policies that lessen the financial burden associated with healthcare services should be implemented, which include improved health insurance coverage. On the other hand, for workers with financial stability, various interventions and relevant labor policies could be considered to enable them to use the medical services they need. This needs further discussion in future studies.
This study has some limitations. First, not all contextual-level variables that influence unmet healthcare needs could be incorporated in the analysis model. An important criticism of the literature on contextual factors and health is that, despite numerous studies, scant attention has been paid to conceptualizing the particular pathways underlying the associations with ad hoc selection of contextual factors studied [22]. Heeding this criticism, we selected the variables based on Andersen’s new healthcare utilization model, which considers both the individual- and contextual-level characteristics. However, due to issues of available data, a wider range of variables including social capital and physical environment could not be incorporated. This study used an RDI, which included both material and social deprivations, as the variable representing contextual-level characteristics in measuring the associations with unmet healthcare needs. However, deprivation indices based on a population census, such as RDI, have a limitation of not incorporating variables that can reflect the characteristics of rural regions [15]. Therefore, this study added the degree of urbanity variable to the model. However, if future studies include additional contextual characteristics that reflect social support of the community, a more meaningful explanation of the associations with unmet healthcare needs would be possible.
Additionally, when two independent variables and one dependent variable are included in a single model, if the association between one of the independent variables (level 1) and the dependent variable is altered by the other independent variable (level 2), an interaction can be created. However, this study did not examine the interactions between individual and regional level variables.
Third, due to the limitations of KCHS, responses from individuals on the details of which healthcare services were unmet could not be obtained. Since the significance and meaning of unmet needs can change based on whether the unmet service was an examination, a treatment of physical or mental problems, or injury care [21], future surveys that include questions on the type of care required will allow a more systematic analysis.
In Korea, the more urbanized the area in which an individual lived, and the lower that individual’s income was, the higher the possibility of experiencing unmet need due to “financial burden.” Conversely, for individuals participating in economic activities, the possibility of occurrence of unmet healthcare due to “service not available when needed” was higher than for individuals not participating in economic activities. A region’s socioeconomic disadvantage itself, which was represented by the deprivation index, did not seem to have an effect on unmet need above and beyond what would be expected given the residents’ socioeconomic status. Our finding suggests that different policy interventions should be considered for each at-risk population group to address the root cause of unmet healthcare need.
ACKNOWLEDGEMENTS
We would like to acknowledge the Korea Centers for Disease Control and Prevention for making available the Community Health Survey data, 2012. This work was supported by a research fund from Chungnam National University.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.