Trends in Regional Disparities in Cardiovascular Surgery and Mortality in Korea: A National Cross-sectional Study
Article information
Abstract
Objectives:
Regional disparities in cardiovascular care in Korea have led to uneven patient outcomes. Despite the growing need for and access to procedures, few studies have linked regional service availability to mortality rates. This study analyzed regional variation in the utilization of major cardiovascular procedures and their associations with short-term mortality to provide better evidence regarding the relationship between healthcare resource distribution and patient survival.
Methods:
A cross-sectional study was conducted using nationwide claims data for patients who underwent coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), stent insertion, or aortic aneurysm resection in 2022. Regional variation was assessed by the relevance index (RI). The associations between the regional RI and 30-day mortality were analyzed.
Results:
The RI was lowest for aortic aneurysm resection (mean, 26.2; standard deviation, 26.1), indicating the most uneven regional distribution among the surgical procedures. Patients undergoing this procedure in regions with higher RIs showed significantly lower 30-day mortality (adjusted odds ratio [aOR], 0.73; 95% confidence interval, 0.55 to 0.96; p=0.026) versus those with lower RIs. This suggests that cardiovascular surgery regional availability, as measured by RI, has an impact on mortality rates for certain complex surgical procedures. The RI was not associated with significant mortality differences for more widely available procedures like CABG (aOR, 0.96), PCI (aOR, 1.00), or stent insertion (aOR, 0.91).
Conclusions:
Significant regional variation and underutilization of cardiovascular surgery were found, with reduced access linked to worse mortality for complex procedures. Disparities should be addressed through collaboration among hospitals and policy efforts to improve outcomes.
INTRODUCTION
Cardiovascular disease is the second leading cause of death in Korea, accounting for 33 715 deaths in 2022, or 9% of the total [1,2]. The incidence of cardiovascular disease is increasing due to the aging population, making it a major public health challenge with considerable societal costs [3-5]. Consequently, there is an urgent need for research in cardiovascular health, novel treatment strategies, and increased funding [2,6-8].
Concerns have been raised regarding regional disparities in healthcare and their potential impact on health outcomes [9]. Cardiovascular surgery is complex, requiring specialist skills and equipment; the availability of these resources directly affects patient survival. With the increasing incidence of cardiovascular disease, it is of paramount importance to expand medical services in this domain [10], including proactive prevention strategies, diagnostic evaluations, and medical procedures, such as minimally invasive interventions and coronary artery bypass surgery [11]. Despite improvements in cardiovascular disease mortality rates, regular monitoring of patients is essential [12]. The concentration of medical usage and resources in specific geographic regions can lead not only to delays in urgent surgery, but also to increases in hidden medical costs due to patients relocating to other areas [10]. This can hinder the operation of an efficient and equitable healthcare system [13]. As a result of pre-existing geographical disparities in cardiovascular disease incidence and treatment, mortality rates from cardiovascular conditions can be disproportionately affected by these dynamics in certain regions [14].
In Korea, previous research related to the accessibility of cardiovascular disease treatment has largely focused on imbalances in the utilization of medical services [10], emergency medical center accessibility [15,16], and the relevance index for specific diseases [17]. Limited research has specifically examined geographical variations in the provision of cardiovascular surgery and the associated mortality rates. A deeper understanding of regional disparities in cardiovascular mortality is vital for meaningful improvement. Shin et al. [15] evaluated the accessibility of local cardio-cerebrovascular disease centers and the correlation of accessibility with mortality rates, with the aim of determining the appropriate placement of regional cerebrovascular disease centers. Similarly, a recent study by Lim et al. [18] investigated the outcomes and challenges of the Busan Regional Cardiocerebrovascular Center project in the treatment of ST-segment elevation myocardial infarction patients over a decade. They found that despite improvements in time parameters for early reperfusion therapy, there was no significant reduction in cardiovascular mortality rates, highlighting the need for further efforts to minimize inter-hospital transfers and reduce the symptom-to-balloon time.
In contrast, the present study analyzed patients who underwent cardiovascular surgery in 2022 to investigate the relationship between regional patterns in the utilization of cardiovascular surgery and mortality rates. In addition, this study includes a policy-shaping dimension with the goal of providing data that may influence health policies in Korea. Furthermore, we aimed to suggest effective treatment strategies and approaches to improve emergency medical services for patients with cardiovascular disease.
METHODS
Data Source
This study utilized health insurance claims data provided by the Health Insurance Review & Assessment Service. This database contains various medical information, including patient demographic characteristics, diagnoses, operations, medications, and test results, and the data are highly reliable and valid [19]. Death within 30 days and the residence information of patients who underwent cardiovascular surgery were confirmed by linkage with the computerized resident registration data of the Ministry of Public Administration and Security based on each patient’s unique identifier. This computerized database contains birth and death information reported at community centers. Linkage played an instrumental role in accurately and reliably identifying the characteristics of the study participants and analyzing the patterns and outcomes of healthcare service utilization based on residency.
Study Population
A cross-sectional study was conducted using data from January 1, 2022 to December 31, 2022, including patients of all ages who underwent major cardiovascular surgical procedures during this period. The target procedures were chosen due to their high incidence in Korea and were classified as high-risk operations. Coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), percutaneous intravascular installation of stents (PIIS), and aortic aneurysm resection (AAR) were selected as the target procedures for this study. Patients were identified using health insurance medical codes for claims; the codes used are listed in Supplemental Material 1.
Statistical Analysis
The relevance index (RI) is highly useful for estimating the demand for healthcare services among local residents and assessing the efficient and equitable distribution of healthcare institutions [17]. The RI is defined as the ratio between the amount of healthcare services used by patients living in a specific region at medical institutions in that region to the total amount of services used. This ratio is used as an important indicator of patients’ preference for medical institutions in a certain region and the scope of services of medical institutions in that region [20]. This study analyzed 26 medical service areas, including Seoul, out of 29 emergency medical treatment areas [21]. This distinction was a strategic decision to better understand patterns of access to and use of healthcare services across regions. This focus on RI alone allowed us to discern regional preferences in healthcare facilities, an essential factor in strategizing healthcare distribution.
Our investigation harnessed the RI to identify regional variations in cardiovascular procedure utilization. Regions were stratified into high, medium, and low RI groups, aligning with emergency zone distributions [22]—a method widely recognized in volume-outcome research. We employed a generalized estimation equation model at the patient level, adjusting for the clustering effect, to explore the associations between mortality rates and the regional RI. We conducted a comprehensive analysis that incorporated key covariates, such as age, sex, insurance type, and the Charlson comorbidity index (CCI). All data processing and statistical examinations were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA), with a rigorously defined 5% threshold for statistical significance. This methodical approach was chosen in order to generate robust results regarding the crucial role of regional health service analysis in optimizing healthcare delivery and fulfilling community health requirements.
Ethics Statement
This study received an exemption from review by the Korea University Bioethics Committee (KUIRB-2023-0318-01). In accordance with the National Health Insurance Act, the data in this study were used only for research purposes, and patient data were coded to prevent personal identification.
RESULTS
Patient Characteristics
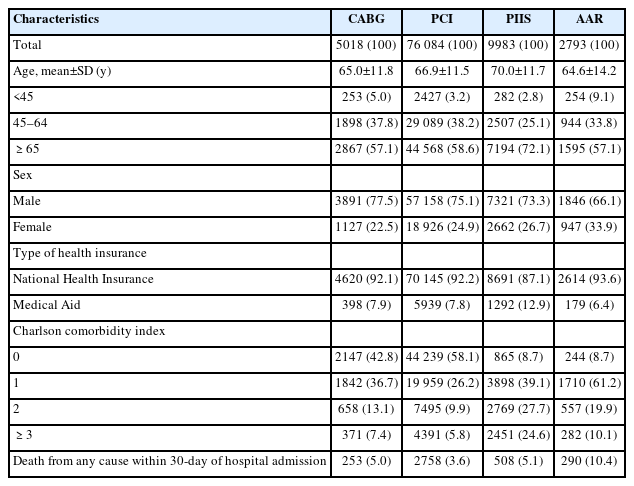
The general characteristics of patients who underwent major cardiovascular procedures are presented in Table 1. Patients who underwent PIIS had a higher average age (70.0 years) than those who underwent other procedures. Across all surgical interventions, the number of male patients was 2-3 times higher than the number of female patients. Patients who underwent PIIS were more likely to have relatively extensive comorbidities (CCI ≥3, 24.6%) than those who underwent CABG (CCI ≥3, 7.4%), PCI (CCI ≥3, 5.8%), or AAR (CCI ≥3, 10.1%). The 30-day post-admission mortality rate for AAR (10.4%) was notably higher than that for PIIS (5.1%), CABG (5.0%), and PCI (3.6%) (Table 1).
Regional Variability
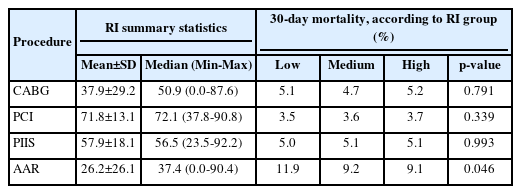
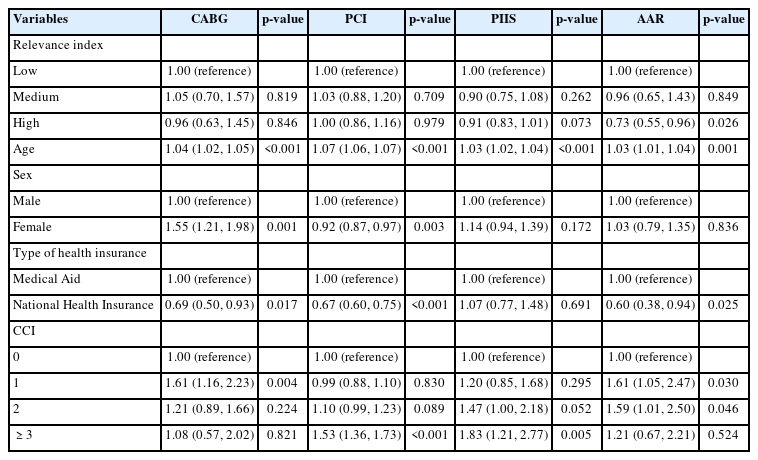
As shown in Table 2, PCI exhibited the highest mean RI (71.8), whereas AAR had the lowest (26.2). The mean RIs for CABG and PIIS were 37.9 and 57.9, respectively. Patients who underwent AAR in regions with a high RI had a significantly lower 30-day mortality rate (9.1%) than those who underwent AAR in regions with a low RI (11.9%). This suggests that regional service variability impacted patient outcomes. Conversely, PCI, CABG, and PIIS did not exhibit significant differences in 30-day mortality rates across the RI groups (Figures 1 and 2, Table 2, and Supplementary Material 2).
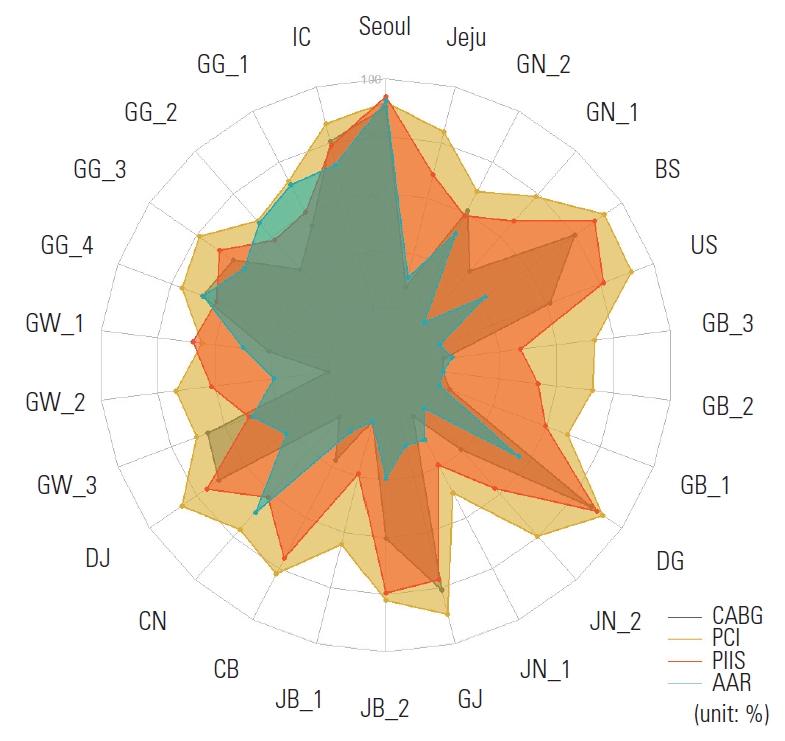
Composite relevance index for emergency medical services across 26 regions in Korea. IC, Incheon; GG_1, Gyeonggi Northwest; GG_2, Gyeonggi Northeast; GG_3, Gyeonggi Southwest; GG_4, Gyeonggi Southeast; GW_1, Gangwon East; GW_2, Gangwon Chuncheon; GW_3, Wonju Chungju; DJ, Daejeon; CN, Chungnam Cheonan; CB, Chungbuk Cheongju; JB_1, Jeonbuk Iksan; JB_2, Jeonbuk Jeonju; GJ, Gwangju; JN_1, Jeonnam Mokpo; JN_2, Jeonnam Suncheon; DG, Daegu; GB_1, Gyeongbuk Andong; GB_2, Gyeongbuk Gumi; GB_3, Gyeongbuk Pohang; US, Ulsan; GN_1, Gyeongnam Changwon; GN_2, Gyeongnam Jinju; BS, Busan; CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention; PIIS, percutaneous intravascular stent; AAR, aortic aneurysm resection.
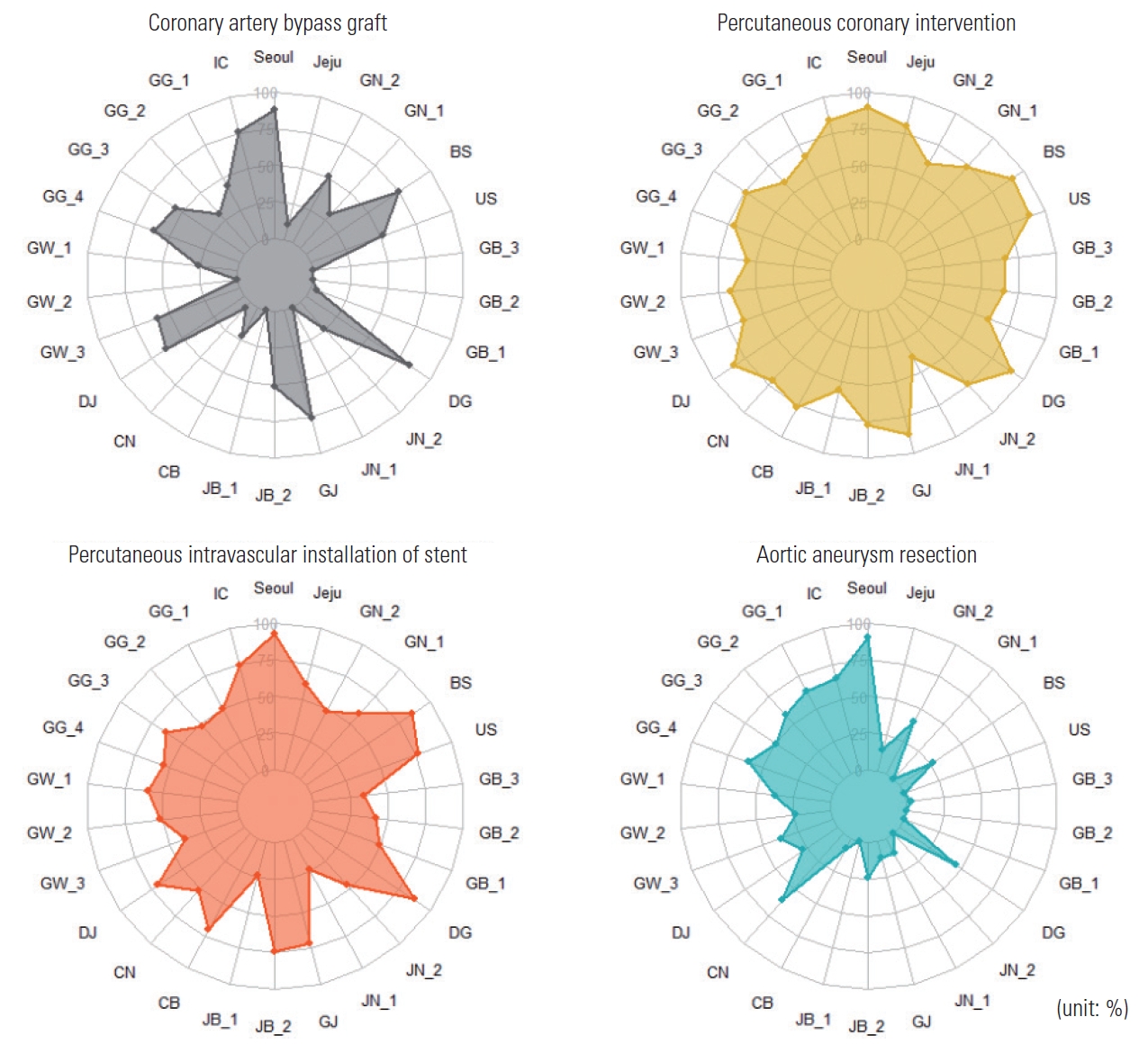
The relevance index for specific cardiovascular procedures across 26 regions defined for emergency medical services in Korea. IC, Incheon; GG_1, Gyeonggi Northwest; GG_2, Gyeonggi Northeast; GG_3, Gyeonggi Southwest; GG_4, Gyeonggi Southeast; GW_1, Gangwon East; GW_2, Gangwon Chuncheon; GW_3, Wonju Chungju; DJ, Daejeon; CN, Chungnam Cheonan; CB, Chungbuk Cheongju; JB_1, Jeonbuk Iksan; JB_2, Jeonbuk Jeonju; GJ, Gwangju; JN_1, Jeonnam Mokpo; JN_2, Jeonnam Suncheon; DG, Daegu; GB_1, Gyeongbuk Andong; GB_2, Gyeongbuk Gumi; GB_3, Gyeongbuk Pohang; US, Ulsan; GN_1, Gyeongnam Changwon; GN_2, Gyeongnam Jinju; BS, Busan.
Table 3 summarizes the association between the RI and 30- day mortality in patients who underwent major cardiac procedures. The RI, categorized as low, medium, or high, showed a statistically significant association with the 30-day mortality rate of AAR; specifically, patients in the high-RI group had a lower mortality rate than those in the low-RI group (adjusted odds ratio [aOR], 0.73; p=0.026). Age was a significant predictor of 30-day mortality across all procedures, with the risk of death increasing with age. Female who underwent CABG had a higher risk of 30-day mortality than male (aOR, 1.55; p=0.001). However, female had a lower risk of 30-day mortality than male following the other procedures. The type of health insurance emerged as a determining factor; patients with health insurance had a lower 30-day mortality rate than those with Medical Aid. An increase in the number of comorbidities was associated with a higher risk of 30-day mortality.
DISCUSSION
This study analyzed regional variations in major cardiovascular procedures using the RI and investigated their impact on mortality rates within 30 days of admission. Among the procedures, only AAR showed a relationship, wherein regions with a high RI for this procedure had a significantly lower mortality rate. The RI for AAR averaged 26.2, with a high RI of 90.4 in the Seoul metropolitan area and lower RIs elsewhere. Despite an annual increase of 3.3% in the total number of specialists nationwide over the past decade, the growth rate for specialties, including thoracic surgery, was only 1.2-2.2% [23], highlighting the shortage of expertise in essential medical fields [24]. In 2022, only 47.9% of thoracic surgery residencies were filled, compared to the overall rate of 78.5%, indicating that the national shortage of specialists in this field is not being resolved. These shortages result in regional disparities. Gangwon Province, for instance, has seen a reduction in emergency room operations and a shortage of health center physicians [25], emphasizing the need for policy interventions and resource redistribution to strengthen medical service equity and responsiveness, especially considering the importance of the “golden hour” [26].
AAR is predominantly performed in Seoul and its surrounding areas, with some regions showing an RI of 0. Patients in regions such as Andong, Gumi, and Pohang in Gyeongsangbuk Province, Ulsan and Changwon in Gyeongsangnam Province, and Suncheon in Jeonnam Province had markedly limited access to AAR, likely due to the lack of essential medical personnel, such as thoracic surgeons [27]. However, it is important to note that the RI, which is based on administrative districts, may have limitations for analyzing time-sensitive cardiovascular diseases where the golden hour is crucial. Future studies could explore the relationship between the RI and the timely medical service utilization rate to provide a more comprehensive understanding of regional disparities in access to cardiovascular care. In this context, the Second Comprehensive Plan for Cardiovascular Diseases (2023-2027) aims to improve surgical treatment and establish new standards for a number of procedures, such as CABG, aortic surgery, and valve surgery [28,29]. Such initiatives are expected to mitigate the regional disparities highlighted by our study, ensuring that all patients, regardless of their location, have access to high-quality cardiovascular care. Our study found that PCI had the highest RI, whereas AAR had the lowest. Notably, the 30-day mortality rate following AAR was significantly lower in high-RI regions than in low-RI regions, suggesting an association between RI and patient survival. Conversely, patients undergoing PCI, CABG, and PIIS did not exhibit significant differences in 30-day mortality rates across the RI groups, indicating that the RI did not significantly influence survival following these procedures. The government has introduced a specialized network for responding to conditions, such as acute myocardial infarction, cerebral hemorrhage, and cerebral infarction [29]. There are 2 types of networks: an inter-institutional network based on regional cardiovascular disease centers and a human network based on specialists. The regional cardiovascular disease center-based network type is at the hospital level, and the human network pilot project is at the person level. These networks aim to ensure the timely and appropriate treatment of severe cardiovascular emergencies, ultimately improving patient outcomes and optimizing regional medical resource allocation. The success observed in acute stroke care, with lower case-fatality rates achieved through specialized treatment strategies, provides a compelling model for cardiovascular care [30]. It suggests that fostering a specialized treatment human network, which could involve coordination among cardiologists, surgeons, and other healthcare professionals within and across healthcare facilities, is crucial. Such a network would not only streamline the referral and treatment processes but also ensure that patients have timely access to the most appropriate and highest-quality care available, regardless of their initial point of contact with the healthcare system.
However, our study has several limitations that should be acknowledged. First, while the quality of care at medical institutions significantly impacts mortality, our analysis did not adjust for this critical aspect. The 2020 Coronary Artery Bypass Grafting Appropriateness Evaluation Report found that although the overall quality of CABG in Korea is high, there is a notable concentration of quality care in the Seoul and Gyeonggi regions, underscoring regional disparities [31]. Second, we did not account for the emergency status of surgical procedures. Jang et al. [32] reported that about one-third of PCIs in Korea are emergency procedures, suggesting that the emergency nature of operations, while potentially significant, may have a limited impact on mortality due to the regional distribution and accessibility of care. The need to consider the emergency status of operations in future research is clear, as it remains a crucial factor affecting outcomes.
This study highlights the significant role of the RI in understanding regional disparities in mortality rates following cardiovascular surgery in Korea. Regions with higher RIs, indicating better healthcare accessibility, were associated with lower mortality rates, especially for AAR procedures. This underscores the importance of improving healthcare accessibility and quality across the country to improve patient outcomes. Strengthening healthcare infrastructure, including establishing a comprehensive professional care human network and optimizing patient transfer systems, is crucial for providing timely treatment and addressing cardiovascular disease effectively.
In conclusion, acknowledging the limitations of our study provides a foundation for future research to explore the impact of emergency status, quality of care, and regional disparities on cardiovascular care outcomes. By addressing these gaps, we can work toward optimizing healthcare delivery and ensuring that all patients, regardless of their location, have access to high-quality cardiovascular care.
Supplemental Materials
Supplemental materials are available at https://doi.org/10.3961/jpmph.24.057.
Supplemental Material 1.
Health insurance fee code for major cardiovascular procedures
Supplemental Material 2.
Relevance Index by 26 regions for emergency medical services
Notes
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
Funding
This research was supported by a grant from the Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (grant No. HC21C0114).
Author Contributions
Conceptualization: Jin DL, Kim KH, Chung ES, Yoon SJ. Data curation: Kim KH. Formal analysis: Kim KH. Funding acquisition: Yoon SJ. Methodology: Jin DL, Kim KH, Chung ES, Yoon SJ. Visualization: Jin DL. Writing – original draft: Jin DL. Writing – review & editing: Kim KH, Chung ES, Yoon SJ.
Acknowledgements
None.