Postpartum Depression in Young Mothers in Urban and Rural Indonesia
Article information
Abstract
Objectives
Young mothers are vulnerable to postpartum depression due to role transition-related stress. Understanding the causes underlying these stressors is essential for developing effective interventions.
Methods
This study analyzed the 2018 Indonesian Basic Health Research data. The Mini International Neuropsychiatric Interview was used to assess postpartum depression symptoms in mothers aged 15-24 years with infants aged 0-6 months. In 1285 subjects, the risk factors for postpartum depression were evaluated using multivariate logistic regression.
Results
The overall prevalence of depression in the 6 months postpartum was 4.0%, with a higher prevalence in urban areas (5.7%) than in rural areas (2.9%). Urban and rural young mothers showed distinct postpartum depression risk factors. In urban areas, living without a husband (odds ratio [OR], 3.82; 95% confidence interval [CI], 1.24 to 11.76), experiencing preterm birth (OR, 4.67; 95% CI, 1.50 to 14.50), having pregnancy complications (OR, 3.03; 95% CI, 1.20 to 7.66), and having postpartum complications (OR, 5.23; 95% CI, 1.98 to 13.80) were associated with a higher risk of postpartum depression. In rural areas, postpartum depression was significantly associated with a smaller household size (OR, 3.22; 95% CI, 1.00 to 10.38), unwanted pregnancy (OR, 4.40; 95% CI, 1.15 to 16.86), and pregnancy complications (OR, 3.41; 95% CI, 1.31 to 8.88).
Conclusions
In both urban and rural contexts, postpartum depression relates to the availability of others to accompany young mothers throughout the postpartum period and offer support with reproductive issues. Support from the family and the healthcare system is essential to young mothers’ mental health. The healthcare system needs to involve families to support young mothers’ mental health from pregnancy until the postpartum period.
INTRODUCTION
Maternal health is crucial for ensuring the health of the next generation. Maternal health includes pregnancy, childbirth, and the postpartum period. Postpartum depression (PPD), which affects 10-15% of mothers, is the most common psychological health problem affecting women worldwide [1]. PPD is often defined as an episode of major depressive disorder (though it may also include minor depression) that occurs in the postpartum period [2]. PPD is often distinguishable from postpartum blues, which typically appear 3 days to 5 days after giving birth and are frequent (incidence of 40-80%), moderate, and transient mood problems [3]. PPD is mainly reported until 6 months postpartum, but in clinical practice and many research studies, time frames ranging up to 1 year or 2 years are also used to define the postpartum period.
In Indonesia, the prevalence of PPD ranges from 2.3% to 22.0%, depending on factors such as PPD testing procedures, assessment time, cut-off values, and population characteristics [4]. Previous research on PPD in Indonesia revealed that risk factors include low income, low educational background, primigravida [5,6], low birth weight, prematurity [6], and lack of social support [5]. The prevalence of PPD in adolescent mothers is almost double that of adult mothers. Adolescent mothers reported a PPD prevalence ranging from 14% to 53% [7,8]. Furthermore, a large body of data indicates that a maternal age between 15 years and 24 years is an essential risk factor for PPD [9]. Young mothers encounter more significant psychological challenges, such as social isolation, being a single parent, family conflict, low self-esteem, primiparity, and body dissatisfaction, which may increase the risk of depression [10,11].
An earlier study on PPD in Indonesian urban and rural areas has not shown conclusive findings. Moreover, the study investigated PPD in all age groups or adult groups, although its findings showed that the prevalence of PPD almost doubled in young mothers [12]. According to a 2022 report of the Indonesian National Statistical Agency, youth aged 15-24 years account for 16.19% of the population [13], or approximately 44 million people. In an Indonesian study of all reproductive ages, young mothers were more likely to experience risk factors for PPD than their older counterparts [14]. The Health Action Plan proposed by the Indonesian Ministry of Health emphasizes equitable access to healthcare services and the importance of maternal health [15]. An earlier study in Indonesia nonetheless found significant differences in PPD in rural and urban settings [6]. There are study about PPD in rural areas, but only in Central Java region and not specific to young mothers [16].
Given the enormous potential of young mothers and the risk of developing PPD, we aimed to determine the magnitude of the problem and the factors associated with the incidence of PPD among young mothers in rural and urban Indonesia.
METHODS
Data Sources
Data on PPD were obtained from the Indonesia Basic Health Survey (RISKESDAS) 2018, a national health survey conducted by the Indonesian Ministry of Health. The RISKESDAS is a 5-yearly cross-sectional survey that collects basic health indicators to depict the status of community health at the district/city, provincial, and national levels. The 2018 RISKESDAS data collection was carried out in 34 provinces and 514 regencies/cities in Indonesia using the probability proportional to size method. Systematic linear sampling was performed, with 2-stage sampling yielding 10 selected households in 1 census block [17]. All members of each selected household (those who had resided on the premises for the past 6 months or more and who had the same source of sustenance funding) were requested to participate in the survey [18].
Subjects
The subjects in the current analysis were mothers in the RISKESDAS sample who were aged 15-24 years with babies aged ≤6 months. The analysis included women who had biological babies aged 0-24 weeks and complete information on the variables studied. This study excluded subjects with severe pain and those who did not have full answers to all questions. The reason for limiting the age of participant children to 6 months was to reduce the risk that factors other than postpartum reproductive health factors may have caused maternal depression. These criteria were met by 1285 subjects.
Outcome Variables
The outcome of this study was PPD, as measured using the International Classification of Diseases, 10th revision (ICD-10) version of the Mini International Neuropsychiatric Interview (MINI) instrument in the Indonesian translation. The MINI instrument is a structured interview with 10 questions developed jointly by psychiatrists and physicians in the United States and Europe for evaluating psychiatric disorders in the Diagnostic and Statistical Manual of Mental Disorders IV and ICD-10 [19]. The symptoms of depression measured by this instrument included the subject’s condition during the last 2 weeks before participation in the survey. When used to diagnose depression in Indonesia, the MINI instrument has been reported to show sensitivity between 60% and 80%, positive predictive values ranging from 30% to 60%, and negative predictive values results around 90%; the agreement between the enumerators was found to be moderate, with a kappa value of 0.62 in diagnosing depression [20]. The MINI consists of 10 questions. Each “no” answer was scored as 0, and each “yes” answer was scored as 1. Respondents were categorized as having depression if there were at least 2 “yes” answers to questions 1-3 and at least 2 “yes” answers to questions 4-10 [19].
Independent Variables
The independent variables in this study included the demographic characteristics of the subjects and reproductive health factors. Demographic characteristics included family size, number of children younger than 5 years, age, educational level, occupational status, husband’s education, wealth index, and whether the participant lived with her husband/spouse. Reproductive health factors included age at first pregnancy, total parity, unwanted pregnancy, gestational age at birth, chronic energy deficiency, pregnancy complications, childbirth complications, postpartum complications, and contraceptive use.
Family size was coded as 0 for household size ≥4 people and 1 for ≤3 people. The number of toddlers was coded as 0 for families with 0 or 1 toddler and 1 for ≥2 toddlers. The age group of 20-24 years was coded as 0 and that of 15-19 years was coded as 1. For participants’ educational level, a code of 0 indicated having graduated from high school or more, and an education of less than high school was coded as 1. Each respondent’s occupational status was classified as working or not working. The wealth index was compiled from household ownership of goods divided into quintiles 1 (poorest) to 5 (richest). The variable of living with the spouse indicated whether the husband typically resided and slept with his wife. The variables of husband’s occupational status and education are shown only in the descriptive tables. Because some respondents did not live with their husbands, these variables were excluded from the multivariate analysis.
Age at first pregnancy was categorized into ≥19 years (code 0) or <19 years (code 1). Total parturition was defined as the mother’s number of live birth events, classified as only once or as twice or more. Pregnancies were classified as wanted or unwanted. Gestational age at birth was categorized as ≥9 months or <9 months. Chronic energy deficiency, pregnancy complications, childbirth complications, and postpartum complications were coded as 0 for “none” and 1 for “present.” Finally, contraception utilization was categorized as use or non-use. All variables with higher codes were interpreted as indicating a higher risk of PPD than those with lower codes. This study investigated the determinants of PPD in young urban and rural mothers.
Statistical Analysis
The data in this study were analyzed using a multiple logistic regression model with stratification based on the type of residential area (urban or rural). Initially, all variables were analyzed in a univariate model based on demographic and reproductive health characteristics (Table 1). Bivariate analysis with cross-tabulation and the chi-square test was performed to determine the relationship of each independent variable with PPD based on residential area (Table 2). The p-value of the chi-square test showed a significant relationship between each variable and PPD. Finally, all independent variables were included in the multivariate model to compare the determinants of PPD between urban participants and rural participants (Table 3). All independent explanatory variables were included in the logistic regression analysis. All independent variables were hypothesized to be associated with the dependent variable. The associations between PPD and all independent variables were analyzed using a multivariate logistic regression model, after which the adjusted odds ratio (OR) was calculated. The statistical significance threshold was set at a p-value of <0.05 (i.e., 5% alpha) [21]. The analysis was performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA), considering the applicable RISKESDAS weights, strata, and primary sample units following the RISKESDAS survey design, as previously reported [18].

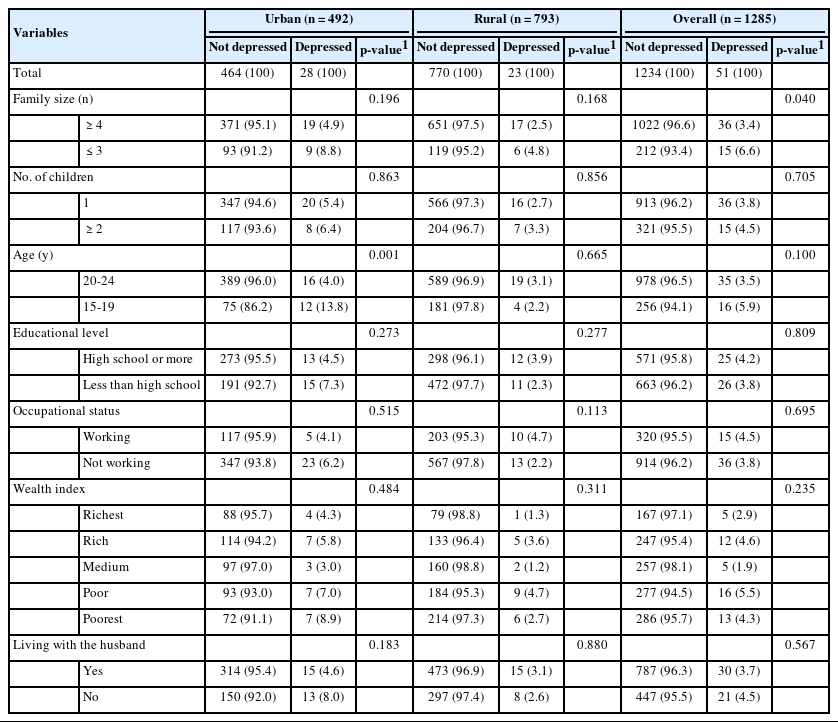
Frequency distribution of demographic characteristics of mothers aged 15-24 years by residence in urban and rural areas

Distribution of maternal reproductive factors of mothers aged 15-24 years by residence in urban and rural areas
Ethics Statement
This study used secondary data from the RISKESDAS 2018, which is available to the public. The identities of the respondents were not revealed or analyzed in this study. Ethical approval for RISKESDAS 2018 was obtained from the National Institute of Health Research and Development (NIHRD) Ethics Committee of the Indonesian Ministry of Health (No. LB.02.01/3/KE024/2018).
RESULTS
Sample Characteristics
Table 1 shows the sample characteristics of 1285 young mothers with babies aged ≤6 months (492 in urban and 793 in rural areas). Overall, 4.0% of mothers were depressed, with the proportion being higher in urban (5.7%) than in rural (2.9%) areas. Over 80% of mothers lived in large families, over 70% were 20-24 years old and not working, and 63.6% lived with their husbands. Table 2 shows the maternal reproductive factors of the mothers. Over 90% of the mothers had wanted pregnancies, and their babies had a gestational age at birth of >9 months. More than two-thirds of mothers had only 1 child. Almost one-third of the mothers were <19 years of age when pregnant for the first time.
The bivariate analysis shown in Table 3 indicates that in urban settings, the only demographic characteristic significantly related to depression in young mothers was the mother’s age. Conversely, there was no significant relationship between demographic factors and depression in participants living in rural settings. Overall, having 4 or more family members was significantly related to depression. Reproductive factors associated with PPD include unwanted pregnancy, gestational age at birth, pregnancy complications, and postpartum complications. However, gestational age at birth was not significantly associated with PPD in rural areas (Table 4).

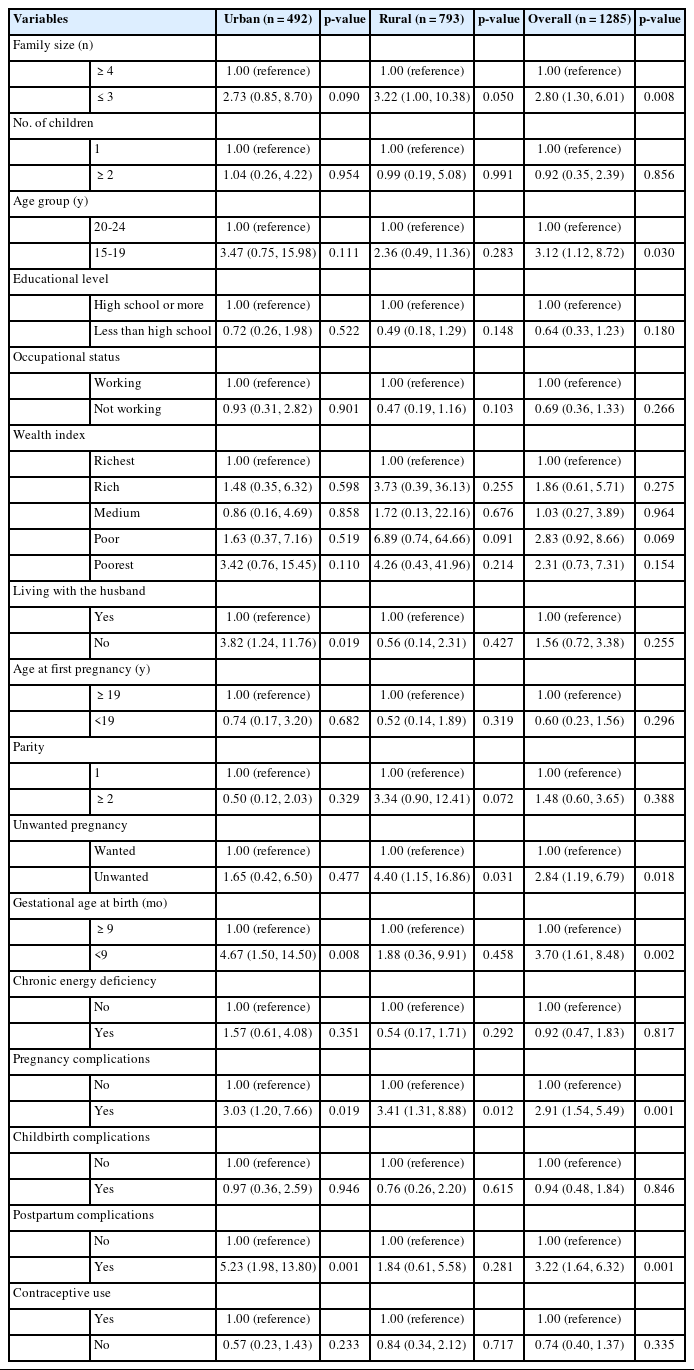
Frequency of respondents based on reproductive factors and depression status in urban and rural areas
Table 5 shows the determinants of PPD based on urban and rural strata. The overall results showed that the number of family members, maternal age, premature birth, unplanned pregnancy, pregnancy complications, and post-pregnancy complications were factors related to PPD in young mothers. However, different risk factors were identified in urban and rural areas, with only pregnancy complications appearing as risk factors for PPD in both areas. In urban areas, not living with a husband was associated with a higher risk of PPD, with an OR of 3.82 (95% CI, 1.24 to 11.76; p=0.019). Other factors carrying a higher risk of PPD for young urban mothers included premature birth (OR, 4.67; 95% CI, 1.50 to 14.50; p=0.008), pregnancy complications (OR, 3.03; 95% CI, 1.20 to 7.66; p=0.019), and postpartum complications (OR, 5.23; 95% CI, 1.98 to 13.80; p=0.001). In rural areas, a higher risk of PPD was associated with living in a smaller household (OR, 3.22; 95% CI, 1.00 to 10.38; p=0.050), having had an unplanned pregnancy (OR, 4.40; 95% CI, 1.15 to 16.86; p=0.031), and experiencing pregnancy complications (OR, 3.41; 95% CI, 1.31 to 8.88; p=0.012).
DISCUSSION
This study showed different patterns of PPD risk factors in young mothers from urban and rural areas. According to this study, 4.0% of young mothers with infants under 6 months experienced depression. The study also revealed that PPD is more common in urban areas (5.7%) than in rural areas (2.9%). Living without a husband, experiencing premature delivery, having complications during pregnancy, and having postpartum health issues were significant risk factors for PPD in urban areas. In rural areas, PPD was significantly associated with a larger household, unintended pregnancy, and pregnancy complications.
This result is comparable to an earlier study using RISKESDAS 2010 data, which found that 3.9% of young mothers aged 13-19 years were diagnosed with PPD [6]. A study of 399 first-time mothers aged 13 to 25 in the United States concluded that PPD scores, assessed on average at 4.24 months postpartum, were 9% of this sample scoring in the clinically significant range (score ≥12) [22]. A study in Australia on young mothers aged 16 years to 24 years indicated that 7.44% of the participants had PPD [23]. In addition, a recent systematic review analyzed PPD globally and found that Southeast Asia had a prevalence rate of 13.53% (95% CI, 11.00 to 16.52) [24]. The difference in prevalence could result from differences in participants’ ages, periods of assessment after delivery, instruments used, cut-off points, and other methodological issues. Notably, the PPD prevalence rate varied depending on the scale used. Studies in the United States and Australia used the Edinburgh Postnatal Depression Scale to measure postnatal depression [22]. The study in southeastern Asia was a meta-regression analysis using different instruments [24].
The study also showed that PPD was more prevalent in urban areas (5.7%) than in rural settings (2.9%). This finding is similar to that of a Canadian study, where PPD was more prevalent in urban settings than rural ones [25]. Comparative research on PPD in 2 groups of women in developing countries, such as Lebanon, revealed a greater prevalence of PPD among rural women (26%) than urban women (16%) [26]. In a systematic analysis, the prevalence of PPD was higher among rural women than among urban women, particularly in developing countries (21.5% among rural women in developed countries and 31.3% among rural women in developing countries) [27]. The higher prevalence of PPD in urban areas could be explained by the fact that rural residents are more likely than their urban counterparts to live near direct family members and to seek assistance and support from family and friends, rather than professionals [28]. In addition, people in rural communities report much higher levels of belonging than those in urban areas, which has also been found to protect against depression [29].
This study demonstrated a distinct pattern in PPD risk factors among young urban and rural mothers. The significant PPD risk factors in urban areas include living without a husband, preterm birth, pregnancy complications, and postpartum complications. Postpartum major depression in rural areas was significantly associated with a large household size, unintended pregnancy, and pregnancy complications. Social support is crucial in predicting PPD, especially in adolescent mothers, since PPD is explicitly linked to limited social support [30]. Adolescent mothers tend to experience more psychosocial difficulties than their adult counterparts [13]. In urban settings, living without a husband contributed significantly to PPD among young mothers. A previous study also found that relationship quality and partner support were predictors of PPD [31]. Another study showed that spousal support was associated with a reduced risk of PPD [32].
In several studies, preterm birth has been linked to increased postpartum depressive symptoms in women [1]. One study showed that preterm birth was a significant factor in urban settings. Mothers of preterm infants may face more stress due to helplessness, exclusion, alienation, a lack of understanding of parenting, and difficulties engaging with their children [33]. Moreover, a mixed-method study conducted on 27 women from southern France found that premature birth can be traumatic and lead to psychopathological symptoms [34]. This study showed a significant relationship between pregnancy and postpartum complications with PPD. Pregnancy complications were significantly related to PPD in women living in urban and rural settings. The occurrence of postpartum complications was a significant risk factor only in urban settings. A previous study in the Netherlands showed that PPD in women was predicted by various pregnancy and delivery complications [35]. A prospective study of 264 women in France found a significant risk of PPD to be associated with postpartum physical complications 2 months after delivery [36]. Unwanted pregnancies can affect the health of both women and their offspring. A meta-analysis of 65 454 participants showed that unintended pregnancy also increases the risk of developing PPD [37]. Unintended pregnancies might cause women to feel more psychosocially stressed because they may unexpectedly interfere with plans for schooling, careers, or other aspects of their lives [38].
Study Limitations
This study included a comprehensive range of risk factors for PPD. However, it was unable to account for other factors such as the mother’s illness, violence experienced by the mother, ongoing depression therapy, and drug usage. Our study data were derived from community data with stratified sampling, not from health facilities—usually accessed only by people aware of their symptoms—to represent the general population.
The prevalence of PPD among young mothers in Indonesia was 4.0%, with a higher prevalence in urban areas (5.7%) than in rural areas (2.9%). Social and reproductive factors were the factors associated with PPD in urban and rural areas, but different risk factors were identified in both areas with only pregnancy complications appearing as risk factors for PPD in both areas. Support from the family and the healthcare system is essential to young mothers’ mental health. The healthcare system needs to involve families to support the mental health of young mothers from pregnancy until postpartum.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Putri AS, Wurisastuti T, Suryaputri IY, Mubasyiroh R. Data curation: Putri AS, Wurisastuti T. Formal analysis: Wurisastuti T. Funding acquisition: None. Methodology: Wurisastuti T, Mubasyiroh R. Project administration: Putri AS. Visualization: Putri AS, Wurisastuti T. Writing – original draft: Putri AS, Wurisastuti T. Writing – review & editing: Suryaputri IY, Mubasyiroh R.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the Head of the Health Policy and Development Agency of the Ministry of Health of the Republic of Indonesia for providing the dataset and allowing us to analyze, represent, and publish the results.