Open Communication About Reproductive Health Is Associated With Comprehensive HIV Knowledge and a Non-stigmatising Attitude Among Indonesian Youth: A Cross-sectional Study
Article information
Abstract
Objectives
Human immunodeficiency virus (HIV) prevention among youth seems under-prioritised compared to other key populations. HIV knowledge and stigma are important parts of HIV prevention. To inform HIV prevention among youths, this study quantitatively analysed the associations between open communication regarding sexuality and sexual health, comprehensive HIV knowledge, and non-stigmatising attitudes in Indonesia.
Methods
This study used data from the Indonesian Demographic and Health Survey (IDHS) 2017. The analysis included unmarried men and women aged 15–25 years old. Comprehensive HIV knowledge and a stigmatising attitude were defined according to the IDHS 2017. Open communication about sexuality and sexual health was defined as the number of people with whom participants could openly discuss these topics in their direct network of friends, family, and service providers, with a scale ranging from 0 to a maximum of 7. Primary analysis used binomial logistic regression with weighting adjustments.
Results
The final analysis included 22 864 respondents. Twenty-two percent of youth had no one in their direct network with whom to openly discuss sexual matters, only 14.1% had comprehensive HIV knowledge, and 85.9% showed stigmatising attitudes. Youth mostly discussed sex with their friends (55.2%), and were less likely to discuss it with family members, showing a predominant pattern of peer-to-peer communication. Multivariate analysis showed that having a larger network for communication about sexuality and sexual health was associated with more HIV knowledge and less stigmatising attitudes.
Conclusions
Having more opportunities for open sex communication in one’s direct social network is associated with more HIV knowledge and less stigmatising attitudes.
INTRODUCTION
The human immunodeficiency virus (HIV) epidemic among youth is often overlooked compared to its effect on other specific populations, such as men who have sex with men (MSM) or female sex workers. This is true even though HIV prevalence and incidence remain high among youth. A 2021 report by the Joint United Nations Programme on HIV/AIDS (UNAIDS) showed that around 3.4 million youths aged 15 years to 24 years currently live with HIV, and that HIV prevalence in this age group has remained stable at around 0.3% worldwide since 2010 [1]. Similar findings were reported for Indonesia. The Indonesian Integrated Behavioural and Biomedical Survey (IBBS) from 2015 showed that the HIV prevalence among adolescents in 6 major cities reached 28.8% [2]. The overall epidemiological status of HIV among youth in Indonesia was also suggested by the low median age (27 years old) of people initiating antiretroviral therapy in Bali, Indonesia [3]. These figures were especially high among youth in key populations, such as MSM, where the rate could reach 29.8% [4].
One strategy to strengthen HIV prevention efforts is improving HIV-related knowledge among youth. There is ample evidence that higher HIV-related knowledge correlates with safer sex practices and other HIV preventive behaviours [5–7]. A good indicator of adequate HIV knowledge is the concept of comprehensive HIV knowledge. Comprehensive knowledge of HIV can be indicated by the ability to recognise HIV transmission methods, awareness of myths surrounding HIV, understanding of appropriate preventive measures, and a fact-based, non-stigmatising attitude toward people living with HIV (PLHIV) [8]. Unfortunately, comprehensive HIV knowledge among youth in Indonesia remains low. Data from the IBBS 2015 showed only 18.28% of adolescent respondents had comprehensive HIV knowledge. That rate was lower than that observed in 2011, when 22.63% of adolescent respondents showed comprehensive HIV knowledge [2].
A possible result of low comprehensive knowledge of HIV is high rates of stigmatisation and stigmatising attitudes toward PLHIV. The Indonesian Demographic and Health Survey (IDHS) from 2017 found over 80% of adults with a stigmatising attitude toward PLHIV [9]. A similar analysis of the IDHS 2012 focusing on adolescents found that over 70% had stigmatising attitudes. Furthermore, this analysis found that comprehensive knowledge could help prevent stigmatising attitudes [10]. There is also a theoretical framework supporting the role of stigma reduction policies in increasing HIV preventive behaviours and HIV testing among young people [11,12].
The relationships between HIV comprehensive knowledge, stigma, and preventive behaviour suggest the need to understand factors affecting HIV knowledge. Among these factors, communication about reproductive health in one’s social network plays an important role in HIV education [13,14]. Taboos surrounding the topics of sex, sexuality, and reproductive health have been known to be barriers to improved knowledge of HIV and other sexually transmitted infections in Indonesia and many other countries [15,16]. More open communication about sexual practices and health has also been found to reduce HIV stigma [17]. One way to increase open communication about sex and reproductive health is to avoid taboos by communicating about sexual education without directly mentioning it [16,18]. Another, more systematic approach is to develop a social structure that enables youth to discuss their sexuality openly [16,19].
The primary objective of this study was to use data from the IDHS 2017 to evaluate how the opportunity to discuss sex openly affected HIV knowledge among youths aged 15 years to 24 years old. Specifically, this study evaluated how having a personal social network available to discuss sex affected HIV knowledge acquisition among youth.
METHODS
Data Source and Population
This study used secondary data from the IDHS 2017, a large nation-wide survey that provided detailed data on the health of the Indonesian population with a special emphasis on fertility, family planning, and sexual health. IDHS datasets are publicly accessible. We accessed the dataset by registering through the DHS program website at https://dhsprogram.com/.
The IDHS 2017 used 2-stage stratified cluster random sampling. In the first stage of sampling, census blocks based on the 2010 Indonesian national census were used as sampling cluster units. Census blocks were systematically selected to be proportional to the regional population size, stratified based on urban or rural areas, and ordered by wealth index category. In the second stage of sampling, 25 households were systematically sampled from each census block for data collection [9]. For the purposes of this study, only unmarried men and women aged 15 years to 24 years old were included in the analysis. This is in line with UNAIDS definition of “young people” [1]. Individuals with missing data were excluded from the analysis.
Variables
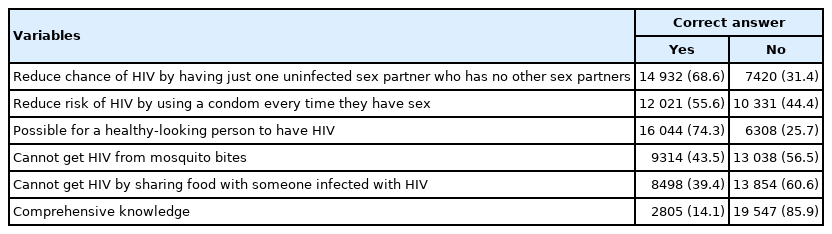
This study’s dependent variables were comprehensive knowledge about HIV and HIV stigmatising attitudes. Comprehensive knowledge followed the definition in the IDHS 2017, which included knowing that (1) always using a condom during sexual intercourse can prevent HIV transmission, (2) having only one HIV-free partner (who themselves does not have other sexual partners) can prevent HIV transmission, (3) seeing that a person looks healthy does not mean they are HIV-free, (4) sharing food with PLHIV does not transmit HIV, and (5) getting a mosquito bite does not transmit HIV. A respondent was defined as having comprehensive knowledge if they answered all of these items correctly [9].
HIV stigma also followed the definition provided by the IDHS 2017, which was based on 4 questions: (1) would not buy fresh food from vendors with HIV, (2) would not keep the HIV infection status of household member secret, (3) would be unwilling to care for relatives with PLHIV in the household, and (4) believes people with HIV should not be allowed to work/go to school. A respondent was defined as showing a stigmatising attitude if they answered yes to at least 1 of these questions [9].
This study’s primary independent variable was the openness to discuss sexuality and reproductive health in the respondents’ community. This variable was defined by the number of people in respondents’ lives with whom they discussed sexuality and sexual health. The IDHS 2017 asked whether respondents discussed matters of sexuality with the following people: mother, father, siblings, friends, religious figures, teachers, and healthcare providers [9]. Openness to discuss sexuality was scored by how many of these people each respondent could discuss sexuality with; the minimum score was 0 (none of them) and the maximum was 7 (all of them).
This study also included data on the socio-demographic characteristics of respondents, including gender, age, education levels, employment, and exposure to HIV-related information from the mass media. Education level was defined as the highest level of formal education that respondents had finished, and employment was defined as whether or not respondents were currently employed. Exposure to HIV-related information from mass media was defined as whether respondents had ever heard of HIV from print media, radio, or television. These parameters served as confounding variables, and were included in analysis because they have been observed to affect levels of comprehensive HIV knowledge [8,20].
Statistical Analysis
Univariate cross-tabulation analysis was conducted for categorical independent variables, while mean difference tests were conducted for continuous independent variables. Hypothesis testing was conducted with the chi-square and Mann-Whitney tests, respectively. Multivariate analysis was conducted using binomial logistic regression, including independent variables with p<0.05 in univariate analysis. The effect size was presented as the odds ratio with a 95% confidence interval (CI), disaggregated for the univariate crude odds ratio and the multivariate-adjusted odds ratio (aOR). Significance tests used the weighting provided in the IDHS 2017 datasets for more accurate generalisation of the data for the Indonesian population. All analyses were conducted using SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
Ethics Statement
This study utilised a publicly available, depersonalised, secondary dataset from the IDHS 2017 website. The use of such data is exempted from ethical review by the local ethical review body. The data collection process for the 2017 IDHS itself was reviewed and approved by ICF International’s Institutional Review Board and the Ministry of Health [21].
RESULTS
The final analysis included 22 352 respondents, with 10 307 (44.1%) women and 12 045 (55.9%) men. The age distribution was skewed toward younger groups, with a median age of 18 years old (interquartile range [IQR], 16–21). A slight majority of respondents (56.6%) lived in urban areas. Most respondents (82.1%) did not have a college degree, but only a slight majority of respondent was unemployed (57.3%). There were some gender differences in demographic characteristics despite the similar age distribution. Women respondents were more likely to live in urban areas (59.3%), have a college degree (24.1%), and be unemployed (66.0%) than their men counterparts (Table 1).
Many of the respondents (22.0%) had no one in their lives with whom they could discuss sexual matters. Similarly, only 25.5% have 1 people, and 22.6% had 2 people with whom to discuss sexual matters in their lives. Only 0.5% of respondents said they were able to discuss sexual matters with all the types of people asked about in the IDHS 2017 questionnaire (Table 1). Men had fewer people with whom they could openly discuss sex than women. Table 2 shows the distribution of openness to discuss sexual matters with the types of people asked about. Respondents were most open to discussing sexual matters with friends (56.1%), while they were least open to discussing them with their fathers (6.6%) and religious figures (8.7%).
Only 14.1% of respondents were categorised as having comprehensive HIV knowledge. Most respondents were able to correctly identify methods of preventing HIV transmission, such as regularly using a condom every time they have sex (55.6%), and having a single HIV-free sexual partner who themselves had no other partners (68.6%). Most respondents also knew that HIV infection can be asymptomatic, meaning that PLHIV can resemble a healthy person (74.3%). However, most respondents also still believed in HIV misconceptions such as the idea that HIV could be transmitted through mosquito bites (56.5%) and shared food (60.6%) (Table 3).
Table 4 shows that an overwhelming 85.9% of respondents answered “yes” to at least 1 stigma-related question, meaning that only a small proportion of adolescents and young people in Indonesia had a non-stigmatising attitude toward PLHIV. The most prevalent stigmatising attitude was refusal to buy produce from vendors with HIV (71.7%). Meanwhile, the least expressed stigmatising attitude was the unwillingness to care for a relative with HIV in one’s household (28.7%). These data show a difference in stigmatising attitudes based on social proximity, with less stigma toward familiar figures than toward strangers.
Univariate and multivariate analysis showed associations between openness to discuss sex with both comprehensive HIV knowledge and a stigmatising attitude among youths in Indonesia (Table 5). Univariate analysis showed that a higher likelihood of having comprehensive HIV knowledge was correlated with more open sex communication, defined as the number of people with whom respondents could openly discuss sex. This association persisted in the multivariate analysis, where respondents with 7 categories of people with whom they could talk about sex were much more likely to have comprehensive HIV knowledge than those who had none (aOR, 2.27; 95% CI, 1.29 to 3.98).

Results of univariate and multivariate logistic regression analyses for predictors of comprehensive human immunodeficiency virus (HIV) knowledge and stigmatising attitude among youths in Indonesia
A similar association was also found with the presence of a stigmatising attitude. Open sex communication (i.e., a higher number of people with whom respondents could discuss sex) was correlated with a lower likelihood of a stigmatising attitude. Even when controlling for comprehensive knowledge, the association between open sex communication and a lower likelihood of stigmatising attitude persisted, albeit with a more modest effect.
In addition, the data showed that all socio-demographic variables were associated with both comprehensive HIV knowledge and a stigmatising attitude. Higher education, older age, exposure to HIV in mass media, and living in an urban area were all associated with a higher likelihood of having comprehensive knowledge and a lower likelihood of showing a stigmatising attitude. Conversely, employed youths were less likely to have comprehensive HIV knowledge and more likely to show a stigmatising attitude toward PLHIV. Interesting differences were found regarding the role of gender. While no significant association between gender and the likelihood of comprehensive HIV knowledge was found, women did show a significantly higher likelihood of having a stigmatising attitude (aOR, 1.59; 95% CI, 1.41 to 1.79).
DISCUSSION
Our analysis showed that only 14.1% of youth in Indonesia had comprehensive knowledge of HIV, while a staggeringly high proportion (85.9%) have stigmatising attitudes. We also discovered limited ability to openly communicate about sex, as a full 22.0% of respondents had no one with whom they could discuss sexual matters. Multivariate analysis found that a higher level of open communication on sexual matters was associated with better HIV knowledge and a lower likelihood of having a stigmatising attitude, even after controlling for potential confounding factors.
It is concerning that our data show a drop in HIV knowledge compared to a previous large survey in Indonesia. The IBBS 2015 reported that 18.28% of Indonesian youths had comprehensive HIV knowledge, while the IBBS 2011 reported a rate of 22.63% [2]. This may indicate a continuing downward trend in HIV knowledge among Indonesian youth. The methodology of assessing HIV knowledge levels in this study is comparable with previous studies, which had similar definitions of comprehensive knowledge. Moreover, these findings (including the rate of 14.1% in the present study) show a considerably lower comprehensive level in Indonesia than in similar countries. Data from Myanmar and India, respectively, showed comprehensive HIV knowledge among youths at 16.2% and 53.21% [22,23]. Meanwhile, in Nigeria and Cameroon, only around 9% of youth had comprehensive HIV knowledge [24,25].
These results also confirmed a high level of stigma toward PLHIV among Indonesian youth, with 85.9% of Indonesian youth having stigmatising attitudes. This is in line with what was reported in the IDHS 2017 [9], as well as other Indonesian studies and surveys. The IBBS 2015, for example, found that although only 20–25% of youth outright said that they would ostracise known PLHIV, fewer than 5% stated that they would behave normally around PLHIV [2]. This finding is also comparable to other countries in Asia and Africa. An Indian study, for example, showed that around 70% of youths had stigmatising attitudes toward PLHIV [26], while a study conducted in the Democratic Republic of Congo and Nigeria found that around 90% of youth had stigmatising attitudes toward PLHIV [27].
The findings also identified a gender distinction in this cultural taboo. Young men seem more inhibited in discussing sex than young women. It has also been proposed that expectations around masculinity might drive young men to leave their education and enter the workforce earlier than women [28], a difference shown in these results as well. This masculine ideal may also keep men from talking about their sexuality and sexual health. Young men are less likely to engage in sexual health communication with their parents or at school [29,30]. Trust and lack of openness become barriers to sexual health communication within one’s family, while the focus on women’s sexual health in sex education at school can lead to disengagement by young men [30]. Our findings confirm these concerns, as young men had fewer people with whom they could discuss their sexuality and sexual health than young women.
The association between open sex communication, comprehensive HIV knowledge, and stigmatising attitude observed in our study can be explained within the framework of social network theory, together with the established observation of cultural taboo against open sex communication. It was postulated that knowledge acquisition, including on HIV, can be improved by widening one’s personal social networks discussing these topics [31,32]. The role of social networking in HIV knowledge acquisition can be inferred from the association between a larger network of people with whom one could discuss sex and higher HIV knowledge. Open discussion of sex-related topics may also reinforce awareness about HIV, which then reduces stigma [11].
These results also suggest the need to promote more open communication around sexuality and sexual health among youth. A starting point could be to optimise peer-to-peer communication about sexual health. In many cultures, sex communication among youth is limited to peers of the same gender and age group, while other youth only discuss sex in formal, sanitised settings such as classrooms or seminars [33]. Interventions aimed at increasing HIV knowledge among youth could co-opt the current taboo-influenced pattern of sex communication by focusing on peer-to-peer sex education or co-opting educational offerings. Peer-to-peer communication has been shown to be a particularly effective and acceptable mode of sex education [33,34]. To minimise opposition by parents to sexual education at school [35], these sessions could be organised as extracurricular activities. Moreover, Internet and social media could be utilised to provide safe spaces for peer-to-peer discussion regarding sexuality and sexual health. This method could be especially effective with the involvement of trained peer-supporters to guide the discussion and clarify misinformation [36].
More broadly, there is a need to address cultural taboos against open communication about sex and sexual health as a part of efforts to improve HIV knowledge. Low levels of discussion of sexuality within the family and with healthcare providers (Table 2) demonstrates this problem. Cultural taboos surrounding sex have been identified as barriers to effective education and promotion of HIV prevention [16,33]. Sex-related discussions in close social networks, such as family members, were deemed shameful or embarrassing [37]. The effectiveness of community-based and parental-based sex education programs was also found to be limited by the broader social norms and taboos surrounding sexual health communication [19,38]. More widespread non-stigmatising portrayals of sex discussions in the media, including both conventional and Internet-based mainstream media play an important role in diminishing taboos, as media still set the standard for publicly acceptable communication [29,33]. Popular culture products are especially powerful tools to reshape cultural taboos, including cultural taboos surrounding sexuality [39].
However, our results must be interpreted in the context of the limitations of this study. For example, its cross-sectional design may limit our interpretation of the causal relationship between open sex communication and HIV knowledge. Another weakness of this study is the limited variables available for analysis, as it was limited to those collected in the IDHS 2017.
In conclusion, our analysis of IDHS 2017 data for Indonesian youth discovered a low level of comprehensive HIV knowledge, a high level of stigmatising attitudes, and an associated limited openness to communicate about sex in the community. Cultural taboos against such communication may inhibit open communication about sexuality and sexual health. Open communication about sexuality and sexual health was found to be associated with a higher likelihood of comprehensive knowledge and lower levels of stigma. Specifically, having more people with whom one can discuss sex openly was associated with a higher likelihood of having comprehensive HIV knowledge and a lower likelihood of having stigmatising attitudes.
Data Availability
The IDHS 2017 datasets used in this study can be accessed through the DHS Program website at https://dhsprogram.com/data/dataset/Indonesia_Standard-DHS_2017.cfm?flag=0.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
ACKNOWLEDGEMENTS
None.
Notes
AUTHOR CONTRIBUTIONS
Conceptualization: Wirawan GBS, Januraga PP. Data curation: Wirawan GBSW, Gustina NLZ. Formal analysis: Wirawan GBS. Funding acquisition: None. Methodology: Wirawan GBS, Januraga PP. Writing - original draft: Wirawan GBS. Writing - review & editing: Januraga PP, Gustina NLZ.