Challenges to Achieving Universal Health Coverage Throughout the World: A Systematic Review
Article information
Abstract
Objectives
No systematic review has explored the challenges related to worldwide universal health coverage (UHC). This study reviewed challenges on the road to UHC.
Methods
A systematic electronic search of all studies that identified the challenges of worldwide UHC was conducted, without any restrictions related to the publication date or language. A hand search and a bibliographic search were also conducted to identify which texts to include in this study. These sources and citations yielded a total of 2500 articles, only 26 of which met the inclusion criteria. Relevant data from these papers were extracted, summarized, grouped, and reported in tables.
Results
Of the 26 included studies, 7 (27%) were reviews, 6 (23%) were reports, and 13 (50%) had another type of study design. The publication dates of the included studies ranged from 2011 to 2020. Nine studies (35%) were published in 2019. Using the World Health Organization conceptual model, data on all of the challenges related to UHC in terms of the 4 functions of health systems (stewardship, creating resource, financing, and delivering services) were extracted from the included studies and reported.
Conclusions
This study provides a straightforward summary of previous studies that explored the challenges related to UHC and conducted an in-depth analysis of viable solutions.
INTRODUCTION
In recent years, there has been an increased push for universal health coverage (UHC) at the global level. UHC is defined by the World Health Organization (WHO) as “ensuring that all people obtain the health services they need, of good quality, without suffering financial hardship when paying for them” [1]. This concept was initially created in 1883 after Germany introduced public health coverage to ensure the health status of its young population. Later, after many countries also began to offer national health insurance, the World Health Assembly adopted the term “UHC” starting in 2005, and in 2010, the World Health Report focused on financing health systems so countries could build platforms for UHC [2].
The relationship between catastrophic health expenses and extreme poverty has led to an increased focus on UHC, not only as a way to improve healthcare utilization but also to eliminate extreme poverty by protecting individuals and families from catastrophic health expenditures. Financial risk protection measures can prevent patients and their families from slipping into poverty when paying for health services out of pocket. Thus, UHC provides an avenue for uniting global health, fighting against poverty, and reducing social inequity and is a hallmark of a government’s commitment to improving the well-being of all of its citizens [3,4].
Movement toward UHC is a long-term policy engagement that requires both political know-how and technical knowledge. Countries need political leaders with commitment and vision who are ready to invest in an administrative capacity, develop solid institutional foundations, and offer responsive governance. Technical solutions must be accompanied by pragmatic and innovative strategies that address the national political and economic context [5]. Evidence has shown that progress toward UHC needs not only strong political commitment, but also a coherent strategy to ensure that the different aspects of health systems are aligned and coordinated with each other in order to effectively address core performance challenges. The 4 main functions of health systems include financing, stewardship, creating resource, and delivering services, and a coherent and well-aligned strategy for health financing reform plays a key role when addressing challenges related to UHC [6,7].
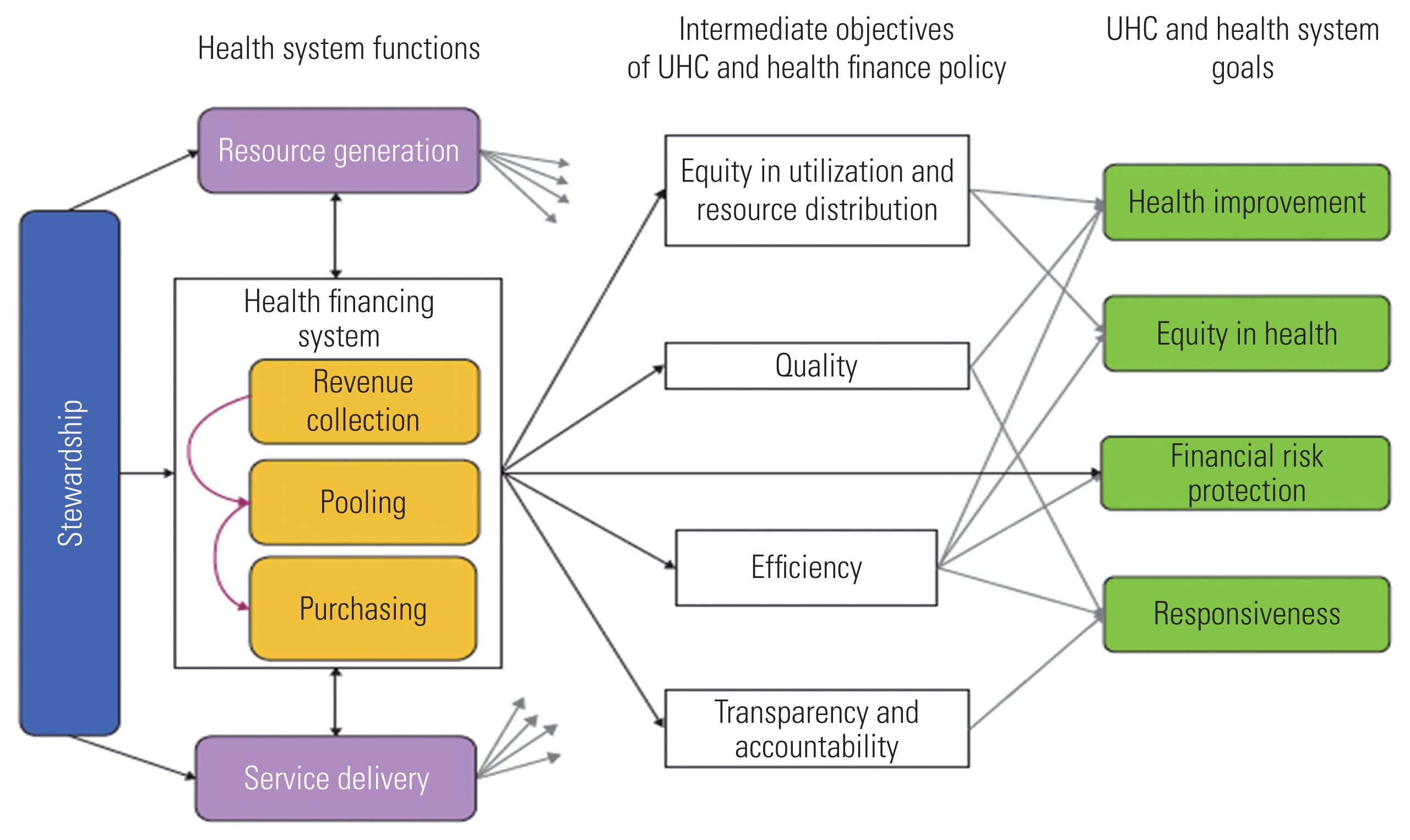
WHO’s thinking on the development of health financing strategies is rooted in its approach to health financing policy, as illustrated in Figure 1 [8]. This figure outlines the links between health financing arrangements and UHC goals as well as intermediate objectives that have plausible links to these goals [9]. This approach combines a normative set of goals that are embedded in the concept of UHC (equity in utilization or service use relative to need, financial protection, and quality) with a descriptive framework of the functions and policies that play a part in all health financing arrangements.
Countries must meet a set of prerequisites in order to achieve UHC, including stakeholder support and a political commitment to funding predominantly from the public sector. The WHO has also proposed 4 essential attributes needed to achieve UHC, which include an efficient and well-run health system, an affordable and equitable system for financing, access to essential medicines and technologies, and a sufficiently trained and motivated health workforce [10]. The common challenges faced by countries when moving toward UHC are coming into sharper focus, and early research [11,12] has begun to identify the most and least effective approaches for addressing these challenges. The solutions to these challenges will likely be highly context-dependent, inherently path-dependent, and shaped by the political leadership and administrative capabilities [13]. However, it remains worthwhile to systematically review all the challenges that could hinder the achievement of UHC based on the current available body of original literature.
In this study, we attempted to gather and review all the available evidence on barriers and challenges to achieving UHC in all countries with available data. Due to the lack of updated nationwide studies, the results of the current systematic review have the potential to be of considerable merit and applicability for policymakers and interested researchers. Understanding the current challenges on the road to achieving UHC is indispensable for society’s development and also is key to eliminating extreme poverty, which can be caused by catastrophic health expenses. In addition, UHC is multidimensional and encompasses legal, political, health, and socioeconomic systems and agendas. Therefore, it is critically important to examine challenges related to UHC from many different angles.
METHODS
Criteria for Considering Studies for This Review
All types of studies and documents that aimed to identify challenges and barriers to UHC in any part of the world were considered for inclusion in this study. We used the WHO definition of UHC [14], which defines UHC as follows: “Universal health coverage means that all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship.” No limitations with regard to publication date or language were applied when searching for studies.
Search Strategy
To identify studies based on this review’s inclusion criteria, an electronic literature search was first conducted of PubMed, Scopus, Web of Science, and the Cochrane Library databases. For all of the databases, any synonyms to the word “challenge,” including obstacle* OR barrier* OR challenge*, were searched followed by the search term “universal health coverage.” For example, in PubMed, the search terms were as follows: (((obstacle*[Title/Abstract]) OR barrier*[Title/Abstract]) OR challenge*[Title/Abstract]) AND “universal health coverage” [Title/Abstract]). The bibliographies of the included studies were also searched. We scanned the reference lists of all of the included papers to identify the main contributing authors on this topic. Another search was then conducted using the names of the identified authors to ensure that the most relevant studies were included in the review. Similarly, a hand search was conducted to identify relevant journals, the gray literature, government documentation, informal reports, and other related materials. All identified studies were entered into EndNote X7 for further investigation of their relevance to the topic.
Study Selection
The process of article identification and paper selection is shown in Figure 2. As a result of the electronic search, 2500 papers were initially identified, and 1 paper was identified through the hand search. All duplicate papers (n=1428) were removed, and 1073 papers remained. The titles and abstracts of the remaining articles were then independently screened by 2 reviewers, and any studies not related to the research objectives were excluded. A total of 72 papers remained, and the full texts were assessed for eligibility, after which 46 articles were excluded, including 42 that were not relevant to the research objectives, 2 that were written in languages than English, 1 that was a book, and 1 for which the full text was unavailable. A total of 26 studies met the inclusion criteria for this review study and were subsequently included in our analysis. A summary of the included studies is available in Supplemental Material 1.
Data Extraction and Analysis Strategy
Data on the collected studies, including information on the descriptive characteristics of studies and the studies’ methods, such as the study design, sample size, main findings, and the relevant challenges related to UHC, were extracted using a purposefully designed data extraction form. The data are summarized in Supplemental Material 1. In addition, since health system functions can impact goals and objectives related to UHC, we divided challenges related to UHC into 4 categories based on the functions of health systems, which include stewardship, creating resource, financing (which itself includes revenue collection, pooling, and purchasing), and delivering services (Figure 1) [8]. Dividing the challenges of UHC by these 4 functions of health systems was based on discussion and agreement between the authors of this review study; hence, we tried to categorize each challenge according to the most relevant functions. For example, efficiency improvements can promote financial protection and equitable utilization of health services. Efficiency refers to the creation of as many high-quality health services as possible given the available resources. Even though this suggests that resources should not be wasted, health systems should still pursue the lowest cost combinations of service inputs (such as health workers, drugs, and other factors) to provide effective and high-quality service. This also suggests that services should be provided at the lowest possible level of the health system. For example, if a patient can be effectively treated at the primary care level, they should not be treated at a central hospital [9]. The data extraction process was undertaken by 2 reviewers independently, and discrepancies were addressed and resolved through discussion as needed.
Ethics Statement
This study is a systematic review and does not deal with human participants.
RESULTS
Description of the Included Studies
As shown in Supplemental Material 1, among the 26 included studies, 7 (27%) were reviews, 6 (23%) were reports, and 13 (50%) had another type of study design. The publication dates of the included studies ranged from 2011 to 2020, and 9 studies (35%) had a publication date in 2019.
Universal Health Coverage Challenges Related to Stewardship
The main challenges related to UHC concerning stewardship are the lack of inter-sectoral coordination and gaps in managerial, administrative, and supervisory capacity from the executive level down to the facility level in countries’ ministries of health. These include gaps in fundamental business practices (human resources, finance, and procurement). In addition, other challenges, shown in Figure 3, include an absence of managerial feedback loops, in part due to limited supervision and empowerment at healthcare facilities [15–25]; public health challenges such as demographic shifts, epidemiological changes, low equity, and low gross domestic product [15,19,23,26,27]; the liberalization of global trade and the corresponding increased burden of disease resulting in a higher demand for healthcare services [28]; the absence of integrated clinical and frontline health worker data and suboptimal health information systems, as well as the limited use of existing data [21,23,29]; the need to design benefit packages and prioritize certain health needs across 3 dimensions, which include coverage population, service, and cost [13,26]; inefficiencies in the management of insurance schemes [4,17]; insufficient government finances [5,18]; a lack of support from key stakeholders [4], and low trust in public healthcare facilities [21].
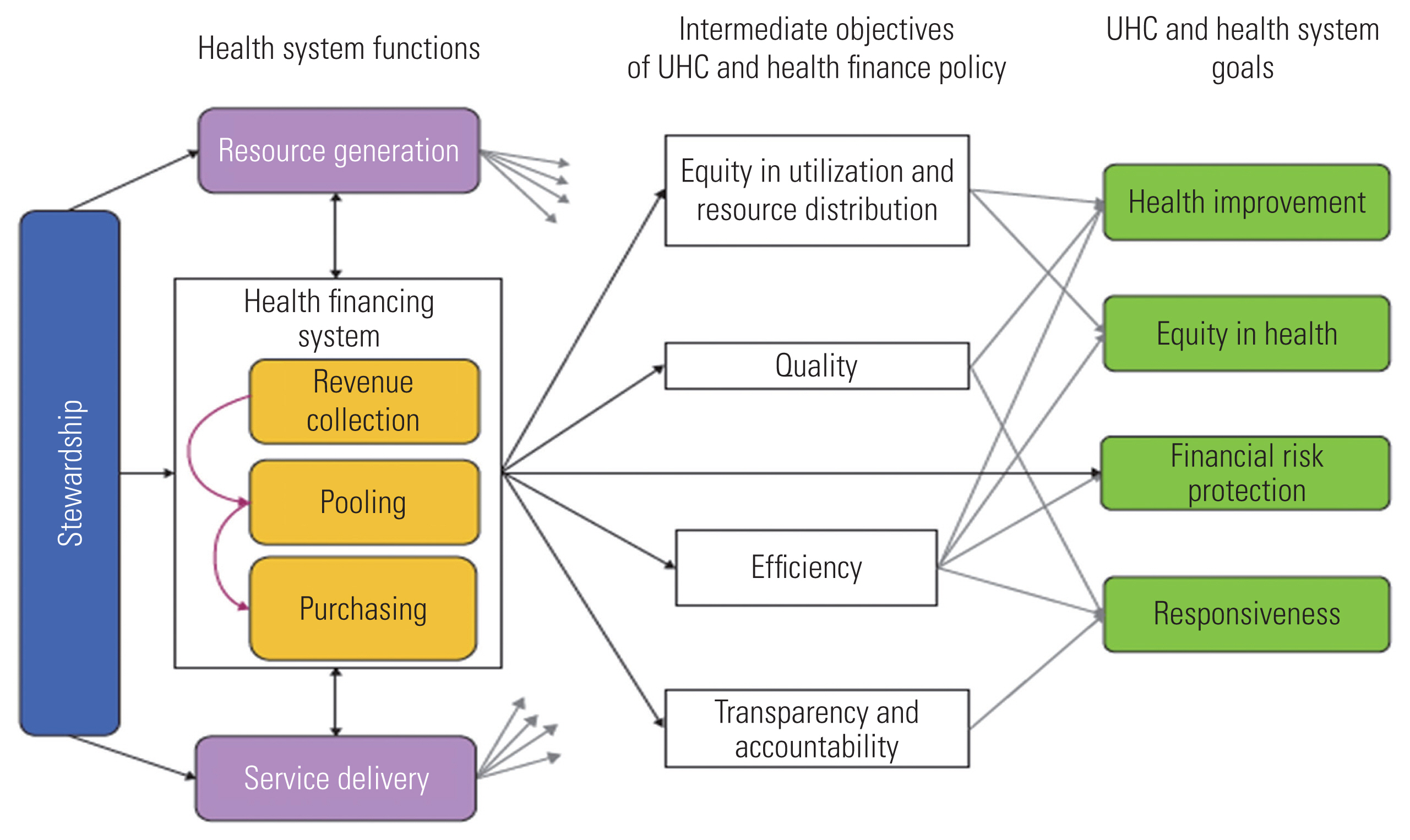
Universal Health Coverage Challenges Related to Creating Resource
The main challenges related to UHC concerning creating resource are inadequate human resources and health workers [1,3,5,18–21,23,25]; challenges related to the production, performance, and distribution of health workers [5,25]; inadequate medical facilities for public hospitals and community health centers [25,29]; inadequate health infrastructure [4,20]; a shortage of technology, equipment, and materials [20]; inequity in the allocation of public health resources (both financial and human) [30]; and “supply-side readiness,” which refers to the availability and quality of services [13]. Figure 4 summarizes these challenges.
Universal Health Coverage Challenges Related to Financing
The financing function includes 3 sub-domains, and the challenges of each of these sub-domains are listed in this section. The main challenges related to revenue collection, which is the first sub-domain, are inadequate financial resources [3,18,19,25,31,32], financial sustainability [22,29], poor funding for primary healthcare systems [4], fragmentation of financing arrangements [21,30,33], and mismatches between the allocation of subsidies, disability severity, and socioeconomic status [32].
The main challenges of pooling, the second sub-category, are the lack of health insurance coverage for people and services [4,5,27,29,32], existing systems of voluntary health insurance [28], fragmentation of the pool of health insurance funds [4,27,34], the lack of financial support or protection [1,5,17,23, 30,32,35], the high proportion of out-of-pocket spending [30, 31,35], a large proportion of people who live in extreme poverty who are unable to pay premiums [4,32], the high cost of transportation to reach healthcare facilities for people with disabilities, and disproportionate copayments for physical therapy, laboratory tests, and some medicines [32].
The main challenges of the third sub-category, purchasing, are confusion about the conditions needed to receive reimbursement for health expenses [32]; the small share of resources allocated to low-level health facilities and community-based services [16,25]; the complex interplay between inadequate allocation, unequal distribution, and inefficient utilization of funds allocated to public health measures [33,35]; low investment in health and primary healthcare [21]; cost control [18]; and the unequal allocation of financial resources for public health [23,30].
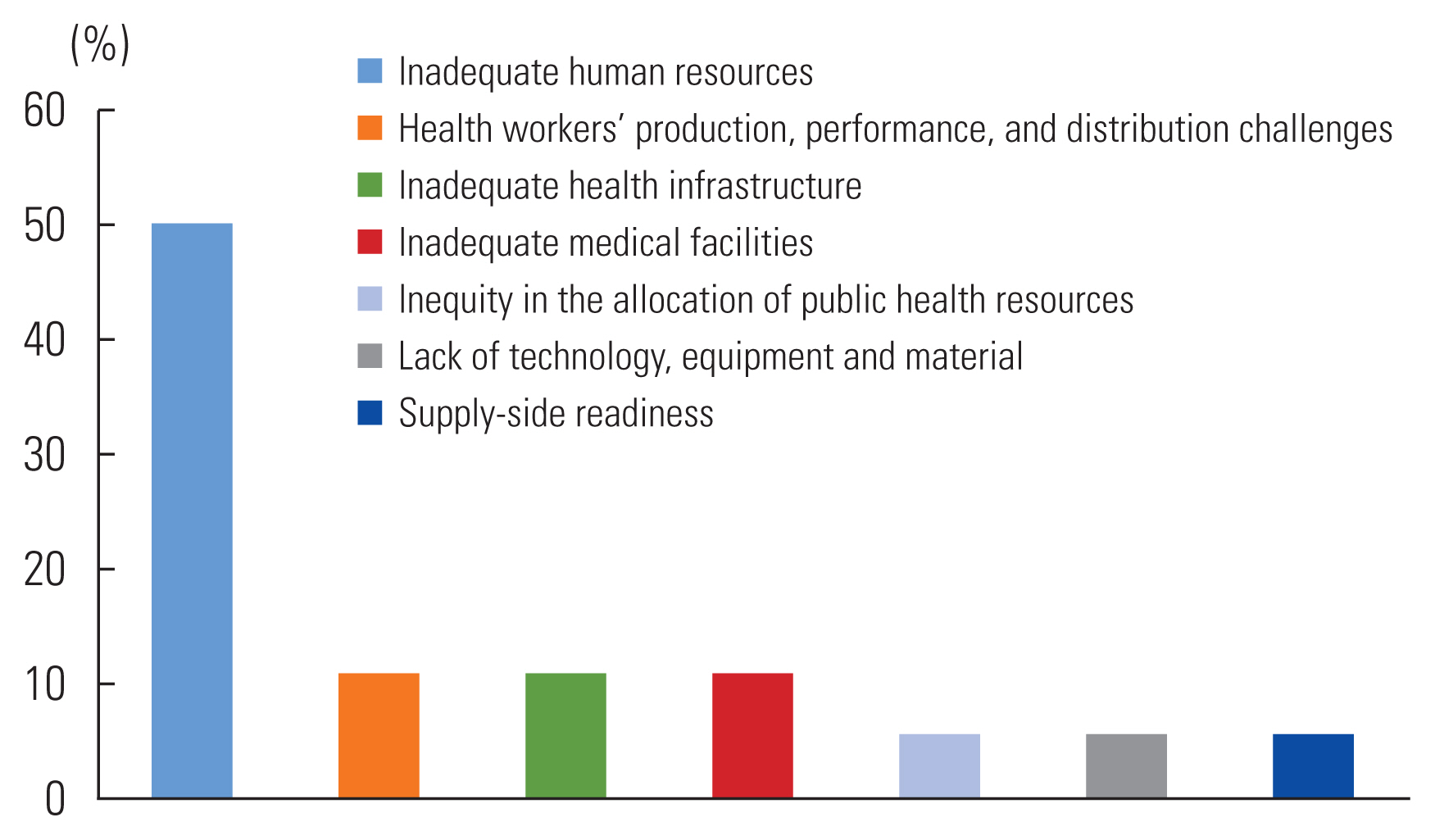
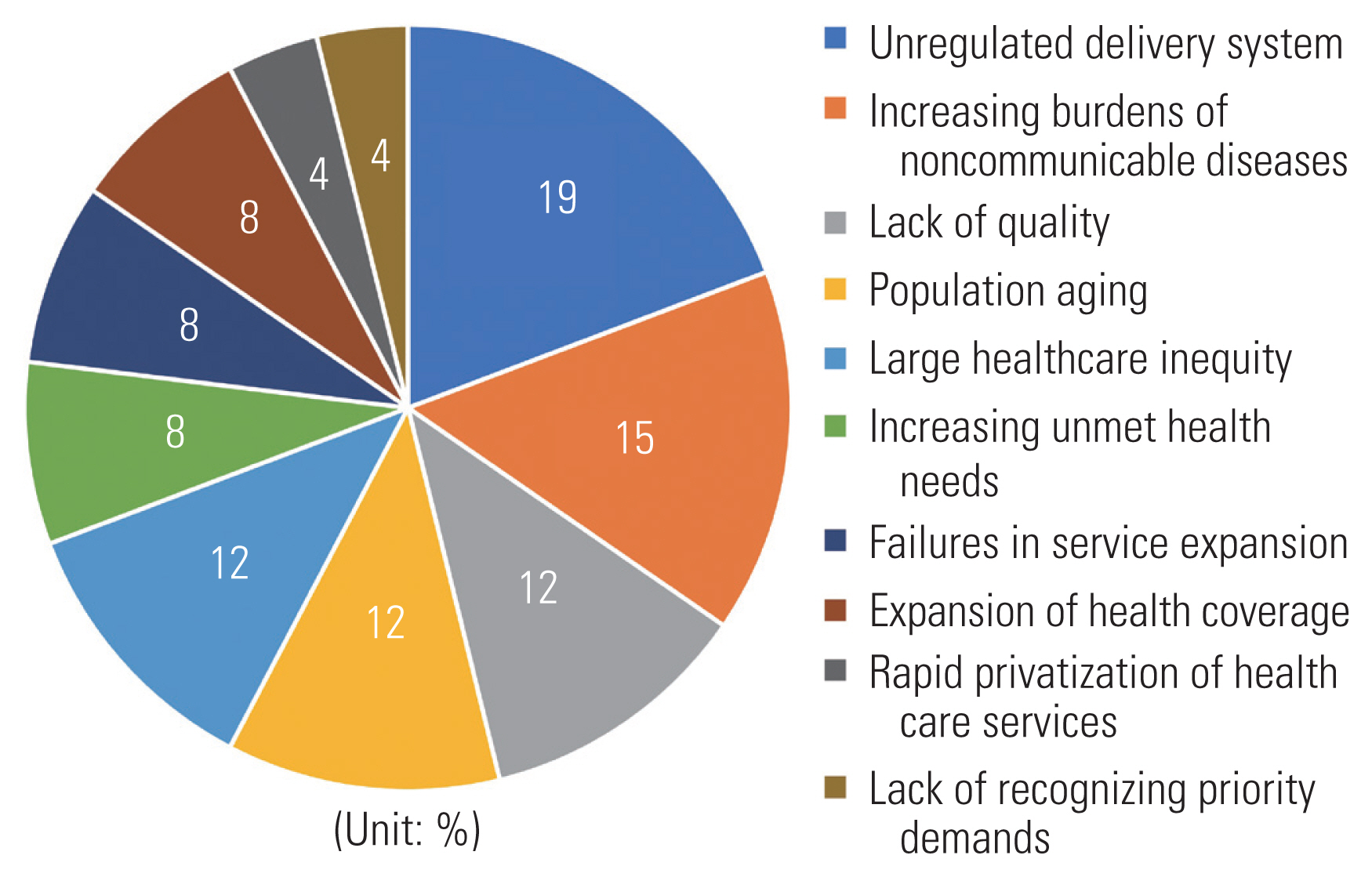
Universal Health Coverage Challenges Related to delivering services
The main challenges related to UHC concerning delivering services, as shown in Figure 5, are unregulated and fragmented healthcare delivery systems [16,19,22,23,25]; inadequate care and services in terms of quality [1,29,33]; the aging of the population, which increases the risk of geriatric health issues [23,27,35]; the increasing burden of non-communicable diseases, persisting infectious diseases, and the reemergence of infectious diseases with pandemic potential [3,19,23,25]; increasing unmet health needs [15,24]; the rapid privatization of healthcare services leading to increased treatment costs [35]; failures to expand and strengthen services [20,25]; incorrect diagnosis of the highest-priority demands [20]; the expansion of health coverage in formal and informal sectors [5,13]; and significant healthcare inequity [17,23,25].
Suggestions to Improve Universal Health Coverage or Overcome Barriers to Universal Health Coverage
The following suggestions were proposed by the authors of the original studies included in this review for improving UHC or overcoming barriers to UHC:
Sufficient revenue should be raised for health system financing, and the efficiency of revenue utilization should be improved. Coverage for the very poor should be provided, and the proportion of the population that is underinsured should be reduced. Access to quality healthcare in rural areas should also be improved [4,31,32].
Policymakers must develop and adopt national health financing systems to provide financial risk protection [5,29–31,35].
Government stewardship, stakeholder support, and fair contribution and distribution of resources by appropriate health financing modalities should be undertaken [28,30,31].
General revenues should be used to fully cover the informal sector, or a combination of tax subsidies, non-financial incentives, and contributory requirements should be devised and implemented [13,31].
An integrated dynamic UHC system that is adaptable to a rapidly developing society should be developed to provide an affordable and sustainable path toward healthcare for all [1,29,30].
Movement toward UHC should be established as a long-term policy engagement requiring both technical knowledge and political know-how [5,27].
UHC schemes should be designed to cover the entirety of a country’s population, including those in poverty in addition to those with higher income levels using special strategies [1,28].
The role of strategic purchasing when working with powerful private sector entities, the effects of federal structures, and the implications of investment in primary healthcare as a foundation for UHC should be explored [18,27].
DISCUSSION
This systematic review focused on the challenges that exist on the road toward worldwide UHC. Due to the diversity of the included studies in terms of their main objectives, designs, publication dates, and other decisive factors, the identified challenges cannot be generalized to all countries throughout the world. However, these challenges can be observed anywhere in the world with differing degrees of severity depending on the context.
Based on the identified studies, we can conclude that the lack of administrative coordination related to stewardship, insufficient human resources related to creating resource, a lack of financial support related to financing, and unregulated and fragmented healthcare delivery systems related to delivering services were the most common challenges on the road toward worldwide UHC. However, the 3 most frequently mentioned challenges were inconsistencies within the structures of the health ministries and their related facilities, insufficient human resources, and a lack of financial support.
When categorizing challenges by the 4 functions of health systems, some of the challenges were difficult to classify according to 1 function since some of them were related to multiple functions. We categorized these challenges based on the most relevant function. For example, inadequate medical facilities, which we classified as a creating resource challenge, can be considered a financing challenge since the reason behind inadequate medical facilities is often a lack of sufficient financial resources to invest in such facilities. Similarly, a lack of health insurance coverage for people and services, which we classified as a financing challenge, can also be considered a stewardship challenge since a possible reason for a lack of health insurance coverage may be upstream policies related to stewardship.
Since most of the fundamental challenges related to UHC can be linked to a weak political commitment and a lack of policy advocacy, we can conclude that major policy alterations must be made. In addition, badly designed policies should be revised to improve health coverage.
To achieve UHC, specific programs to train human capital should be developed and expanded alongside the allocation of more financial resources. The support of stakeholders must also be considered, and the distribution of human and financial resources must be revisited. As of the time of this study, due to the coronavirus disease 2019 pandemic, many countries are struggling with poor economic sustainability. Policymakers should take initiative to enact stronger healthcare measures, and leaders should make serious efforts to implement their solutions.
The results of this study could help health stakeholders and decision-makers identify the challenges most relevant to their countries and devise plans for achieving UHC by addressing these challenges. Achieving UHC is not limited to high-income and developed countries, and low-income, middle-income, and developing countries can also take effective steps to address challenges related to UHC and improve the status of health coverage across their populations. However, the countries that made the most successful efforts toward UHC have benefited from their governments’ political and financial commitments and private sector assistance. Comprehensive governmental support and tax financing have been the most successful strategies for governments concerning the health sector [33,34]. Recognition of a country’s health needs and the implementation of measures to expand and strengthen the health system, particularly measures concerning prevention and public health, have been among the most consequential strategies undertaken by countries that successfully achieved UHC. In addition, the development of coordinated referral systems has also helped to improve health coverage leading to UHC [5,14].
The pathway to UHC specifically depends on a country’s history, available resources, expectations, and political economy [23]. No country has enough resources to meet all of the health needs of all of its citizens, and trade-offs must always be made. When countries develop road maps for achieving UHC, they must prioritize investments to address their populations’ health needs given their limited resources, institutional capacities, burdens of disease, and levels of community engagement, among other factors. It is important to understand challenges, issues, and options in order to engage in evidence-based planning and decision-making.
CONCLUSION
This study provides a straightforward summary of previous studies that explored the challenges related to UHC and conducted an in-depth analysis of viable solutions. Based on the challenges identified in this study, policymakers should take active steps to consider viable solutions to overcome these challenges. Demographic and structural foundations of countries must also be taken into account when devising solutions to these challenges.
SUPPLEMENTAL MATERIALS
Supplemental material is available at https://doi.org/10.3961/jpmph.21.542.
Summary of characteristics and findings of the included studies on the challenges of universal health coverage
ACKNOWLEDGEMENTS
None.
Notes
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Tajvar M, Darrudi A. Data curation: Tajvar M, Darrudi A, Ketabchi Khoonsari MH. Formal analysis: Tajvar M, Darrudi A. Funding acquisition: None. Methodology: Tajvar M, Darrudi A. Project administration: Tajvar M, Darrudi A. Visualization: Tajvar M, Darrudi A. Writing – original draft: Tajvar M, Darrudi A, Ketabchi Khoonsari MH. Writing – review & editing: Tajvar M, Darrudi A, Ketabchi Khoonsari MH.