How Much Do Older Adults Living Alone in Rural South Korea Know About Dementia?
Article information
Abstract
Objectives
This study aimed to examine the level of dementia knowledge of older Korean adults living alone in rural areas and to identify related factors.
Methods
A cross-sectional descriptive design was applied. The participants were 231 older adults living alone who were recruited from 12 of the 13 primary health care posts in the rural area of Chuncheon. Participants’ level of dementia knowledge was assessed using the Dementia Knowledge Scale. Data were analyzed using descriptive statistics, and the t-test, analysis of variance, chi-square test, and Mann-Whitney test were applied.
Results
Participants’ mean age was 77.3±5.4 years, and women comprised 79.7% of the sample. Over half of the participants (61.9%) had no formal education, and all the participants were enrolled in Medical Aid. The participants’ average percentage of correct answers was 61.6%. The highest rate (94.4%) was for the item “Dementia can change one’s personal character.” The item with the lowest proportion of correct answers was “Dementia is not treatable” (23.4%). Dementia knowledge was significantly associated with age, education, health coverage, source of living expenses, and dementia risk.
Conclusions
Dementia knowledge among Korean rural older adults living alone was relatively low. Participants’ misconceptions about symptoms and treatment could hinder them from seeking early treatment. The results of this study suggest the need for active outreach and health care delivery for rural older adults living alone in South Korea.
INTRODUCTION
Dementia has emerged as one of the most important health challenges throughout the world [1], and South Korea (hereafter Korea) is no exception. In Korea, 9.2% of people aged 65 and over were estimated to have dementia in 2012 [2], and the prevalence is expected to increase to 15.6% by 2050 [2]. The prevalence of mild cognitive impairment, a risk factor of dementia [3], among adults aged 65 and over was estimated to be 27.5% in 2012 [2], and there were more people in this age group with mild cognitive impairment in rural areas (30.7%) than in urban areas (20.5%) [2]. In addition, the economic costs of dementia have enormously increased in Korea. Suh et al. [4] estimated its total annual cost to be over USD 2.4 billion in 2002, and a recent study [5] forecast that the annual cost of dementia would reach a total of USD 37.5 billion by 2050.
Dementia should receive more attention as a health issue for older adults in the rural areas of Korea, especially for those living alone. First, the proportion of individuals over 65 of age has increased more rapidly in rural areas than in urban areas. While the proportion of people aged 65 and over in urban areas increased from 5.5% in 2000 to 9.2% in 2010, the proportion of those living in rural areas rose from 14.7 to 20.7% over the same period [6]. Second, rural older adults are in poorer health and have more difficulties accessing health care than their urban counterparts. For example, the self-rated health of rural older adults was found to be poorer than that of their urban counterparts [7], and rural older adults were less physically active than their urban counterparts [7,8]. These are risk factors for dementia [9-13]. In addition, older adults in rural areas have been found to use fewer health care than those in urban areas due to the concentration of health care resources in urban areas [7]. There is a misconception that dementia is part of the normal aging process [14], and as a result, rural older adults may have difficulty accessing treatment for early-stage dementia. Moreover, more older adults live alone in rural areas (33.5%) than in urban areas (22.7%) [6]. Older adults living alone tend to experience faster cognitive decline than those living with others, including family members, due to a monotonous life pattern and lack of environmental stimulation [15-18].
Currently, early detection, intervention, and risk reduction are known as the best ways to lower the dementia burden [19]. Therefore, individuals need to be informed about the progress and management of dementia, because older adults with such knowledge can be actively engaged in preventive behaviors [20]. However, little evidence exists about how much older adults living alone in rural areas, an especially vulnerable group, know about dementia. Therefore, this study aimed to examine the level of dementia knowledge of older Korean adults living alone in rural areas and to identify related factors.
METHODS
Participants and Procedures
After obtaining institutional review board approval, participants were recruited from 12 of the 13 primary health care posts in the rural area of the city of Chuncheon. The study’s purpose and process were announced at the primary health care posts. Of 393 registered older adults living alone, 231 agreed to participate in this study (response rate, 58.8%). Written consent was obtained, and small incentives, such as snacks and beverages, were given. Data were collected by 12 community health practitioners who were trained to assess older residents. Data were gathered during January 2014.
Measures
Information on study participants’ characteristics—gender, age, educational level, type of health coverage, source of living expenses, number of chronic diseases, self-rated health, and alcohol consumption—was collected using a questionnaire. Regarding types of health coverage, Medical Aid is a public assistance program that enables the poor to have access to health care at little or no charge. Type 1 Medical Aid beneficiaries are generally poorer than their type 2 counterparts.
Participants’ level of dementia knowledge was assessed by the Dementia Knowledge Scale (DKS), which was developed by the research team of the Nationwide Prevalence Study of Dementia in Korean elders [2]. It is a 15-item questionnaire with yes/no responses. Its items are composed of questions about causes (items 1, 2, 4, 5, 7), prevalence and the health system (items 3, 6, 15), symptoms and diagnosis (items 8-11), and prevention and treatment (items 12-14) of dementia. Scores reflect the number of items answered correctly. A higher score indicates a higher level of dementia knowledge.
Level of cognitive function was assessed by the Korean version of the Mini-Mental State Examination for Dementia Screening (MMSE-DS) [21,22], a culturally modified MMSE developed by Folstein et al. [23]. It has been widely used in primary health care in Korea [2,21,24]. An MMSE-DS score of 23 or lower suggests mild cognitive decline, and it is also used to identify people at-risk for dementia by considering gender, age, and education [21,22].
Data Analysis
SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used to analyze the data. Descriptive statistics were used to show the basic characteristics of participants and levels of dementia knowledge by gender. The t-test, analysis of variance, chi-square test, and Mann-Whitney test were applied to identify differences in dementia knowledge by participants’ characteristics and dementia risk. The outcome measure was the DKS score. A statistical significance level of p<0.05 for 2-sided tests was used.
Ethics Approval
The study protocol was approved by the institutional review board of Hallym University (HR-2013-61).
RESULTS
Participants’ Characteristics
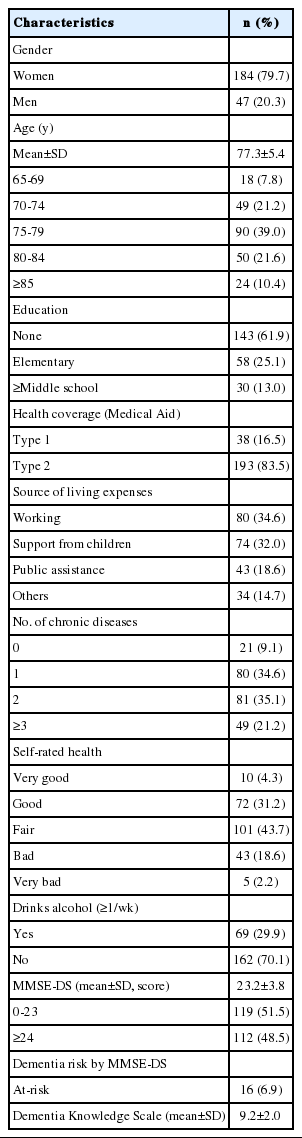
Participants’ characteristics are presented in Table 1. Their mean age was 77.3±5.4 years, and women comprised 79.7% of the participants. Over half of them (61.9%) had no formal education, and all the participants were enrolled in Medical Aid. Over one-third of the participants (34.6%) lived on income from their work, followed by financial support from their children (32.0%) and public assistance (18.6%). Only 9.1% of the study participants were free from chronic illness, while 21.2% of them suffered from more than 3 chronic diseases. Those who rated their health status as bad or very bad comprised 20.8% of the participants. Roughly one-third of the participants drank alcohol more than once a week. The mean score on the MMSE-DS was 23.2±3.8, and those who scored 23 or lower comprised 51.5% of the sample. The high-risk group was identified based on gender, age, and education, as well as the MMSE-DS score, and 6.9% of the participants were deemed to be at-risk for dementia, requiring further examination and treatment.
Dementia Knowledge and Item Responses
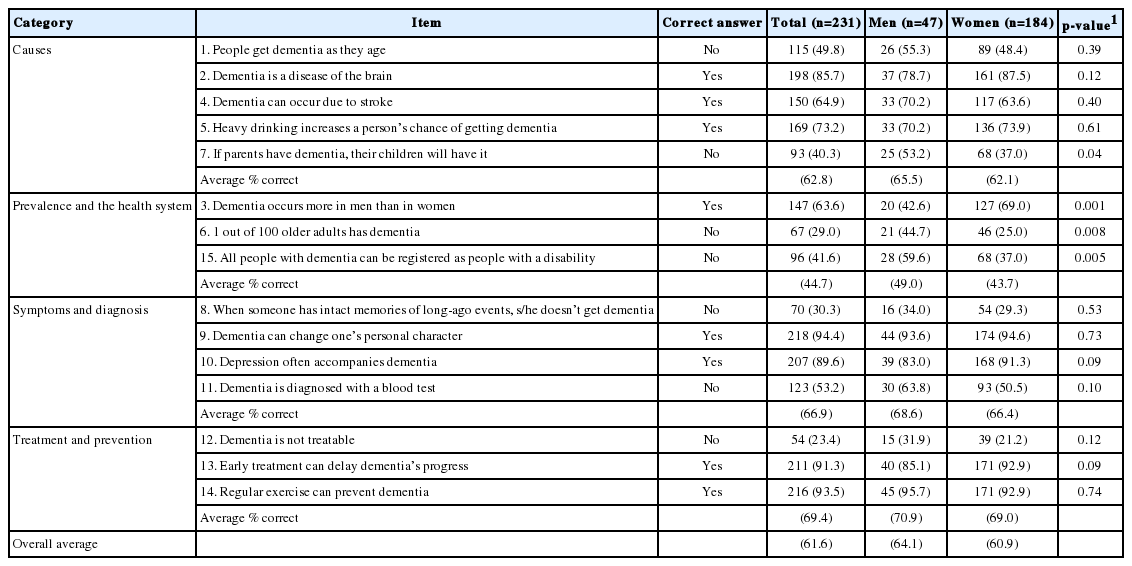
Table 2 summarizes the rates of correct answers for study participants. The average percentage of correct answers was 61.6%. Among the 4 categories of dementia knowledge, treatment and prevention showed the highest rate of correct answers (69.4%) followed by symptoms and diagnosis (66.9%), causes (62.8%), and prevalence and the health system (44.7%). Three items showed rates of correct answers over 90%. The highest rate was 94.4% for “Dementia can change one’s personal character.” The item “Regular exercise can prevent dementia” had a correct answer rate of 93.5%. The third-highest rate (91.3%) was for the item “Early treatment can delay dementia’s progress.”
The item with the lowest proportion of correct answers was “Dementia is not treatable” (23.4%). The item with the second lowest correct answer rate was related to the prevalence of dementia, as 71.0% of the participants mistakenly thought that dementia occurs in only 1 out of 100 people. The third lowest rate (30.3%) was for the item “When someone has intact memories of long-ago events, s/he doesn’t get dementia.” Other items that less than half of the participants answered correctly were: “If parents have dementia, their children will have it” (40.3%), “All people with dementia can be registered as people with a disability” (41.6%), and “People get dementia as they age” (49.8%).
There were differences in the mean DKS scores between men and women (64.1 for men and 60.9 for women). Statistically significant score discrepancies were found between men and women for the following items: “If parents have dementia, their children will have it,” “Dementia occurs more in men than in women,” “1 out of 100 older adults has dementia,” and “All people with dementia can be registered as people with a disability.” The correct answer rate of men respondents was higher than that of their women counterparts for the items listed above, except for the item “1 out of 100 older adults has dementia.”
Dementia Knowledge and Its Related Factors
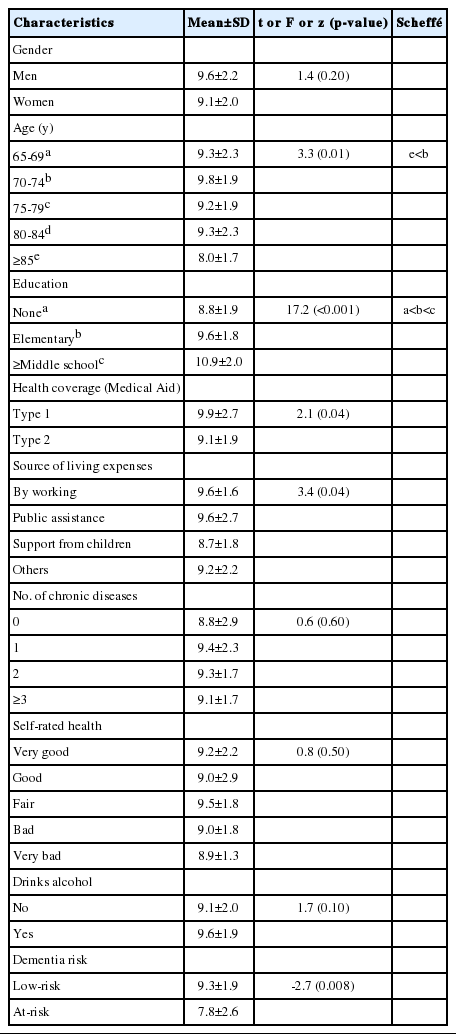
Table 3 shows the associations between study participants’ knowledge about dementia and their characteristics. Dementia knowledge was significantly associated with age (F=3.3, p=0.01), education (F=17.2, p< 0.001), health coverage (t= 2.1, p=0.04), source of living expenses (F=3.4, p=0.04), and MMSE-DS (z=-2.7, p=0.008).
People aged 85 and over scored only 8.0±1.7 on average, which was significantly lower than the average score (9.8±1.9) of those aged 70 to 74. Participants with no formal education scored lower (8.8±1.9) than those with an elementary education (9.6±1.8) or a middle school and above education (10.9±2.0). Type 1 Medical Aid beneficiaries showed a significantly higher level of knowledge (9.9±2.7) than their type 2 counterparts (9.1±1.9). Regarding the source of living expenses, a statistically significant difference was found, as those who received support from their children showed lower levels of knowledge (8.7±1.8), but the post-hoc analysis did not confirm this difference. The at-risk group of dementia according to the MMSE-DS showed the lowest average score of dementia knowledge (7.8±2.6). In contrast, the low-risk group scored 9.3±1.9.
DISCUSSION
It is well known that the prevalence of dementia is increasing globally. Many countries, including Korea, have begun to focus attention on how to deal with the burden of this disease. The knowledge level of rural older adults living alone about dementia, which is key for early detection and successful treatment, was assessed in this study.
The study participants showed relatively low levels of dementia knowledge (correct answer rate, 61.6%), confirming the results of previous studies of rural older adults [25]. Compared to the rural study participants, those in urban areas have shown higher correct answer rates (64.5, 66.7%) [26,27]. Although there were high correct answer rates within 4 categories, those of the study participants ranged from 44.7 to 69.4%, while those of urban older adults ranged from 60.6 to 66.1% [26]. Of particular note, roughly half of the study participants incorrectly believed that dementia is a part of aging. In other studies, only 23.4% of Korean urban residents [26] and 7.3% of Japanese residents believed this [28].
This study also underscores generational differences, as well as rural/urban differences, in knowledge about dementia. Other studies have found that citizens in their 20s had an average of 85.8% correct answers [27], and a group of adults had 75.0% [26]. These proportions were all higher than the rate of 61.6% among the participants in this study, who were in their mid-70s on average. This suggests that there is an urgent need to provide information on dementia to rural older adults living alone.
Participants’ lowest score was on the item “Dementia is not treatable,” which only 23.4% answered correctly. This proportion was lower than the 48.0% of Korean urban older residents [26] and 37.8% of Japanese community residents [28] who answered this item correctly. This negative belief was also reported in a US panel study [29], which highlighted the possibility that this belief could hinder older adults from actively seeking dementia treatment. However, in a 1999 national survey, only 5.7% of Korean citizens answered this correctly [30], and this improvement could be interpreted as the result of national outreach for dementia management.
Among the items regarding symptoms of dementia, participants showed relatively high levels of knowledge that dementia can change one’s character and can be accompanied by depression. However, only about 30.0% of the study participants were aware that long-term memory function remains intact in the early stages of dementia. This item also had a low correct answer rate among urban older adults (34.2%) [27]. Since study participants showed a high level of knowledge about the importance of early detection and regular exercise for preventing dementia, education about patterns of memory loss and about treatment could encourage them to actively seek dementia treatment. Educational outreach programs would be beneficial for improving the early detection and treatment of dementia.
The overall and categorical average correct answer rates of men respondents were higher than those of their women counterparts. Although statistically significant differences between men and women were found for only 4 items, the correct answer rate was higher for men than for women 9 of the 15 items. Because there was no significant difference in age between men and women, gender discrepancies in the correct answer rates can be attributed to the gender gap in education. In the past, Korean women had no choice but to sacrifice themselves for their brothers’ education, often against their will. In fact, there was a significant difference in educational level between the men and women study participants (data not shown). Previous studies have also reported that education was significantly associated with dementia knowledge [26, 29,30].
Old age and low levels of education have been reported to be significant factors related to knowledge levels about illnesses, including dementia [26-28]. The results of the current study confirmed this. Participants aged 85 years and older showed the lowest level of dementia knowledge. We further analyzed the mean MMSE-DS scores by age group, and the group aged 85 and older showed the lowest mean score on the MMSE-DS (20.9±4.3). It is possible that the deterioration of cognitive function with aging hindered older participants from obtaining new knowledge.
All of the participants received Medical Aid from the government, which is divided into types 1 and 2 assistance based on physical function and personal assets. Interestingly, participants who belonged to type 1 had more knowledge about dementia than their type 2 counterparts. Participants in the type 1 group had more free time than their type 2 counterparts because most of them did not work for their living (data not shown). Therefore, they tended to get help from and communicate with their community health practitioners, and were more likely to receive information on dementia. Regarding the source of living expenses, however, further investigation is needed to determine why working participants were more knowledgeable about dementia.
Health care providers in rural communities need to pay more attention to older adults living alone. Based on the MMSE-DS, approximately 6.9% of the study participants needed further evaluation for dementia. More than half of the participants experienced mild cognitive impairment; this proportion is markedly higher than the 27.8% reported in a national survey [2] and the 24.3% reported in urban community settings [31]. Other studies have also found rates of mild cognitive impairment of 5.0-36.7% among older community residents [32]. In addition, all of the participants lived alone, which is known to be an aggravator of cognitive function deterioration [15-18].
This study has some limitations. First, the study participants—rural older adults living alone—were not compared to their urban/younger counterparts and/or older adults living with others, and recruiting such counterparts in a future study will provide a more complete picture. Second, investigating their knowledge about other diseases, such as stroke, would have provided an opportunity to identify significant factors related to dementia knowledge in particular. Third, we did not employ a probability sampling technique, which might hamper the external validity of the study. For example, all of the participants were incidentally Medical Aid beneficiaries, although rural older adults living alone are known to be poorer than their younger and/or urban counterparts and the general population. Fourth, some variables associated with dementia knowledge were unfortunately not included in the study. For example, although a previous study [33] identified depression as a factor related to dementia knowledge, this study failed to measure the depression level of the study participants. The community health practitioners told the authors that there was little variation in the depression level among rural older adults, but a measure of depression should have been employed to confirm their impressions. Lastly, we did not provide results from multiple regression analysis. We conducted multiple linear regression analyses, but we were not sure that the results of the study would be robust because of the small sample size and selection bias. Instead, we aimed to focus on the level of dementia knowledge among older adults living alone in a rural area.
Despite the limitations mentioned above, this study showed that the level of dementia knowledge among Korean rural older adults living alone was relatively low. It was lower than among younger generations and urban older adults. Participants’ misconceptions about symptoms and treatment could hinder them from seeking early treatment. The results of this study suggest the need for active outreach and health care delivery for rural older adults living alone in Korea.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.