Interaction of Vitamin D and Smoking on Inflammatory Markers in the Urban Elderly
Article information
Abstract
Objectives:
Epidemiological studies have reported that vitamin D deficiency is associated with inflammatory disease. Smoking is a well-known risk factor for inflammation. However, few studies have investigated the interactive effect of vitamin D deficiency and smoking on inflammation. This study aims to investigate the interaction of vitamin D and smoking with inflammatory markers in the urban elderly.
Methods:
We used data from the Korean Elderly Environmental Panel Study, which began in August 2008 and ended in August 2010, and included 560 Koreans ≥60 years old living in Seoul. Data was collected via questionnaires that included items about smoking status at the first visit. Vitamin D levels, high-sensitivity C-reactive protein (hs-CRP), and white blood cell (WBC) counts were repeatedly measured up to three times.
Results:
The association of vitamin D and hs-CRP was significant after adjusting for known confounders (β=-0.080, p=0.041). After separate analysis by smoking status, the association of vitamin D deficiency and hs-CRP in smokers was stronger than that in nonsmokers (smokers: β=-0.375, p=0.013; non-smokers: β=-0.060, p=0.150). Smoking status was an effect modifier that changed the association between vitamin D deficiency and hs-CRP (interaction estimate: β=-0.254, p=0.032). Vitamin D was not significantly associated with WBC count (β=0.003, p=0.805).
Conclusions:
Vitamin D deficiency was associated with hs-CRP in the urban elderly. Smoking status was an effect modifier of this association. Vitamin D deficiency was not significantly associated with WBC count.
INTRODUCTION
Vitamin D concentration is increased by exposure to sunlight. Urban residents spend most of their time in indoor spaces, resulting in vitamin D deficiency, the prevalence of which is high worldwide. Vitamin D insufficiency (≤20 ng/mL) is 41.6% in US adults, based on data from the 2005-2006 National Health and Nutrition Examination Survey [1].
Researchers have been concerned with health outcomes in relation to vitamin D deficiency. It is well-known that vitamin D deficiency is associated with osteoporosis through its effects on parathyroid hormone [2,3]. Several studies show that vitamin D deficiency is also associated with chronic diseases such as cardiovascular disease [4,5] and cancer [6,7]. Other studies have found vitamin D deficiency to be associated with inflammatory disease. In the Iowa Women’s Health Study, low vitamin D ingestion was associated with rheumatoid arthritis [8], and vitamin D deficiency has been associated with disease severity in systemic lupus erythematosus patients [9].
Elderly people are especially vulnerable to the risks of vitamin D deficiency, because they tend to spend more time indoors, receive less dietary vitamin D, be more obese, and have reduced renal function [10].
Smoking is associated with vitamin D levels [11] and is a well-known risk factor for inflammation [12,13]. However, few studies have quantitatively assessed whether smoking modifies the impact of vitamin D on inflammation. The aims of our study were to investigate the association of vitamin D and inflammatory markers and to evaluate whether the association changes with smoking status in the urban elderly.
METHODS
Study Population
We used data from the Korean Elderly Environmental Panel Study, which included 560 Koreans aged 60 years or older living in Seongbuk-gu, Seoul, Republic of Korea (hereafter Korea). The study began in August 2008 and ended in August 2010. Baseline surveys and the first measurement were performed between August 2008 and December 2008. The second measurement was performed between April 2009 and October 2009, and the third between March 2010 and August 2010. We excluded participants with an acute inflammatory condition, levels of high-sensitivity C-reactive protein (hs-CRP) ≥1 mg/dL, or a white blood cell (WBC) count ≥10 000/μL [14,15]. We also excluded participants with missing measures of vitamin D, hs-CRP, and WBC count. A final total of 529 participants were included in our study. Among them, the numbers of participants that visited once, twice, or three times were 213, 204, and 112, respectively. All participants submitted written informed consent. Seoul National University Hospital approved the study protocol (IRB no. H-0804-045-241).
Surveys and Laboratory Measurements
Skilled interviewers collected information using standard questionnaires. These included questions about age, sex, smoking status (smoked at least 400 cigarettes in life: yes/no) [16], alcohol consumption (alcohol drinking at least once a month in life: yes/no), and physical activity (exercise to the point of sweating in last week: <1-2 days or ≥1-2 days). Height and weight were measured in each series of the study.
Blood samples were taken from overnight-fasting participants at around 10:00 and stored at -70°C. Vitamin D levels were measured in blood samples as 25-hydroxyvitamin D (25[OH]D) concentrations; 25(OH)D is a widely used measure that reflects sun exposure and dietary intake [17]. 25(OH)D was measured using LIAISON equipment for chemiluminescent immunoassay (DiaSorin Inc., Stillwater, MN, USA); the limit of detection was 4 ng/mL.
Hs-CRP levels were measured using latex agglutination turbidimetry with an automated analyzer (Hitachi 7180, Hitachi High-Technologies, Tokyo, Japan) and reagents (Pure Auto S CRP latex, Daiichi Pure Chemicals, Tokyo, Japan). Quality control was performed using an hs-CRP calibrator according to the protocol. WBC counts were measured using a cell counter.
Statistical Analysis
Continuous variables (vitamin D, hs-CRP, WBC count, body mass index [BMI]) were right-skewed, so they were natural log-transformed before further analysis. We used the χ2-test and Student’s t-test to analyze baseline characteristics and distribution of variables. To explore the association of vitamin D concentration with inflammatory markers, we used generalized estimating equations (GEE). Model 1 had only one explanatory variable (vitamin D concentration). Model 2 had three adjustment variables (age, sex, visit number) in conjunction with model 1. Model 3 had five adjustment variables (smoking status, alcohol consumption status, exercise status, BMI, month of visit) in conjunction with the variables of model 2. We adjusted for the month of the visit in consideration of the seasonal variation of vitamin D and inflammatory markers [18,19]. Model 3 plus an interaction term (log-transformed vitamin D*smoking) in GEE was used to evaluate the vitamin D-smoking interaction on inflammation. The statistical programs SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) and R version 2.15.2 (Comprehensive R Archive Network [http://cran.r-project.org]) were used for all analyses.
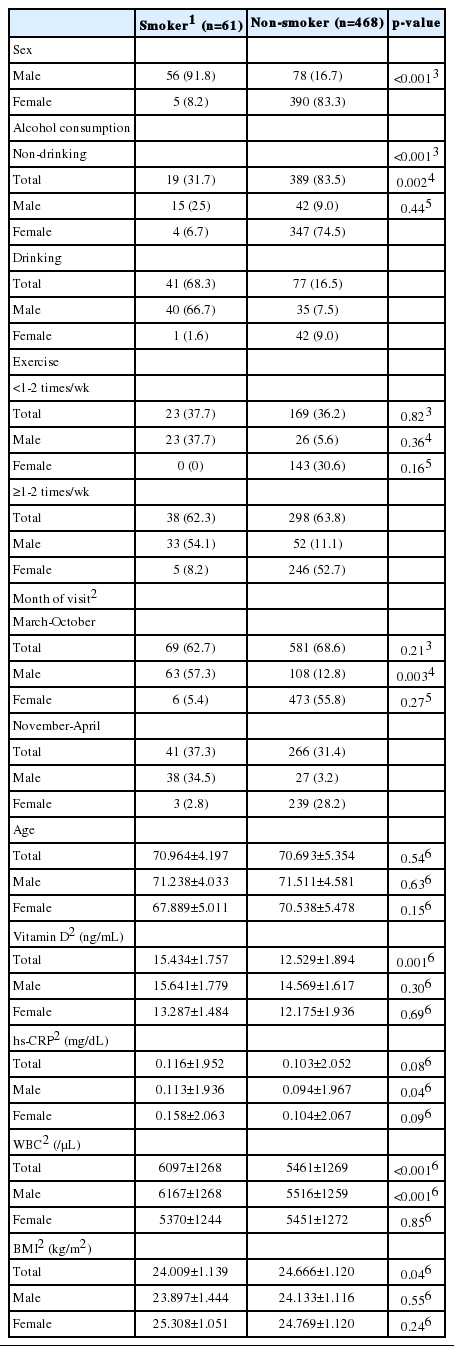
RESULTS
Table 1 shows the participant characteristics, stratified by smoking status. There were 61 smokers (11.5%) among the participants. 91.8% of smokers and 16.7% of non-smokers were male. Given the sex difference in smoking status, we described participant characteristics separately by sex. Among all participants, smokers had higher vitamin D concentrations than non-smokers, and the difference is statistically significant (p=0.001). However, there is no significant difference after stratification by sex. Smokers had slightly higher hs-CRP concentrations than non-smokers among all participants and among males (p= 0.085 in total, p=0.040 in males). Additionally, smokers had higher WBC counts than non-smokers among all participants and among males (p<0.001 in total, p<0.001 in males). Age was not different between smokers and non-smokers.
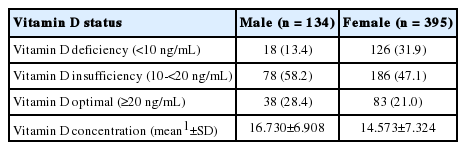
Table 2 shows the participants’ vitamin D status. We used average values calculated from repeated measures on the same participants. Only 28.4% of males and 21.0% of females had optimal vitamin D concentrations. About half of the participants were of vitamin insufficiency status (males, 58.2%; females, 47.1%), and some were at vitamin D deficient status (males, 13.4%; females, 31.9%). The reference value for vitamin D was defined according to Tracher et al. [20].
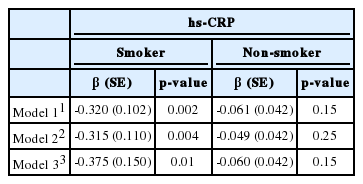
The association of serum vitamin D concentration with inflammatory markers is shown in Table 3. After adjusting for known confounders, the association of vitamin D deficiency and hs-CRP was significant. (β=-0.080, p=0.041). However, there was no significant association between vitamin D deficiency and WBC count (β=0.003, p=0.805).
Effect modification was observed when we analyzed separately by smoking status (Table 4). In smokers, vitamin D deficiency was significantly associated with hs-CRP after controlling for known confounders (β=-0.375, p=0.013). In non-smokers, the estimate of association was smaller than in smokers and was not statistically significant (β=-0.060, p=0.150).
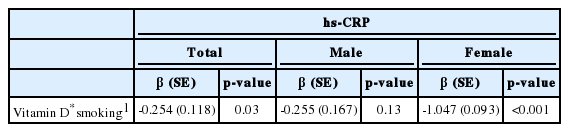
Table 5 shows that the estimate of interaction between vitamin D concentration and smoking status on hs-CRP was significant (β=-0.254, p=0.032). The estimate of association in smokers is considered to be significantly different from that in non-smokers, because the p-value of the interaction is significant in multiple linear regression [21]. Supplemental Figure 1 shows slopes of vitamin D-hs-CRP association curves differ depending on smoking status. Because most smokers were males, we analyzed separately by sex. In females, there was a stronger interaction effect (β=-1.047, p<0.001). In males, the interaction effect was not significant (β=-0.255, p=0.126). However, the interaction estimate in males was not attenuated in comparison with that in total subjects, and its direction did not change, so the non-significant result might simply be due to the weaker statistical power in analyzing males separately (smaller sample size).
The association of vitamin D and inflammatory markers, stratified by sex, is shown in Supplemental Table 1. The estimate of the association in males was slightly different from that in females, and the interaction effect of vitamin D-sex on hs-CRP was not significant (β=-0.077, p=0.428).
DISCUSSION
The main findings of this study are that there is a significant association of vitamin D deficiency and hs-CRP, and that smoking status is an effect modifier of this association such that smokers have a stronger association of vitamin D deficiency and hs-CRP than non-smokers.
Previous studies have reported the association of vitamin D deficiency and hs-CRP. Mellenthin et al. [18] reported that 25(OH)D concentrations were inversely associated with hs-CRP in the general adult population. Patel et al. [22] showed that concentrations of 25(OH)D and 1,25-dihydroxyvitamin D (1,25[OH]2D), a bioactive form of vitamin D, were inversely associated with CRP in patients with early inflammatory polyarthritis. A meta-analysis investigated the association of dietary supplemental vitamin D with hs-CRP and reported a pooled effect of -1.08 mg/L (95% CI, -2.13 to -0.03, p<0.01) [23]. Our results are in line with these studies. Some studies have suggested mechanisms for how vitamin D affects inflammation. Wang et al. [24] showed that diabetic peritonitis was attenuated in diabetic mice by intraperitoneal injection of 25(OH)D. Treatment with 25(OH)D induced vitamin D receptor expression but inhibited toll-like receptor 4 (TLR4). Moreover, 25(OH)D inhibited the signal transducer and activator of the transcription 3 (STAT3) signaling pathway. Both TLR4 and STAT3 are associated with signaling pathways in inflammation and the immune system. Other animal studies show that 1,25(OH)2D inhibited activation of nuclear factor kappa-light-chain-enhancer of activated B cells, which is a transcription factor that plays an important role in inflammation and the immune system [25-27].
Some studies report conflicting results, however Shea et al. [17] reported that vitamin D levels were inconsistently associated with inflammatory markers. They did not find an association of 25(OH)D levels and hs-CRP levels; however, their study had some different factors (age of participants, exclusion criteria, analysis method) from those in our study. Eren et al. [28] showed that vitamin D levels are not associated with inflammatory markers in patients with acute coronary syndrome; however, their participants did not represent the general population.
Few studies have investigated the interaction between smoking and vitamin D on inflammation. Merlino et al. [8] previously suggested such an interaction in a cohort study in older females. Compared to nonsmokers with low vitamin D intake, smokers with higher vitamin D intake had a trend of lower risk of rheumatoid arthritis, while smokers with lower vitamin D intake were at increased risk of the disease. However, the estimate of interaction was not significant.
There are few epidemiological studies showing the association of vitamin D and WBC count. Mellenthin et al. [18] investigated the association of vitamin D deficiency and WBC count in the general adult population and found that vitamin D deficiency was associated with WBC count in smokers (n=718) but in non-smokers (n=2005). Yildirim et al. [29] reported no significant difference in WBC count between vitamin D deficient patients and control groups.
We did not find a significant association between vitamin D deficiency and WBC count. After analyzing separately by smoking status, we did not find significant associations in either smokers or non-smokers (data not shown). Moreover, we did not find any vitamin D-smoking interaction effect on WBC count (β=-0.04, p=0.680). However, some studies have investigated the association of vitamin D and specific WBC type. Some studies have found that 1,25(OH)D prevented differentiation and maturation of dendritic cells [30,31], while de Groot et al. [32] showed that vitamin D treatment lowered the eosinophil count in non-atopic asthma patients who had a high baseline eosinophil count. We suggest that evaluation of different forms of inflammatory cells, not just the total WBC count, may be a useful method to identify the association of vitamin D and inflammation.
We found that more than 70% of older adults in our study were vitamin D insufficient. The arithmetic mean level of vitamin D concentration was 16.73 (standard deviation [SD], 6.91) in males and 14.57 (SD, 7.32) in females. According to the 2010-2011 Korean National Health and Nutrition Examination Survey, the mean vitamin D concentrations were 20.13 to 20.51 ng/mL in males ≥60 years and 18.20 to 18.92 ng/mL in females ≥ 60 years [33]. Vitamin D concentrations in our study participants may be slightly lower than the national level because all of the participants are in an urban area (Seoul); some studies have reported differences in vitamin D levels between urban and rural areas [33,34].
Previous studies have shown that smokers have lower vitamin D concentrations than non-smokers [11,35]. In our study, smokers had higher vitamin D concentrations. This may result from sex differences in vitamin D concentrations; females tend to have lower vitamin D concentrations [33,34]. In our study, most smokers were males. We calculated the estimate of interaction between vitamin D and sex, but no effect modification was observed, such that the effect modification between vitamin D and smoking on hs-CRP resulted from a true effect of smoking and not from an effect of sex.
Our study has several limitations. First, all of the participants were elderly people living in an urban area, and thus the results may not be generalizable to other age groups or areas. Second, our study design is limited in its ability to make causal inference, although repeated measurements strengthened the validity of association. Third, we could not completely exclude the presence of inflammatory diseases. We collected diagnoses of the diseases through questionnaires completed by participants; however, due to the potential for recall bias, we excluded participants with high levels of inflammatory markers suggestive of acute inflammatory status. Fourth, the measurable inflammatory markers in our study were limited.
CRP is a well-known non-specific inflammatory marker. The hs-CRP method can detect very low levels of CRP (lower detection limits of 0.02 mg/dL) [36]. Hs-CRP concentrations increase slightly with low-level inflammation (coronary artery disease, mild chronic infection, and tissue damage, etc.), and are markedly increased with high-level inflammation (bacterial or fungal infection) [37]. The total WBC count is also a well-known non-specific inflammatory marker. The WBC count increased with low-level inflammation (chronic inflammation, smoking, stress, etc.) and markedly increased with high-level inflammation (bacterial infection, bone marrow disease, etc.). Given the potential for high-level inflammation to distort the association of vitamin D and inflammatory markers, we excluded participants considered to be in an acute or severe inflammatory state from our analysis. These two non-specific inflammatory markers may not be enough, however, to represent chronic low-level inflammation. Therefore, further studies are needed to investigate the association of vitamin D level and other inflammatory markers such as cytokines or specific WBC types. To our knowledge, this is the first study reporting that smoking status is a significant effect modifier of the vitamin D deficiency–hs-CRP association.
We have found that significant association of vitamin D deficiency and hs-CRP in the urban elderly. Smoking status is an effect modifier of this association. In urban elderly smokers, vitamin D deficiency appears to be more risky for increasing hs-CRP. However, we could not find a significant association of vitamin D and WBC count. Larger longitudinal studies are needed to investigate associations of vitamin D and other inflammatory markers and any causal relationships.
ACKNOWLEDGEMENTS
This study was partially supported by the Women Scientist Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (#2015R1A1A3A04001325).
Notes
Conflict of Interest
The authors have no conflicts of interest with the material presented in this paper.
Supplementary Material
Associations of serum vitamin D concentration with serum hs-CRP and WBC count: stratification by sex