Association of Demographic and Socioeconomic Factors With Risk Factors for Chronic Kidney Disease
Article information
Abstract
Objectives:
The goal of this study was to examine the association of various demographic and socioeconomic factors with risk factors for chronic kidney disease (CKD).
Methods:
We used nationally representative pooled data from the Korea National Health and Nutrition Examination Survey (KNHANES), 2007–2013. We estimated the glomerular filtration rate (GFR) using the Modification of Diet in Renal Disease equation. We defined CKD as a GFR <60 mL/min/1.73 m2, and 1304 of the 45 208 individuals included in the KNHANES were found to have CKD by this definition. The outcome variable was whether individual subjects adhered to the CKD prevention and management guidelines recommended by the Korea Centers for Disease Control and Prevention. The guidelines suggest that individuals maintain a normal weight, abstain from alcohol consumption and smoking, manage diabetes and hypertension, and engage in regular exercise in order to prevent and manage CKD.
Results:
This study found that individuals with CKD were more likely to be obese and have hypertension or diabetes than individuals without CKD. In particular, male and less-educated CKD patients were less likely to adhere to the guidelines.
Conclusions:
Although the prevalence of CKD, as indicated by the KNHANES data, decreased from 2007 to 2013, the prevalence of most risk factors associated with CKD fluctuated over the same time period. Since a variety of demographic and socioeconomic factors are related to the successful implementation of guidelines for preventing and managing CKD, individually tailored prevention activities should be developed.
INTRODUCTION
Chronic kidney disease (CKD) is a global problem, and its prevalence is increasing dramatically. According to data from the National Health and Nutrition Examination Survey, the prevalence of CKD in the US was 14.0% between 2007 and 2010, which was greater than the 13.1% prevalence observed in 2004 [1,2]. The prevalence of CKD in Asia is equivalent to or higher than in Western countries. The prevalence of a glomerular filtration rate (GFR) <60 mL/min/1.73 m2 in the adult Japanese population is 19.1% [3]. A recent study found the prevalence of CKD in Beijing to be 13.0% [4]. The socioeconomic burden of CKD is alarming in the Republic of Korea (hereafter Korea), where the total direct and indirect costs associated with CKD were estimated to be over 5000 billion Korean won (US$ 5 billion) in 2011 [5]. The prevalence of CKD has increased significantly over the past decade, resulting in the greater utilization of related health care services. The increasing burden of CKD has led to increased interest in strategies for preventing and managing CKD. The Korean Society of Nephrology and the Korea Centers for Disease Control and Prevention (KCDC) have recently published guidelines for the prevention and management of CKD. Previous studies have indicated that it is important for CKD patients to avoid several risky health behaviors, such as smoking, drinking, and obesity, in addition to managing hypertension and diabetes and engaging in regular exercise [6].
Smoking has been found to be related to CKD, independently of several important confounders. Similarly, heavy drinking, defined as the consumption of four or more standard units of alcohol per day, has been found to be associated with CKD [7]. Smoking has emerged as an important modifiable kidney risk factor based on multiple studies that have documented a distinct association between smoking and renal injury among the general population. Several studies have documented smoking-related alterations that have been proven to be harmful to the kidney [8]. Joint exposure to both current heavy drinking and smoking was associated with almost five-fold increased odds of developing CKD compared to the absence of these factors (odds ratio [OR], 4.93; 95% confidence interval [CI], 2.49 to 9.94) [7]. Moreover, CKD appears to be associated with the risk of total stroke, showing a particularly strong association with hemorrhagic stroke in males and ischemic stroke in females [9].
Obesity has been increasingly regarded as an major risk factor for the development of CKD [10]. Obesity is a major risk factor for the progression of kidney damage. Obesity leads several pathophysiologic disorder that contribute to renal damage [11]. Overweight and obese people are more apt to generate albuminuria and, at least in some types of kidney disease, a more speedy progression and greater amount of albuminuria of renal failure. Preliminary material indicate that many of the nephropathologic manifestations associated with obesity can be ameliorated with reductions in body fat caused by dietary energy control or surgical procedures which reduce intake [12]. It has been confirmed that the presence of obesity accelerates the progression of CKD in patients with CKD of various etiologies. Moreover, firm links have been established between obesity, proteinuria, and the progression of CKD [13]. Unusual kidney function, induced by increased renal tubular reabsorption, begins volume expansion and the hypertension, and increased blood pressure during excessive weight gain, and metabolic abnormalities related to obesity, in turn, contribute to chronic kidney disease [14].
Observational studies have reported a significant inverse association of physical function and aerobic capacity with mortality in patients with CKD. Such studies have provided evidence that exercise may cause a decrease of cardiovascular disease risk factors. The evidence supports therapeutic exercise as a helpful treatment for patients with CKD [15]. There is proof of the benefit of regular exercise in a lot of long period conditions including CKD [16]. The contribution of diseases related to aging, such as diabetes mellitus and hypertension, may accelerate this decrease in renal function with aging and therefore raise the incidence of chronic kidney disease [17]. The joint recommendations of the American Society of Nephrology and the National Kidney Foundation provide helpful guidelines for the management of hypertension patients with CKD. They recommend a goal blood pressure for all CKD patients of <130/80 mmHg [18].
Numerous studies have suggested that socioeconomic disparities exist in the prevention and management of disease in general [19-25]. CKD is not likely to be an exception to this generalization; therefore, this study examined the association of various demographic and socioeconomic factors with risk factors for CKD in the Korean population.
METHODS
Data Source and Subjects
The data used in this report were obtained from the cross-sectional, nationally representative 2007–2013 Korea National Health and Nutrition Examination Survey (KNHANES) performed by the Korean Ministry of Health and Welfare. A stratified multistage probability design was used, with subject selection made from sampling units using household registries. A total of 6000 households containing 13 173 individuals each year took part in the survey, which consisted of four parts: a health interview survey, a health consciousness and behavior survey, a physical examination, and a nutrition survey. As the raw data are open to the public for scientific use, ethical approval was not needed for this study.
We analyzed cross-sectional data from 58 423 individuals who answered the health behavior survey completely. Since we estimated the GFR from serum creatinine levels, we excluded subjects for whom this information was not available. Thus, a total of 45 208 subjects were included in our analysis.
Independent Variables and Outcome Variables
The level of kidney function was ascertained by using an abbreviated equation developed to estimate the GFR using data from the Modification of Diet in Renal Disease study. The National Kidney Foundation Kidney Disease Outcome Quality Initiative has defined CKD as a GFR <60 mL/min/1.73 m2, and this definition was applied in our study.
In the present study, the outcome variable was whether individuals adhered to the CKD prevention and management guidelines. We defined non-compliance to the guidelines as obesity, alcohol consumption or smoking, the absence of regular exercise, diabetes, or hypertension. Hypertension was indicated by a systolic pressure ≥140 mmHg, a diastolic pressure ≥90 mmHg, or the use of anti-hypertension medication. Diabetes was identified by a fasting blood glucose level ≥126 mg/dL, a diagnosis based on a physical examination performed by a doctor, or the use of a hypoglycemic agent. We defined regular exercise as at least three exercise sessions per week, and obesity as a body mass index ≥ 25 kg/m2. Individuals were categorized as smokers if they were current smokers, and were classified as drinkers if they had consumed alcohol over the course of the previous year.
We analyzed the following demographic and socioeconomic factors: age, sex, education, marital status, household income, residence, and occupation. The participants were classified into four age groups (≤49, 50-59, 60-69, and ≥70). Education levels were categorized into three groups (none or elementary school, middle or high school, and university or higher). Marital status was divided into two categories: married and not married. The household income quartile was sourced from the KNHANES, and the adjusted household income was calculated by dividing the household monthly income by the square root of the household size. Based on this method of calculating the household income, the KNHANES subjects were ranked from lowest to highest and then grouped into four household income quartiles (1 being the lowest and 4 being the highest), each containing approximately 25% of the survey population. Residence was categorized into (1) metropolis (Seoul, Busan, Daegu, Incheon, Daejeon, Gwangju, and Ulsan) or (2) rural. Occupations were categorized into six groups (managers or professionals; office workers; service workers or retailers; agriculture or fishery employees; technicians, mechanics, or assemblers; and simple laborers).
Statistical Analysis
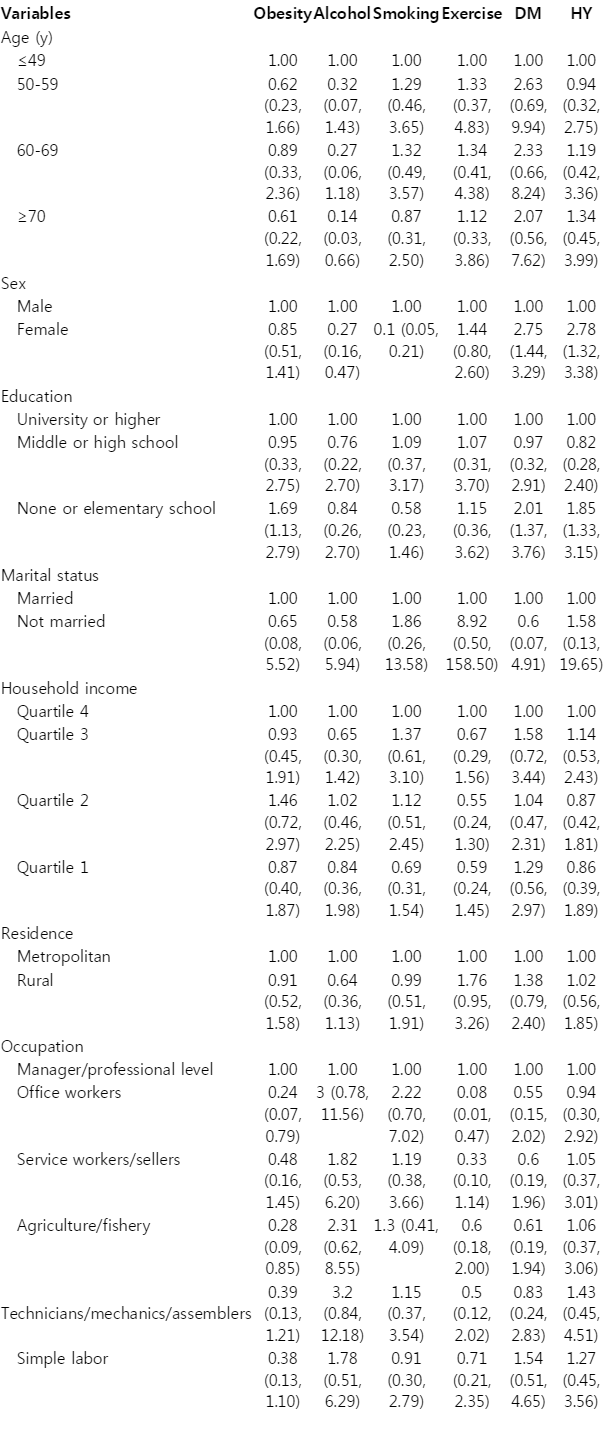
We used descriptive statistical methods to present the characteristics of the subjects, and reported the number and percentage for each variable. ORs with 95% CIs were calculated to measure the strength of the association between the demographic variables and the six guideline-related outcome variables in this study population. All variables were tested in a multiple logistic regression model, in which the proc survey logistic procedure was used. Multiple logistic regressions were tested on the six guideline-related outcomes (obesity, alcohol consumption, smoking, exercise, diabetes, and hypertension). All statistical tests were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
RESULTS
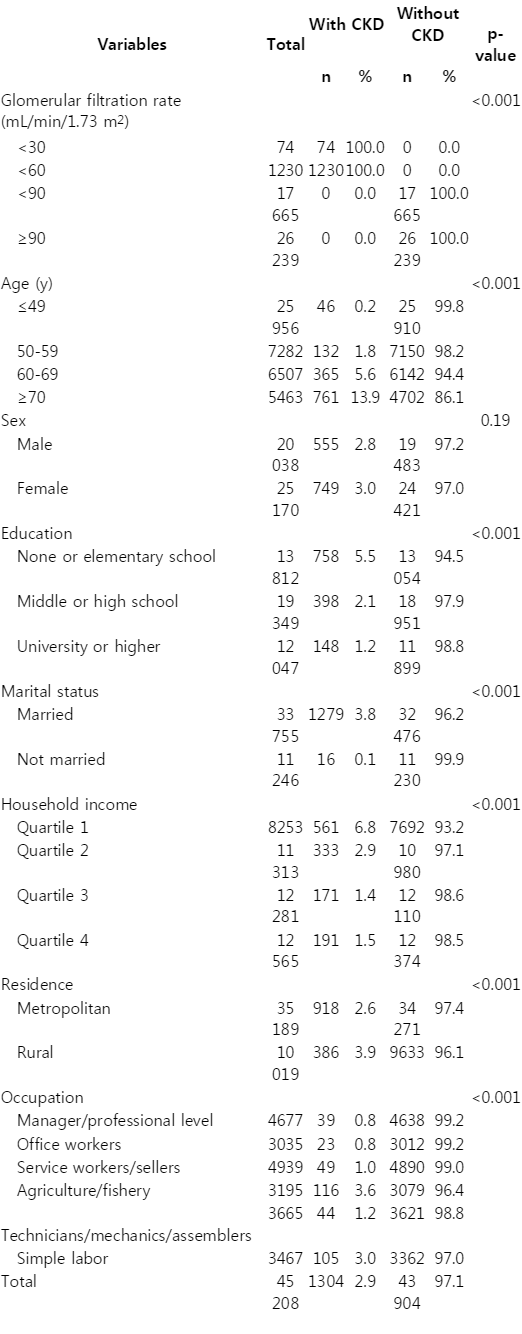
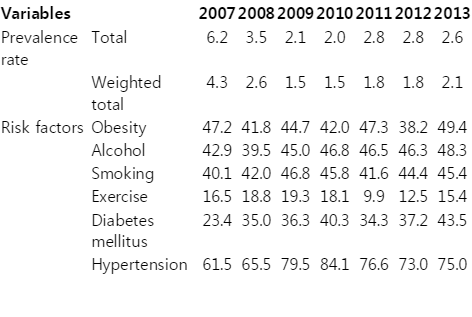
We examined the demographic and socioeconomic status of respondents depending on their CKD status using pooled data from the KNHANES, 2007–2013 (Table 1). Roughly 2.6% of individuals in the pooled data were identified as having CKD. The demographic and socioeconomic profiles of the individuals with CKD were different from those without CKD, with the exception of sex. Table 2 shows the prevalence of CKD by year, showing that the prevalence decreased over time (from 6.2% in 2007 to 2.6% in 2013). In addition, we examined the prevalence of risk factors associated with CKD by year. The prevalence of most risk factors fluctuated over the time interval studied.
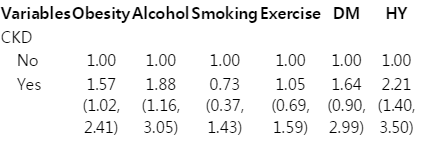
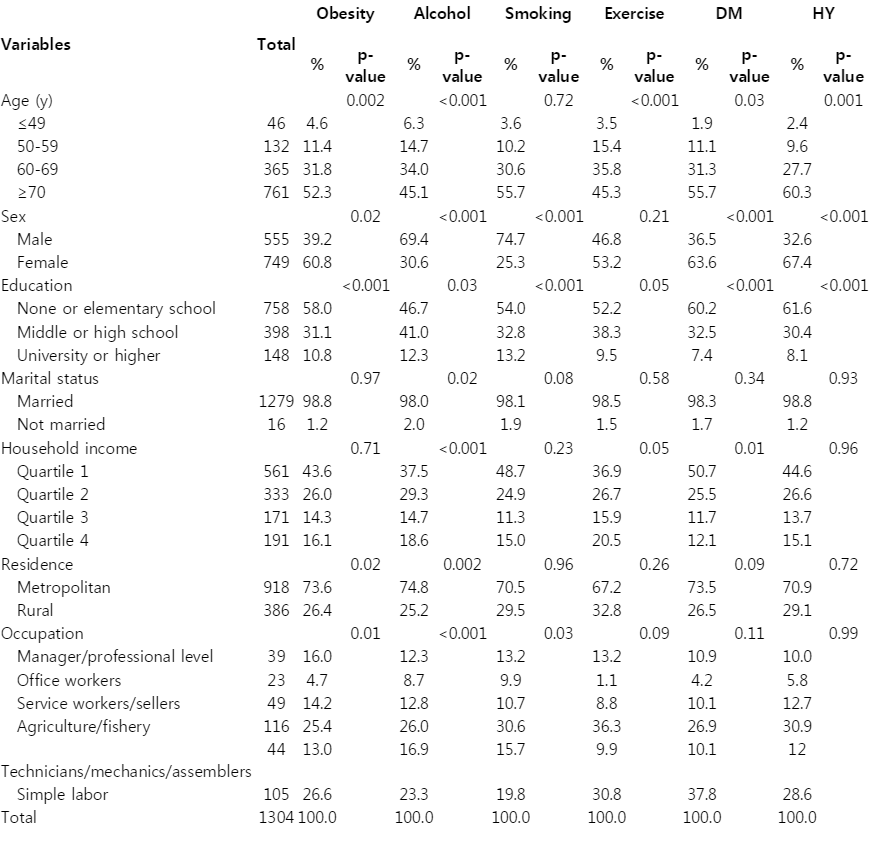
We found that individuals with CKD were more likely to be obese and have hypertension or diabetes than individuals without CKD (Table 3). The results of the general characteristics and multiple logistic regression analysis examining the associations of demographic and socioeconomic variables with the six preventative guideline-related outcomes among individuals with CKD are presented (Tables 4 and 5). Age was negatively associated with alcohol consumption, and female patients were more likely than their male counterparts to adhere to the CKD prevention guidelines. Higher education levels were associated with lower rates of obesity, diabetes, and hypertension. Marital status, household income, and residence did not show significant effects, and some occupation categories only showed a significant effect for obesity and exercise.
DISCUSSION
We analyzed six outcome variables that reflect the guidelines recommended by the KCDC for the prevention and management of CKD. Although the prevalence of CKD decreased from 2007 to 2013, the prevalence of most risk factors associated with CKD fluctuated over this time interval. These findings may indicate that public health programs encouraging patients with CKD to adhere to health guidelines need to be strengthened.
Individuals with CKD were more likely to be obese and to have hypertension or diabetes than individuals without CKD. Obesity is a major risk factor associated with CKD. An ongoing obesity epidemic has been observed throughout the world [26,27]. Obesity is linked to pathogenic mechanisms of kidney injury and has been associated with kidney disease in animal models. Obesity is a modifiable risk factor for diabetes and hypertension, which are the two most common causes of progressive CKD and end-stage renal disease in most populations. Ample evidence exists that extreme obesity is associated with albuminuria, a biomarker of kidney injury, reflecting a distinctive pattern of obesity-related glomerulopathy. Evidence also exists indicating that the behavioral, pharmacological, and surgical treatment of obesity-related CKD may be effective in modifying the biomarkers of kidney injury (i.e., increased renal blood flow and proteinuria). Moreover, extensive evidence has been presented that individuals with CKD and patients who progress to end-stage renal disease have a higher prevalence of obesity than other groups [28]. These observations provide the context for a discussion of whether current evidence supports recommendations for public health action to reduce the burden of obesity-related CKD.
No significant differences regarding physical activity were found among individuals with and without CKD. Physical activity confers diverse biological benefits that may counteract the adverse metabolic environment of CKD. Conversely, physical inactivity contributes to the development of CKD, particularly through diabetes and hypertension, which are the most common causes of kidney disease [29-33]. Continued improvement in the monitoring of physical activity would help guide development of policies and programs to increase the activity levels of patients with CKD, thereby reducing the overall burden of non-communicable disease. Collaboration with community agencies would play a crucial role in successfully implementing such plans. For example, making use of existing transportation systems may assist patients in attending health screenings, clinic appointments, or dialysis treatment. Local gyms and schools may offer reduced or free educational sessions related to wellness activities, such as exercise programs or basic health education.
CKD is often caused by diabetes mellitus and hypertension. Both diabetes mellitus and hypertension are treatable and preventable; however, the population of individuals diagnosed with these two diseases is increasing. Health promotion and early detection are key factors in reducing the incidence of diabetes mellitus and hypertension and thus reducing the incidence of CKD.
Among individuals with CKD, being male or less educated corresponded to a lower likelihood of following the guidelines for preventing and managing CKD; therefore, efforts to improve the adherence to such guidelines may need to be tailored specifically to those groups.
Our study has some limitations. First, the present study employed a cross-sectional design. Therefore, we could not confirm a definite causal relationship between CKD and the associated risk factors. Second, we did not analyze nutritional factors that could affect CKD. Third, since variables such as smoking, alcohol consumption, and exercise are estimated by self-reporting, there is a risk of inaccurate self-reporting caused by recall bias. However, the prevalence of obesity, hypertension, diabetes mellitus, and CKD as indicated by GFR was estimated based on data from physical examinations.
Despite the above limitations, our study is the first empirical study designed to examine demographic and socioeconomic factors associated with the prevention and management of CKD in Korea. Individuals with CKD were more likely to be obese and to have hypertension or diabetes than individuals without CKD. Since a variety of demographic and socioeconomic factors are related to the prevention and management of CKD, individually tailored prevention activities must be developed and implemented.
ACKNOWLEDGEMENTS
This work was supported by the Korea Centers for Disease Control and Prevention (no. 2012 E3301900#). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Notes
Conflict of Interest
The authors have no conflicts of interest with the material presented in this paper.