Differences in the Levels of Gastric Cancer Risk Factors Between Nanjing and Minqing Counties, China
Article information
Abstract
Objectives:
In Fujian Province, China, gastric cancer is one of the leading causes of mortality among all malignant tumors. Nanjing county and Minqing county are located in inland Fujian and have similar general demographics. However, the adjusted mortality rate of gastric cancer in Minqing was found to be much higher than that in Nanjing. We sought to explore factors associated with this increased risk of gastric cancer between the two counties.
Methods:
We recruited 231 and 224 residents from Nanjing and Minqing, respectively, and analyzed differences between their dietary habits, Helicobacter pylori infection rates, and concentrations of serum pepsinogen I, pepsinogen II, gastrin-17, and ratio of pepsinogen I:II.
Results:
Subjects in Minqing had more first-degree relatives who had been diagnosed with upper gastrointestinal tumor, more unhealthy dietary habits, a higher Helicobacter pylori positive rate, and greater proportion of abnormal serum gastrin-17 than those in Nanjing did.
Conclusions:
The factors that differed between these two counties might indicate that residents in Minqing have a higher risk for developing gastric cancer than those in Nanjing do.
INTRODUCTION
Gastric cancer is one of the most common malignant tumors causing death in China. In 2012, the adjusted morbidity rate of gastric cancer was 22.7/100 000 persons, only second to lung cancer out of all types of malignancies in China. The adjusted mortality rate of gastric cancer was 17.9/100 000 persons, the third leading cause of death among all malignancies [1]. In Fujian Province, located in southeast China, the adjusted mortality rate of gastric cancer in 2011 was 18.7/100 000 persons (data on the incidence rate of gastric cancer is not available). The mortality rate of gastric cancer varies throughout China; for example, the first national survey on all-cause mortality showed that the adjusted mortality rate of gastric cancer was 39.4/100 000 persons in coastal areas, but 16.2/100 000 persons in inland areas [2].
Nanjing county and Minqing county are both inland areas in Fujian province. According to 2010 data from the Office for National Statistics, the populations were 349 918 and 306 471 and the mortality rates were 0.642 and 0.634% in Nanjing county and Minqing county, respectively. Although these two counties have similarly sized populations and similar mortality rates, the adjusted mortality rate of gastric cancer was 29.7/100 000 in Minqing, which was much higher than that in Nanjing (19.5/100 000). Unfortunately, the incidence rates of gastric cancer in these two counties were not available. Although mortality is substantially influenced by the cancer stage and other clinicopathological features, we think that the incidence rates of gastric cancer in Minqing might be higher than that in Nanjing.
Family history, Helicobacter pylori (H. pylori) infections, consuming foods rich in salt or nitro compounds, and unhealthy dietary habits have been reported as significant risk factors for developing gastric carcinoma [3-5]. Unsurprisingly, previous studies have also shown that eating fruits and vegetables, drinking tea, and having good dietary habits are protective factors against the disease [6,7]. Recently, serological parameters of gastric cancer such as serum pepsinogen (PG) I and II, gastrin-17 (G-17), and the H. pylori antibody have been applied to evaluate the risk for developing gastric cancer and its precancerous lesions known as atrophy gastritis [8-10]. A low PG I or low ratio of PG I to PG II can be an indication of gastric corpus atrophy, and a low G-17 level can reflect a gastric antrum atrophy. Moreover, the presence of H. pylori antibodies can indicate infection.
We aimed to investigate differences in the dietary habits, family history, H. pylori infection rate, and distributions of serum PG I, PG II, ratio of PG I:II, and G-17 level between people living in Minqing and Nanjing to reveal factors associated with the higher prevalence of gastric cancer in Minqing than that in Nanjing.
METHODS
Subjects
A multi-stage sampling method was adopted to recruit subjects in Nanjing and Minqing. First, three towns were randomly selected from 11 towns in each county. Then, two out of six villages from each target town were randomly selected, and 30 to 40 families from each target village were selected by the simple random selection method. Last, one participant from each family was recruited if they were aged between 30 to 70 years, had been living in that county for at least five years, were without any clinically diagnosed gastric diseases, and had never taken a proton pump inhibitor. If this recruited participant refused participation, another person living in that village and meeting these requirements were recruited; the replacement rate was less than 10%. Every subject provided informed consent before participation.
Data Collection
Trained investigators used a questionnaire to obtain self-reported data on demographic information, family history of gastrointestinal diseases, and dietary habits.
Serum Sampling
After an overnight fast from 9 p.m. to 7 a.m., 5 mL of blood was collected by an experienced medical staff member. After centrifugation, the serum was extracted and stored at -70°C for further detection.
Detection of Serum Pepsinogen I, Pepsinogen II, Gastrin-17, and Helicobacter pylori Antibody
Serum PG I, PG II, G-17, and H. pylori antibody were measured with ELISA kits (Biohit Group, Helsinki, Finland). Catalog no. 601 010.01CN, 601 020.02CN, 601 035CN, and 601 040.03CN were used to test for PG I, PG II, G-17, and H. pylori antibody, respectively.
Stratification of Variables
Subjects were divided into 3 age groups: young (30 to 44 years), middle-aged (45 to 59 years), and older (≥60 years). A food frequency questionnaire was used to collect data on diet. Answers for each food item were collected as never or seldom (≤1 time/wk), sometimes (2 to 6 time/wk), or regularly (≥7 time/wk). Following the manufacturer’s instructions, a H. pylori antibody level above 30 enzyme immuno units was defined as H. pylori positive. In addition, a PG I, PG I:II ratio, and G-17 concentration of <30 μg/L, <3, or <2 pmol/L / >10 pmol/L, respectively, were considered abnormal.
Statistical Analysis
Epidata 3.1 (EpiData Association, Odense, Fyn, Denmark) was used for dual inputting of questionnaire data to test for parallel consistencies and ensure accuracy. SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) was used all statistical analyses. Rank-sum tests were used to analyze quantitative and ranked data. chi-squared tests were used to analyze categorical data. For all tests, a p<0.05 was considered statistically significant.
RESULTS
Demographic Information
In total, 231 subjects were recruited from Nanjing, including 136 males (58.9%) and 95 females (41.1%), and the average age among all subjects was 49.5±9.9 years old. In Minqing, 224 subjects were recruited, including 117 males (52.2%) and 107 females (47.8%), and the average age was 50.2±10.0 years old for the total population. No significant differences were found for the ratio between genders or average ages between Nanjing and Minqing.
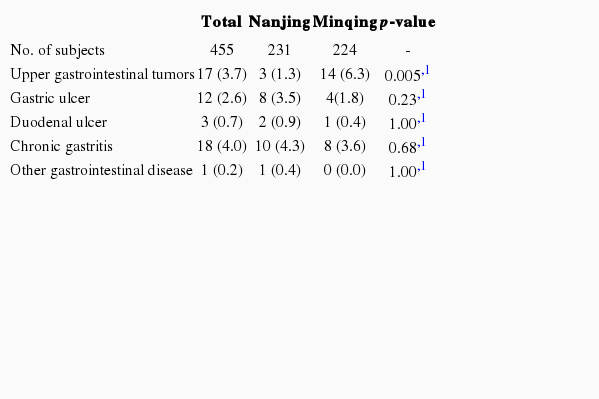
Family History
As shown in Table 1, the analysis of family history data indicated that the percentage of the subjects with a first-degree relative (parents, grandparents, brothers, or sisters) who had been diagnosed with an upper gastrointestinal tumor (esophagus cancer, gastric cancer, liver cancer, etc.) was significantly higher in Minqing than that in Nanjing (6.3% vs. 1.3%, p=0.005).
Dietary Habits
Kelp, tea, fruits, vegetables, ginger, lean meat, and lardo were more frequently consumed in Nanjing than in Minqing (p<0.05). However, pickles, processed meat, processed fish, and fish sauce were more frequently consumed in Minqing than in Nanjing (p<0.05). The proportion of subjects who reported smoking cigarettes was higher in Nanjing than that in Minqing (p=0.004) (Table 2).
Helicobacter pylori Infection
The H. pylori infection rate in Minqing (62.1%) was significantly higher than that in Nanjing (48.1%, p=0.003). Furthermore, the H. pylori infection rates among females and those aged between 45 to 59 years in Minqing were significantly higher than their counterparts in Nanjing were (p<0.05) (Table 3).
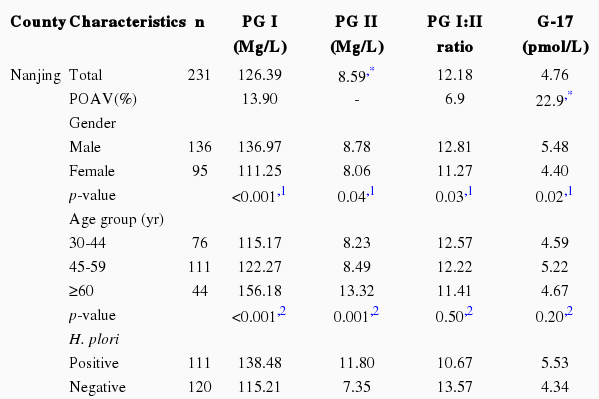
Serum Pepsinogen I, Pepsinogen II, the Ratio of Pepsinogen I:II, and Gastrin-17
The proportion of subjects with an abnormal serum PG II or G-17 concentration in Minqing was significantly higher than that in Nanjing (p<0.05); however, PG I and the ratio of PG I:II were not significantly different between Nanjing and Minqing. PG I, PG II, the PG I:II ratio, and G-17 did not significantly differ between the two counties among age and sex-specific groups. Regardless of whether the subject lived in Nanjing or Minqing, all subjects with an H. pylori infection had a significantly higher PG I, PG II, and G-17 serum concentration than those without an H. pylori infection did (p<0.05). However, subjects with an H. pylori infection had a significantly lower ratio of PG I:II than those without an H. pylori infection did (p<0.05) (Table 4).
DISCUSSION
Although Nanjing and Minqing are both inland areas in Fujian sharing similar general demographics, the adjusted mortality rate of gastric cancer in Minqing was much higher than that in Nanjing. Moreover, the prevalence of gastric cancer might be higher in Minqing than that in Nanjing; however, these data were not available. Our results indicate that family history of upper gastrointestinal tumors, certain dietary habits, H. pylori infection rates, and the concentrations of serum PG I, PG II, G-17, and the PG I:II ratio significantly differed between these two counties.
Previous studies have indicated that family history is an important risk factor for developing gastric cancer, with odds ratios (OR) of 2 to 3 among subjects with a first-degree relative who had been diagnosed with a gastrointestinal neoplasm [11-13]. Recent research from South Korea also reported an adjusted OR for gastric cancer of 2.85 (95% confidence interval, 1.83 to 4.46) among subjects with a first-degree relative with gastric cancer [14]. In our study, Minqing had more patients with a family history of upper gastrointestinal tumors in a first-degree relative than Nanjing did (p=0.005), which might be one of the reasons for the higher risk of developing gastric cancer in Minqing than that in Nanjing.
Our data showed that the consumption of vegetables, fruits, tea, kelp, ginger, and fresh meat was significantly more frequent in Nanjing than in Minqing (p<0.05). Vegetables and fruits are rich in vitamin A, C, and E. Vitamins, especially vitamin C, has a strong antioxidant effect, which can enhance the immune system and prevent gastric mucosa from lesions and necrosis [15]. Tea is rich in polyphenols, a kind of phytochemical that contains the epigallocatechin-3-gallate antioxidant for free radical inhibition and scavenging. An investigation conducted in the northern Kyushu region of Japan showed that people who frequently drank tea had a significantly lower incidence of gastric cancer than that of their counterparts [16]. A case-control study showed that drinking green tea might reduce the risk of gastric cancer, with a decreased adjusted OR of 0.42 (95% confidence interval, 0.32 to 0.55). In addition, the potential protective effect of green tea might be enhanced in a dose-response relationship with prolonged consumption [17]. Kelp contains three polysaccharides including algin, fucoidan, and laminaran [18]. All of these polysaccharides have a strong anti-tumor effect that has not only been found to directly inhibit the growth of tumor cells but also enhance the immune system to indirectly inhibit the growth and proliferation of cancer cells. Ginger might also have a similar anti-oxidative and anti-tumor effect [6,19,20]. Fresh meat is rich in protein, which can improve the ability to repair gastric mucosal injuries, but a high intake of meat and animal fat is considered a risk factor for gastric cancer [21]. Therefore, the impact of fresh meat consumption on gastric cancer requires further investigation.
Our study indicates that the consumption of processed fish, processed meat, fish sauce, and pickles containing abundant nitro compounds and salt was significantly more frequent in Minqing than in Nanjing. Nitro compounds include N-nitrosoamines and N-nitrosamides, which are strong carcinogens. In one study performed in Wuwei city, Gansu province, China, where there is a high incidence of gastric cancer, nitrate, nitrite, dimethylnitrosamine and diethylnitrosamine were detected in the pickles, which are the local residents’ winter vegetable substitute [22]. The study by Yu et al. [23] showed that fish sauce was one of the risk factors of incident gastric cancer in Fujian province. Salt itself has no carcinogenic effects; however, after ingesting a high concentration of salt, the gastric mucosa may be directly damaged by the resultant high osmotic pressure. If this pressure continues to develop, the chronic effects of a high-salt diet would greatly increase the risk of carcinogenesis. Since 1985, 12 studies on the relationship between salt intake and gastric cancer have been conducted in China, Japan, Italy, France, the United Kingdom, and the United States (2876 cases of gastric cancer and 8516 controls) [24]. All of these results indicate that a high salt intake is a risk factor for developing gastric cancer with relative risks between 1.4 and 6.2.
H. pylori infection is a major cause of chronic gastritis and stomach ulcers as well as an important risk factor for developing gastric cancer. In China, the H. pylori infection rate in the general population is approximately 40% to 90%, with an average of 59% [25]. The World Health Organization has classified H. pylori infection as a Class I carcinogen for the development of gastric cancer [26]. In our study, the H. pylori infection rate in Minqing was significantly higher than that in Nanjing, which might have contributed to the higher prevalence of gastric cancer in Minqing than that in Nanjing.
In recent years, serum PG I, PG II, G-17, and the ratio of PG I:II have proved to be reliable, non-invasive serum markers reflecting atrophy of the gastric mucosa [27,28]. Studies have reported that the risk for developing gastric cancer is up to 90-fold higher in patients with gastric atrophy than that among people without gastric atrophy [29]. Thus, gastric cancer incidence may be serologically monitored by collecting data on the status of the gastric mucosa. In our study, the concentration of PG II was significantly higher in Minqing than that in Nanjing, but PG I, the ratio of PG I:II, and G-17 were not significantly different. Furthermore, the percentage of subjects with abnormal G-17 was significantly higher in Minqing than that in Nanjing, which suggests those living in Minqing have a higher risk for developing gastric atrophy than those living in Nanjing do. Moreover, subjects with H. pylori infection had significantly higher concentrations of PG I, PG II, and G-17 than subjects without infection did. The ratio of PG I:II was significantly lower in subjects with an H. pylori infection than that among subjects without the infection, thus having an H. pylori infection might impact the secretion of gastric glands.
In conclusion, residents in Minqing have a higher prevalence of upper gastrointestinal tumors among their first-degree relatives, more unhealthy dietary habits, a higher H. pylori infection rate, and a higher proportion of abnormal serum G-17 than those living in Nanjing do. These reasons might explain the increased risk for developing gastric cancer in Minqing relative to that in Nanjing. This study also suggests that the concentration of PG I and II as well as G-17 might be associated with the H. pylori infection rate. The main limitation of this study was our small sample size. Further investigations on large populations are needed.
ACKNOWLEDGEMENTS
This study was supported by a grant from the Ministry of Health in China and the Bureau of Health in Fujian (no. WKJ-FJ-18).
Notes
The authors have no conflicts of interest with the material presented in this paper.