The Association Between Serum Albumin Levels and Metabolic Syndrome in a Rural Population of Korea
Article information
Abstract
Objectives
A positive association between serum albumin levels and metabolic syndrome has been reported in observation studies, but it has not been established in the Korean population. The purpose of this study was to evaluate the association between serum albumin levels and the presence of metabolic syndrome among a sample of apparently healthy Korean adults.
Methods
This cross-sectional study analyzed data of 3189 community-dwelling people (1189 men and 2000 women) who were aged 40 to 87 years and were living in a rural area in Korea. Serum albumin levels were classified into quartile groups for each sex. Metabolic syndrome was defined according to the National Cholesterol Education Program Adult Treatment Panel III guidelines with an adjusted waist circumference cut-off value (≥90 cm for men and ≥85 cm for women). An independent association between serum albumin levels and metabolic syndrome was assessed by multiple logistic regression analysis.
Results
Higher serum albumin levels were associated with increased prevalence of metabolic syndrome. The odds ratio (95% confidence interval) of the prevalence of metabolic syndrome for the highest versus the lowest serum albumin quartiles was 2.81 (1.91 to 4.14) in men and 1.96 (1.52 to 2.52) in women, after adjusting for age, smoking status, alcohol consumption, and physical activity. When each metabolic abnormality was analyzed separately, higher serum albumin levels were significantly associated with hypertriglyceridemia and hyperglycemia in both sexes, and with abdominal obesity in men.
Conclusions
These results suggest that higher serum albumin levels are positively associated with an increased risk of metabolic syndrome in Korean adults.
INTRODUCTION
Serum albumin level is a marker of nutritive conditions, acts as an antioxidant, and is a plasma volume expander [1-3]. In some studies, lower serum albumin has been regarded as an indicator of malnutrition, inflammation, and liver disease [4], and has been reported to be associated with increased cardiovascular disease morbidity and mortality [4-6]. Meanwhile, other studies have not observed significant associations between lower serum albumin and carotid atherosclerosis [7,8]. Another study observed an association between low serum albumin and coronary heart disease only in current smokers, but not in never or former smokers [9]. On the other hand, higher serum albumin levels are linked to cardiovascular risk factors including blood pressure and cholesterol levels [4,5,10]. In addition, some studies have reported positive associations between serum albumin levels and metabolic syndrome [11,12], the latter of which is a clustering of multiple cardiovascular risk factors [13,14].
However, the association between serum albumin levels and metabolic syndrome has not been established for the Korean population. Thus, we investigated the association between serum albumin levels and the prevalence of metabolic syndrome along with its components among a sample of apparently healthy Korean adults.
METHODS
I. Participants
We performed a cross-sectional analysis of baseline data of a community-based prospective cohort in Kangwha Island, South Korea. From 2006 to 2009, a total of 3600 people participated in the baseline health examination study. We excluded 411 participants for the following reasons: no fasting blood sample (n=15); no information about their smoking status and alcohol consumption (n=5); systolic blood pressure <60 mmHg or >300 mmHg and diastolic blood pressure <40 mmHg or >200 mmHg (n=5); triglycerides ≥400 mg/dL (n=85); history of cardiovascular disease or cancer (n=215); aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyl transferase (γ-GTP), or creatinine levels over the 99th percentile (n=101). Finally, 3189 participants (1189 men and 2000 women) were eligible for this study. All participants gave written informed consents, and the study protocol was approved by the Institutional Review Board.
II. Data Collection
The participants' age, sex, smoking status, alcohol consumption, physical activity, and medical history were collected using a standardized questionnaire. The anthropometrics including height, weight, and waist circumference were measured. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Waist circumference was measured midway between the inferior margin of the last rib and the iliac crest in a horizontal plane. Blood pressure was measured twice by an automatic sphygmomanometer (Dinamap 1846 SX/P; GE Healthcare, Waukesha, WI, USA) with the participant in the sitting position after resting for at least 5 minutes. If the difference between each measurement was more than 10 mmHg, a third measurement was performed. The mean value of the last two measurements was used for the analysis. Blood samples were taken after at least an 8-hour fast. Serum levels of total protein, albumin, creatinine and γ-GTP were measured by colorimetric methods using automatic analyzers. Serum C-reactive protein (CPR) was measured by the turbidimetric immunoassayassay. AST, ALT, glucose, total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides were measured by enzymatic methods. Low-density lipoprotein (LDL) cholesterol was calculated using the Friedewald' formula [15]. Hemoglobin A1c was measured by a high-performance liquid chromatographic method using a commercial kit. Fasting plasma insulin was measured by radioimmunoassay using a commercial kit. The measure for insulin resistance, the homeostasis model assessment of insulin resistance (HOMA-IR), was calculated as fasting insulin (µU/mL)×fasting glucose (mg/dL)/405 [16].
III. Definition of Metabolic Syndrome
Metabolic syndrome was defined according to the guidelines of the National Cholesterol Education Program Adult Treatment Panel III [17] with adjustment for the waist circumference cut-off value [18]. Metabolic syndrome was diagnosed for participants that had any three of the following five features: waist circumference ≥90 cm in men and ≥85 cm in women; triglycerides ≥150 mg/dL or on drug treatment for elevated triglycerides; HDL cholesterol <40 mg/dL in men or <50 mg/dL in women or on drug treatment for reduced HDL cholesterol; systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg or on hypertensive drug treatment in a patient with a history of hypertension; fasting glucose ≥100 mg/dL or on drug treatment for elevated glucose.
IV. Statistical Analyses
The mean values of the risk factors for cardiovascular disease including blood pressure, cholesterols, and fasting glucose were computed by quartiles of the serum albumin level. Linear trends in these risk factors were tested according to the serum albumin quartiles. Trends for skewed variables were evaluated using a nonparametric trend test. Spearman correlation analyses were performed to assess the correlation between serum albumin levels and other clinical characteristicts. Logistic regression analysis was performed to assess the association of serum albumin levels with metabolic syndrome and also with each metabolic syndrome component. Logistic regression analysis was performed with and without adjustment for age, body mass index, smoking status, alcohol consumption, and physical activity. All statistical analyses were performed with the SAS version 9.2 (SAS Inc., Cary, NC, USA). All tests were two-sided and performed at a 5% significance level.
RESULTS
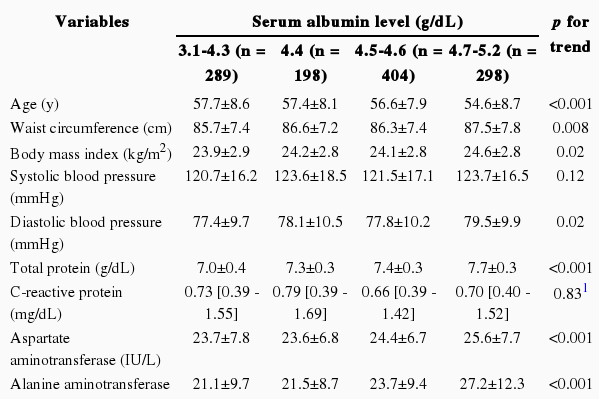
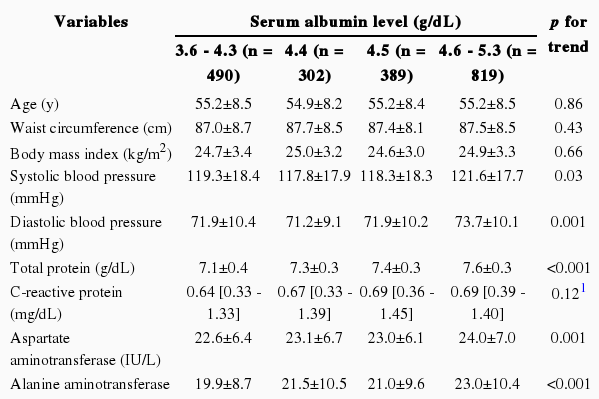
Characteristics of the study participants are shown according to the serum albumin quartiles. The participants' age ranged from 40 to 87 years, with a mean age of 55.7 years. Cut-off levels for the quartile groups were different for men and women. Thus the analyses were performed separately for men and women (Tables 1 and 2).
Among the 3189 participants, a higher serum albumin quartile level was significantly related to higher diastolic blood pressure, total cholesterol, fasting glucose, and HOMA-IR. We calculated the Spearman' correlation coefficients (ρ) to assess the relationship between serum albumin levels and each cardiovascular risk variable (Table 3). Serum albumin levels showed a significant (p<0.05) correlation with systolic blood pressure, diastolic blood pressure, total cholesterol, LDL cholesterol, triglycerides, fasting glucose, hemoglobin A1c, HOMA-IR (in men and women), age, waist circumference, and BMI (in men).
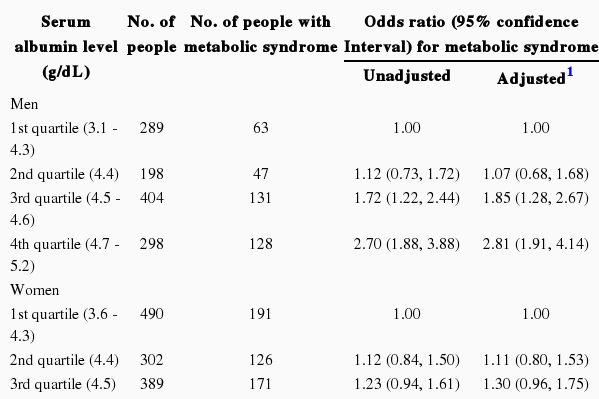
Table 4 shows the association between serum albumin quartiles and metabolic syndrome. Men with the third and fourth quartile of serum albumin levels, and women with the fourth quartile of serum albumin levels had a significantly higher prevalence of metabolic syndrome than those with the lowest quartile. Adjustment for age, BMI, smoking status, alcohol consumption and physical activity did not affect these associations.
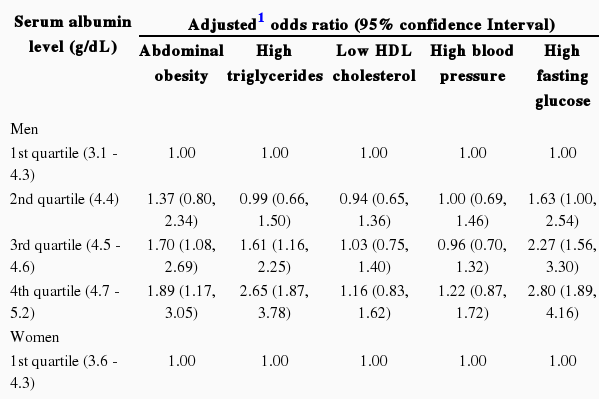
We also investigated associations between serum albumin quartiles and each of the components of metabolic syndrome in men and women, after adjusting for potential confounders (Table 5). Men with the third and fourth quartiles of serum albumin levels had a significantly increased prevalence of abdominal obesity, hypertriglyceridemia, and hyperglycemia. Women with serum albumin levels in the fourth quartile had an increased prevalence of hypertriglyceridemia and hyperglycemia, but women in the third quartile had an increased prevalence of hypertriglyceridemia only.
DISCUSSION
This study showed a positive association between serum albumin levels and the prevalence of metabolic syndrome among a sample of apparently healthy Korean adults even after controlling for related covariates including age, BMI, smoking status, alcohol consumption, and physical activity. More specifically, serum albumin levels were significantly associated with abdominal obesity, hypertriglyceridemia, and hyperglycemia in men, and with hypertriglyceridemia and hyperglycemia in women. Our findings are consistent with the Japanese studies suggesting a positive association between serum albumin levels and the prevalence of metabolic syndrome [11,12]. On the other hand, other studies from UK and the US have reported that lower serum albumin levels were associated with an increased risk of cardiovascular disease incidence and mortality [4-6]. The inconsistency of these findings might be, at least in part, due to the different characteristics of the study participants. In our study participants, higher serum albumin levels were positively associated with most major cardiovascular risk factors including blood pressure, non-HDL cholesterol, hyperglycemia, and insulin resistance. However, in the Framingham Offspring Study, people with lower serum albumin levels had unfavorable cardiovascular risk profiles, such as higher BMI, total cholesterol, cigarette smoking, and low HDL cholesterol. The inconsistency between these study findings also might be due to different outcomes of interest. Many studies have reported that lower serum albumin levels increased cardiovascular disease incidence or mortality [4-6], but the association between serum albumin levels and carotid atherosclerosis has been inconsistent [7,8,11]. In addition, some studies have shown that higher serum albumin levels are linked to cardiovascular risk factors [4,5,10]. These inconsistent results suggest that low albumin levels might be a reflection of the inflammatory process rather than an independent risk factor of cardiovascular disease.
In our study, higher serum albumin levels were associated with the increased prevalence of abdominal obesity in men but not in women. Sex difference in the association between serum albumin and abdominal obesity can be partially explained by some mechanisms. It is known that women have a higher amount of subcutaneous abdominal fat and lower visceral abdominal fat than men, and that estrogen plays a role in this difference in fat distribution [19-22]. Albumin synthesis is stimulated by steroids hormones [23], and albumin acts as a carrier for steroid hormones [24]. Our study did not observe a correlation between serum albumin levels and CRP, while some previous studies have reported an association between low serum albumin levels and increased CRP [25,26]. Our study population was limited to a sample of relatively healthy individuals of Korea. Therefore, the association between serum albumin levels and CRP might be diminished.
The underlying mechanisms for the association between serum albumin levels and metabolic abnormalities are still unclear. However, it can be explained, at least in part, by dietary protein intake. Protein intake has a positive association with serum albumin levels [27-29], and high protein intake is accompanied by the stimulation of glucagon and insulin, high glycogen turnover, and increased gluconeogenesis [30]. Accordingly, a high protein diet was associated with an increased prevalence of diabetes [31,32]. Thus, overall, high protein intake can contribute to hyperinsulinemia, hyperglycemia, hypertension, and lipid abnormality, and in turn can contribute to the development of metabolic syndrome.
This study has the following limitations. First, we did not analyze the effects of dietary protein intake. Protein intake can be related to both serum albumin levels and metabolic syndrome; thus further studies are needed to establish the underlying mechanisms of this association. Second, we could not assess the causal relationship between serum albumin levels and metabolic syndrome because of the cross-sectional study design. Follow-up studies are merited to investigate the serum albumin levels as a prospective risk factor of metabolic syndrome. Finally, our analysis was based on a cohort study from one rural area and limited to relatively healthy individuals. The findings of our study may not be generalizable to the entire Korean population.
In conclusion, our findings suggest that higher serum albumin levels are positively associated with metabolic syndrome, probably through increased abdominal obesity, high fasting blood glucose, and triglycerides.
ACKNOWLEDGEMENTS
This study was supported by grants from the Korea Centers for Disease Control and Prevention (2006-E71011-00, 2008-E71004-00, and 2009-E71006-00) and a grant from the Korea Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A102065).
Notes
The authors have no conflicts of interest with the material presented in this paper.
This article is available at http://jpmph.org/.