The Socioeconomic Burden of Coronary Heart Disease in Korea
Article information
Abstract
Objectives
We aimed to estimate the annual socioeconomic burden of coronary heart disease (CHD) in Korea in 2005, using the National Health Insurance (NHI) claims data.
Methods
A prevalence-based, top-down, cost-of-treatment method was used to assess the direct and indirect costs of CHD (International Classification of Diseases, 10th revision codes of I20-I25), angina pectoris (I20), and myocardial infarction (MI, I21-I23) from a societal perspective.
Results
Estimated national spending on CHD in 2005 was $2.52 billion. The majority of the spending was attributable to medical costs (53.3%), followed by productivity loss due to morbidity and premature death (33.6%), transportation (8.1%), and informal caregiver costs (4.9%). While medical cost was the predominant cost attribute in treating angina (74.3% of the total cost), premature death was the largest cost attribute for patients with MI (66.9%). Annual per-capita cost of treating MI, excluding premature death cost, was $3183, which is about 2 times higher than the cost for angina ($1556).
Conclusions
The total insurance-covered medical cost ($1.13 billion) of CHD accounted for approximately 6.02% of the total annual NHI expenditure. These findings suggest that the current burden of CHD on society is tremendous and that more effective prevention strategies are required in Korea.
INTRODUCTION
Over the past 3 decades, coronary heart disease (CHD) mortality has fallen by more than 50% in developed countries such as the United States, Canada, Australia, France, and Japan [1,2]. By contrast, recent trends have shown that CHD mortality has been rising in many developing or newly developed countries including Korea, China, India and other Asian countries [3]. Although the CHD mortality rate in Korea remains among the lowest in the world [4], it increased rapidly (by more than 5- to 6-fold) from 1983 to 2003 [5]. At present, CHD is one of the leading causes of death in Korea, and the age of CHD onset is conjectured to be younger among Koreans than in the past [6,7]. However, the emergence of CHD epidemics in these countries has attracted little concern and a limited public health response [1,8]. The lack of recognition of the seriousness of the CHD impact on individuals and society hinders the implementation of more vigorous prevention strategies. Although several studies of the cost-of-illness of CHD have been carried out in industrialized western countries [9,10], few studies have been done in Asian countries. A goal of this study was to estimate the socioeconomic cost of treating CHD in Korea in 2005. It is hoped that increased awareness and knowledge about the magnitude and components of economic burden of CHD in Korea would influence health policy makers to allocate more health care resources and to prioritize the prevention of CHD with other public health problems.
METHODS
Study Design
This was a population-based study designed to examine the economic impact of the CHD epidemic in Korea on individuals and society as whole. The economic consequences of CHD were estimated from a societal perspective using a prevalence-based approach, in which the costs of both incident (new) and prevalent (pre-existing) cases of CHD are measured within a population over a defined period of time [11]. This was a cost-of-treatment study, examining only the costs associated with treating CHD. This study adopted a top-down approach that estimated the average cost of treatment for individual patients based on the national data. To understand the differences in cost patterns according to subtypes of CHD, we performed separate cost estimation for angina pectoris and myocardial infarction (MI), the most prevalent CHD subtypes in the Korean population.
Study Cohort and Data Sources
We used the electronic administrative claims records of the Korean National Health Insurance (NHI) and Medical Aid (MA) program as a major data source to identify study cohorts of patients with CHD, angina, or MI, and to track health care services provided to patients to treat these conditions during 2005. As a mandatory government-run program, the NHI and MA claims database contains all medical and prescription drug claims for insurance-covered services provided to the entire population.
Individuals (N=959 037) aged 20 years or older were included in the study cohort if they had at least one insurance claim record with a primary or secondary diagnosis of CHD (International Classification of Diseases, 10th revision (ICD-10) codes of I20-I25) during 2005. Ten thousand and two claims were excluded if they had at least one claim containing a diagnosis of cancer (ICD-10 code: C00-C97), because treatments for this condition are associated with extremely high expenditures. CHD-related claims, defined as those with a primary or a secondary diagnosis of CHD, were extracted for each subject and aggregated to produce patient-level information on the total CHD-related healthcare utilization and cost. The same methods were used to identify the study cohorts of CHD subtypes, using ICD-10 codes of I20 for angina and I21-I23 for MI [12,13]. After cleansing the data sets, we obtained information on 956 191 patients from 3 741 848 claims for CHD. During the year of 2005, there were 307 935 claims included as CHD for one outpatient visit. The number of CHD patients according to diagnosis categories after cleansing the data sets is provided in Table 1. The information on other costs not included in the NHI database was obtained from the Korean National Statistics office and from the 2001 and 2005 Korean National Health & Nutritional Examination Survey (KNHANES) [14]. To estimate the indirect cost, we obtained data from the Korean National Statistical Office and from the Ministry of Labor [15,16].
Cost Estimation and Data Analysis
The total economic cost of CHD includes direct and indirect costs. In this study, direct costs included medical costs and transportation costs. Indirect costs consisted of lost opportunity due to morbidity and premature death and informal care costs. We estimated the average per-capita costs and the total national costs for treating CHD, angina, and MI during 2005 by gender and by 5-year age grouping. All costs were expressed in 2005 monetary value.
Direct Costs
Direct costs include direct medical costs and transportation costs spent to visit healthcare providers. Direct medical costs were estimated from spending on inpatient care, outpatient care, and prescription costs. The NHI and MA claims data are limited in that they provide only information on the medical costs for insurance-covered services. Therefore, medical costs for non-covered services were estimated on the basis of a published report on the proportion of uninsured medical costs to the total medical costs spent to treat CHD, which was measured using medical bills from selected hospitals in Korea in 2005 [7]. The average proportion of uninsured costs for hospital admission and outpatient visits associated with CHD was estimated as 26.1% and 9.3%, respectively.
Transportation cost was calculated by multiplying the average round-trip transportation cost to healthcare institutions by the total number of CHD-related visits or admissions per year. The average round-trip cost ($18.6 for an outpatient visit and $23.6 for a hospital admission, using an exchange rate of ₩1024 for $1) was obtained from the 3rd KNHANES in 2005. Considering that most elderly patients in Korea visit hospitals with a caregiver, transportation costs for a caregiver were added for patients aged 65 years and older.
Direct costs=medical costs (MC)+transportation costs (TC)

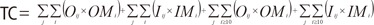
i= 1 if 20-24 years old, 2 if 25-29 years old, ..., 14 if 85 or over
j= 1 if male, 2 if female
α= proportion of uninsured costs among the total medical costs for inpatient care
β= proportion of uninsured costs among the total medical costs for outpatient care
Eij= insured medical costs for inpatient care
OEij= insured medical costs for outpatient care
Mij= prescription drug costs
Oij= number of outpatient visits
Iij= number of hospital admissions
OMij= average transportation cost for an outpatient visit
IMij= average transportation cost for a hospital admission
Indirect Cost
The indirect costs were calculated as productivity losses by patients and caregivers. According to the human capital approach, the monetary value of opportunity costs for CHD morbidity and mortality was quantified as productivity loss due to absence from work caused by hospitalization and outpatient visits as well as premature death [17]. Productivity loss due to CHD-related morbidity was calculated by multiplying the average daily or hourly wage by days of hospitalization or hours spent in outpatient visits (assumed as one third of the day) attributable to CHD [18,19]. Premature death costs were the expected value of an individual's future earnings during the potential years of life lost (PYLL) [15], which was defined as a discrepancy between the life expectancy and the age of death as obtained from the Korean life table [20]. The monetary value of the future income loss for the period after 65 years of age was counted as zero, because Korean people generally retire from work at age 65. Expected future earnings were discounted by 5% annually to reflect the present value of future productivity [21]. Sensitivity analysis was conducted with a relaxed assumption on the productivity loss due to premature death from CHD over 65 years of age.
The opportunity cost for informal caregivers' time spent to take care of patients with CHD was estimated to be a product of days in hospitalization or hours spent for outpatient visits attributable to CHD and the average daily wage ($55.48) of women aged 20 to 50 years. This is based on the fact that, in Korean culture, in general, young female family members serve as primary caregivers when family members are sick. Considering that most elderly patients in Korea visit the hospital accompanied by a caregiver, one third of the opportunity cost for a caregiver was added to outpatient visits for those over 65 years old.
Indirect costs=productivity loss due to morbidity (PL)+informal caregiver costs (IF)+premature death costs (PD)

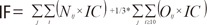
i=1 if 20-24 years old, 2 if 25-29 years old, ..., 14 if 85 or over
j=1 if male, 2 if female
Nij=days in hospitalization
δ= non-productivity rate of outpatient care compared to inpatient care
Oij=number of outpatient visits
Pij=proportion of population being economically active,
yij=average daily earning
IC=average daily informal care costs
t=age of death
τ=number of years after death till 65 years
Fij=number of deaths
Yjt+τ=average yearly earning at t+τ
γ=discount rate
RESULTS
Treated Prevalence of Coronary Heart Disease
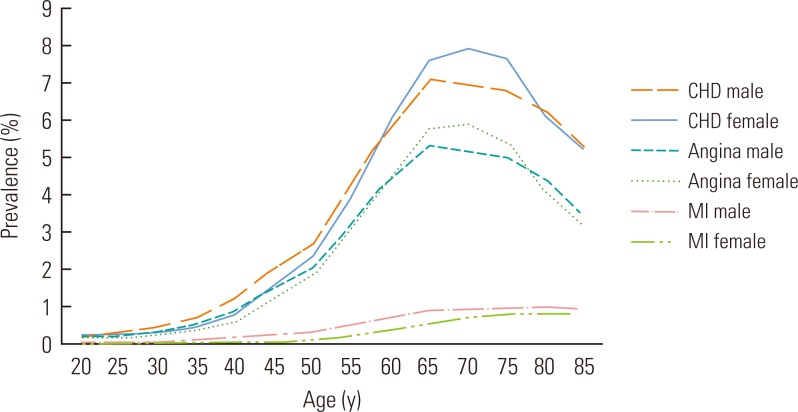
The total adult population aged 20 years or older diagnosed with and treated for CHD during 2005 was 959 037 (462 231 men and 496 806 women), and the treated prevalence of CHD among adults aged 20 years or older was 2454 per 100 000 (Table 2). Figure 1 presents the overall age- and gender-specific treated prevalence of CHD, angina, and MI among the adult Korean population. The proportion of the adult population with CHD, angina, or MI was estimated to be 2.45% (male, 2.38%; female, 2.53%), 1.83% (male, 1.78%; female, 1.88%), and 0.26% (male, 0.31%; female, 0.20%), respectively. Overall, women showed a higher prevalence of CHD and angina than men, whereas men had a higher prevalence of MI. For both CHD and angina, the prevalence peaked sharply and then declined between the ages of 65 and 69 in men and 70 and 74 in women. On the other hand, the prevalence of MI increased steadily with age.
Total National Costs
The total national costs of CHD are provided in Table 3. Overall, the annual economic burden of CHD imposed on Korean society was estimated to be $2.52 billion in 2005. Medical cost was the largest component of CHD-related costs, at $1.3 billion (53.3%), followed by productivity loss due to morbidity and mortality (33.6%), transplantation cost (8.1%), and informal caregiver cost (4.9%) (Figure 2).
The total national costs associated with angina and MI were $1.1 billion and $954 million, accounting for 45.2% and 37.9%, respectively, of the total CHD-related costs (Figure 2). A substantial discrepancy existed in the distribution of cost across different cost components between the two subtypes of CHD. For example, medical cost was the predominant cost of treating angina, making up 74.3% ($846 million) of the total cost, including 23.3% for inpatient care and 51.0% for outpatient care, and the cost of productivity loss due to premature death made up the smallest portion ($26.6 million, 2.3%). On the other hand, premature death cost was the largest cost component for patients with MI ($638 million, 66.9%), while medical costs associated with inpatient and outpatient care accounted for 27.9% ($266.3 million) only.
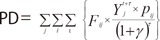
Figures 3 and 4 showed the distribution of the total national direct and indirect costs for each diagnostic category of CHD by age and by gender. Direct costs for CHD, angina and MI, showed similar patterns in men and women in that they peaked and then declined between the ages of 65 and 74, while indirect costs for men were much higher than for women across age groups.
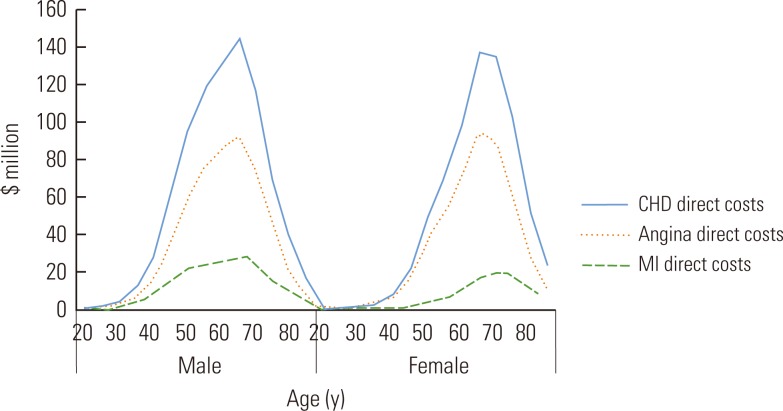
Direct costs of coronary heart disease by age and sex, Korea, 2005. Direct costs include direct medical cost (inpatient care, outpatient care, and prescribed drug treatment) and transportation cost. CHD, coronary heart disease; MI, myocardial infarction.
Per-capita Cost
Table 4 presents annual per-capita health care utilization and costs for treating CHD, angina and MI by age and gender in Korea in 2005. The average annual cost of CHD per patient was $1835, and was comprised of 76.6% for medical costs, 11.6% for transportation costs, 7.0% for informal care costs, and 4.8% for productivity loss due to morbidity.
Because the NHI claims data do not provide information about death for individuals, we couldn't include productivity loss cost due to death for person-level data. Therefore, cost of premature death was not included in estimates of per-patient cost. It was included in the estimation of the total national costs, however, by adding the product of the age-and gender-specific total number of CHD deaths provided by the National Mortality Statistics and the estimated future earnings lost due to premature death from CHD across age and gender groups. Direct costs, productivity loss due to morbidity, and informal care giver costs were estimated based on the claims of patients who had been treated for CHD in 2005. The cost per patient for these categories, excluding premature death costs, was estimated by dividing by the number of CHD treated patients in 2005.
The annual per-capita cost of treating angina excluding premature death cost was $1556, and was comprised of 76.1% for medical care costs, 12.7% for transportation costs, 6.3% for informal care costs, and 4.8% for productivity loss due to morbidity. The annual per-capita cost for MI was $3183, which was about 2.0 times higher than the cost for angina. Compared to angina, the proportion of costs for MI occupied by medical care is higher (84.4% vs. 76.1%) and consequently the other cost components made up a relatively smaller proportion of the total cost (4.2% for transportation costs, 7.2% for informal care costs, and 4.2% for productivity loss due to morbidity).
Sensitivity Analysis
For the base case analysis, we applied no productivity loss for the remaining life expectancy after the age of 65 with a result in total premature death costs of $764 million, $27 million, and $638 million for CHD, angina, and MI, respectively. When we applied one half of the annual income of the age group of 60 to 64 years to the remaining life expectancy after the age of 65 years, the estimated premature death costs rose to $1153 million, $54 million, and $945 million for CHD, angina, and MI, respectively. The cost of productivity loss, according to CHD premature death, was $911.1 million with a 3% discount rate, and $646.3 million with a 7% discount rate. The cost of productivity loss, according to angina premature death, was $30.6 million with a 3% discount rate, and $23.4 million with a 7% discount rate. The cost of productivity loss, according to MI premature death, was $761.9 million with a 3% discount rate, and $540.5 million with a 7% discount rate.
DISCUSSION
The present study is the first attempt to estimate the economic burden of overall CHD, angina and MI in Korea using a national database. The estimated socioeconomic cost of CHD is $2.5 billion, which is equivalent to approximately 0.32% of the gross domestic product ($791.5 billion) of Korea in the same year (Table 5). The total insurance-covered medical cost ($1.13 billion) of CHD accounts for approximately 6.02% of the total annual NHI expenditure ($18.82 billion in Korea in 2005). It is worthwhile to compare the cost of CHD to the cost of other diseases to help understand the relative economic impact of CHD.
The socioeconomic costs for each of the 5 leading causes of death in Korea in 2001 were reported as follows: ₩5595 billion ($5.5 billion) for malignant neoplasm, ₩1941 billion ($1.8 billion) for liver disease, ₩1775 billion ($1.7 billion) for cerebrovascular disease, ₩1510 billion ($1.5 billion) for heart disease, and ₩971 billion ($0.95 billion) for diabetes [22]. According to previous studies, the socioeconomic burden of stroke in our country for 2005 was approximately ₩3.737 trillion [23], while economic costs related to cancer were estimated to be ₩14.1 trillion [24]. In regards to cancer, the death cost was ₩7.4 trillion (52.6%), which formed a greater portion of the disease burden, but in regards to CHD, the medical costs were estimated to form the largest part, with ₩1.3 trillion (53.3%).
These results confirm that the current economic burden of CHD in Korea is substantial and suggest that the prevention of CHD may need to be the priority for health care intervention in Korea. Prevention strategies should include both public health and clinical approaches, target both the general population and high-risk groups, and integrate population-based risk modification and cost-effective management strategies for individuals [1,25].
In Great Britain and the European Union, the dominant direct medical cost for CHD was inpatient care [26]. In Korea, however, it was outpatient care, probably due to the high prevalence of angina, which is mainly treated on an outpatient basis. For angina, medical cost for outpatient care was the largest cost component, at $580.5 million (51%) (Figure 2), whereas lost earnings due to premature death ($638.3 million [66.9%]) was the largest cost in the treatment of MI. When the CHD expenditures of OECD nations in 1999 were examined, the employment/informal care costs formed a larger part than the direct care costs in the United Kingdom, Switzerland, and Canada. On the other hand, direct care costs formed a larger part than the employment/informal care costs in Sweden and Germany. According to the CHD cost estimation results of the United Kingdom in 2004, the informal care costs from professional caregivers were valued at £1013 million, which accounts for nearly half of the hospital inpatient care costs of £2425 million, creating a large burden [27].
Increasing mortality trends in young adults have occurred in the United States from 1980 to 2002 despite the wide use of evidence-based therapies such as angioplasty, thrombolysis, and various medications [28]. Increased premature death rates due to CHD in a relatively younger population in Korea would erode the national economy due to the loss of work force [6]. This suggests that strong public health actions are needed to change lifestyle behaviors and to control the various risk factors associated with CHD [28]. The average annual per-capita costs of patients with CHD, angina or MI excluding mortality costs were $1835, $1556, and $3183, respectively. The difference in per-capita costs between angina and MI may be attributable to the difference in the length of hospital stays (8.5 days vs. 12.1 days), duration of follow-up outpatient visits, drug prescription frequency, and intensity of diagnostic tests and therapeutic measures. Patients with acute MI are more likely to require emergency medical care, surgical care, and hospitalization compared to patients with stable angina. These findings are similar to previous findings that emergency medical costs, initial hospitalization rates, and readmission costs are higher in patients with acute MI than those with stable angina in the United States [29].
Regardless of the subtype of CHD, per-capita costs were consistently greater among men than women because of higher levels of indirect and direct costs in men across the age groups. Since most of the studies calculate indirect costs based on the human capital approach, higher indirect costs for men can be explained by higher wage rates for men. The human capital approach method usually assesses a loss of productivity with a loss of labor workforce. This approach is limited in that it can underestimate the value in productivity reduction according to the domestic work and unofficial nursing care [30]. Compared to males, the economic participation of females is lower, thus, that production loss of domestic workers, which is not included in the estimation, can be an important cause for the considerable underestimation of the loss in the female production costs compared to males.
On the other hand, higher direct costs for men to treat the same type of CHD might be explained by various factors. Several studies from other countries have also reported gender differences in the prevalence, medical and surgical treatment rates, prognosis and manifestation of cardiovascular disease [31]. Similar to the results of a meta-analysis of international variations across 31 countries, women were found to have a 10% higher treated prevalence of angina than men [32]. In the Framingham study, it was shown that women who had angina generally had a good prognosis, whereas angina in men more often led to MI [33]. However, the biological, economical, and socio-cultural factors for these gender differences are not well-known yet [31], and further studies are needed to find the reasons for gender discrepancies in Korea.
This research made use of the claim data of the entire nation to estimate the disease costs of CHD, angina, and MI disease, which are anticipated to increase in occurrence gradually in our country. Due to the characteristics of the disease, where there are many cases where it is included as a secondary diagnosis, estimations included the burden of the 1st secondary diagnosis as well as the primary diagnosis, so it can be used as a reference when distributing medical resources. Also, this research estimated the uninsured medical costs by applying the uninsured medical costs ratio according to the disease and type of medical institution. It is difficult to estimate an accurate uninsured cost value, but it can be a basis for understanding the rough scale of the costs.
This study had several limitations. First, there was difficulty in confirming the accuracy of the diagnoses, since the analyzed data was not derived from clinical settings, but from claims data. However, a validation study performed in Korea compared the diagnoses derived from the NHI claims database to actual diagnoses in patients' medical records. For 2003, the overall positive predictive value of the diagnoses was reported to be 81.8% in the case of inpatients [34]. Therefore, we believe that, overall, the prevalence rates of CHD based on the NHI claims data are likely to be an approximation of the true rates. Second, this insurance claims-based study limited our access to information such as disease severity, co-morbid conditions, past history and specific treatment. Third, a portion of estimated socio-economic cost has been underestimated, since intangible (psycho-social) costs were not evaluated. When patients are accompanied with cancer, stroke, high blood pressure, diabetes, or hyperlipidemia, CHD can be recorded as a secondary diagnosis in the clinical scene. This study regarded CHD patients as those who had CHD as their primary diagnosis, as well as those who received one occurrence of medical treatment in the clinic for CHD as their 1st secondary diagnosis. Therefore, in cases including patients who were confirmed to be none CHD patients, there is a possibility that the medical cost was overly estimated. However, in order to reduce the possibility of overestimation, claims of CHD after the 1st secondary diagnosis, cases with accompanying cancer, and claims with medical costs over one billion won were excluded from the estimation. In future studies, there is a need to estimate a more accurate CHD burden through the consideration of detailed procedures, surgery related to CHD, or the administration of medications, as in the previous studies of Europe and the United States.
According to a 2008 report on European Cardiovascular Disease statistics, the percentages of total health care expenditure due to CHD for primary care, outpatient care, inpatient care, emergency care and medications were estimated to be 2.70% in the United Kingdom, 3.20% in Germany, 3.08% in the Czech Republic, and 2.05% in Hungary in 2006 [35]. It was estimated to be 2.83% of the total health care expenditure in Korea during 2005. It is meaningful that the percentages of the health care cost of CHD were not much different to those of European countries. It implies that Korean society shoulders an enormous economic burden comparable to those in developed countries and more effective prevention strategies are required.
In summary, the annual total national costs of CHD, angina, and MI in Korea were estimated to be $2.52 billion, $1.1 billion, and $954 million in 2005, respectively. Our study results provide strong evidence of the need to develop national policy to effectively prevent CHD in Korea. We found that angina and MI, which are subsets of CHD, have different distribution patterns of per-patient and societal cost of disease treatment according to gender and age. Better preventive policies for CHD can be instituted with a more accurate predictable outcome when CHD is subdivided into angina and MI and when disease-specific cost factors are estimated according to sex, age, and per-patient cost. It is our hope that an increased awareness of the magnitude and specific components of the economic burden of CHD in Korea will influence health policy makers to allocate more health care resources to CHD and to prioritize its prevention.
ACKNOWLEDGEMENTS
Financial support for this study was provided by the Korea Ministry of Health, Welfare, and Family.
Notes
The authors have no conflicts of interest with the material presented in this paper.