Epidemiological Investigation of an Outbreak of Hepatitis A at a Residential Facility for the Disabled, 2011
Article information
Abstract
Objectives
An outbreak of hepatitis A occurred at a residential facility for the disabled in July 10, 2011. This investigation was carried out to develop a response plan, and to find the infection source of the disease.
Methods
A field epidemiologist investigated the symptoms, vaccination histories, living environments, and probable infection sources with 51 residents and 31 teachers and staff members. In July 25, 81 subjects were tested for the hepatitis A virus antibody, and specimens of the initial 3 cases and the last case were genetically tested.
Results
Three cases occurred July 10 to 14, twelve cases August 3 to 9, and the last case on August 29. Among the teachers and staff, no one was IgM positive (on July 25). The base sequences of the initial 3 and of the last case were identical. The vehicle of the outbreak was believed to be a single person. The initial 3 patients were exposed at the same time and they might have disseminated the infection among the patients who developed symptoms in early August, and the last patient might have, in turn, been infected by the early August cases.
Conclusions
The initial source of infection is not clear, but volunteers could freely come into contact with residents, and an infected volunteer might have been the common infection source of the initial patients. Volunteers' washing their hands only after their activity might be the cause of this outbreak. Although there may be other possible causes, it would be reasonable to ask volunteers to wash their hands both before and after their activities.
INTRODUCTION
Hepatitis A is a viral infection transmitted via the fecal-oral route. It does not show chronic progress, but rather has an acute manifestation. After childhood infection with the hepatitis A virus (HAV), it progresses asymptomatically. After producing the antibody for the HAV, symptoms do not recur even after exposure to HAV. However, the progression of an HAV infection in adulthood is serious. Thus, fatal symptoms could be occured without intensive care. Before the 1980s, most people in their 20s had the antibody for hepatitis A because the water and sewage system was incomplete and feces were used as fertilizer in South Korea [1,2]. However, as the chance of exposure to HAV decreased with expanding infrastructure and improved hygiene, the number of adults who had not been infected with HAV in childhood increased, and the seropositive rate for the HAV antibody in people in their 20s continuously decreased [3,4]. As a result, in the late 1990s, the HAV infection spread rapidly among the adolescent and young adult population [1,3,5]. Under these conditions, a strategy for dealing with HAV infection is necessary because additional outbreaks of hepatitis A can continue to be expected.
The occurrence of HAV infection in three disabled residents of a residential facility was reported to a public health center from a hospital located in P city on July 20, 2011. Therefore, an epidemiological investigation was conducted to identify the infection source of the HAV and exact transmission route and to prevent the further spread of the virus.
METHODS
Subjects
Facility A, in which the hepatitis A occurred, is for the severely disabled. Residents in this facility spend most of their time inside the facility. Some of them do outside activities such as going to a school for the disabled and going to church. Considering the conditions of the group residential facility, a complete enumeration investigation was performed with a total of 82 people (51 residents, 13 teachers, and 18 staff members). Although visitors and volunteers who came into contact with the residents are supposed to be included in this investigation, a telephone interview was performed with visitors to examine their symptoms and diagnoses. Considering the incubation period for HAV, volunteers were excluded from the present study because the range of subjects would have extended to include about 200 volunteers a month. Instead, the visiting and volunteering histories were gathered from the hepatitis A patients who had been reported to the K and P cities.
Methods
The epidemiological investigation team was organized from the public health center in K city, which includes facility A. The primary investigation was performed by a field epidemiologist of the public health center on July 20. For most of the residents, bathroom assistance from the staff and volunteers and wearing a diaper were needed due to physical or mental impairment. For this reason, additional cases were likely. The secondary investigation was conducted by the Korea Centers for Disease Control and Prevention (KCDC) epidemiological investigation department, the epidemiological investigation team in the public health policy department of the jurisdictional province government, and the epidemiological investigation team of the public health center in K city on July 25 (Figure 1).
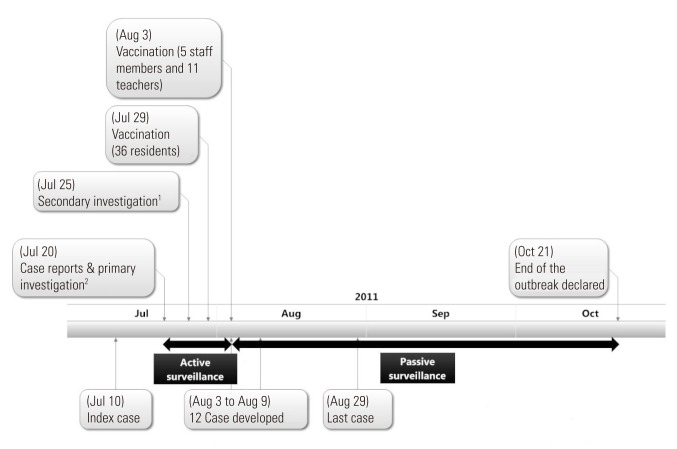
Timeline of epidemiological investigation. The patient with the index case was diagnosed in July 20. 1A seriologic test and genomic test were done. 2Case investigation, questionnaire, and education were performed.
Case monitoring and transmission control
The three cases reported on July 20 had been hospitalized on July 16. Since the primary investigation, active surveillance system had been activated. The anti-HAV immunoglobulin test was conducted on July 25, which was the secondary investigation date. The results of the antibody test were reported on July 29; however, a sufficient supply of vaccine for 52 people was difficult to obtain at once. The disabled residents were vaccinated first since they were a vulnerable group due to their personal hygiene, while teachers were able to manage their personal hygiene with methods such as hand washing. At first, 36 residents seronegative for IgG anti-HAV were vaccinated on July 29, which was the date when the antibody test report was made. Next, 16 staff members and teachers without the antibody were vaccinated on August 3. After finishing the vaccination to group without the antibody on August 3, the active surveillance was converted to passive surveillance. The day when the first resident was discharged from the hospital was July 27. After July 27, residents who were discharged from the hospital and those with symptoms were isolated for monitoring. Isolated residents used a separate restroom in the isolation room. Teachers seropositive for IgG anti-HAV were assigned to these residents. Considering the period needed for antibody production [6], they were isolated until September 3, which was 4 weeks after August 3, which, in turn, was the last vaccination date in the facility.
Interview and living environmental investigation
In the individual interviews, the following information was collected: the hepatitis A vaccination history, clinical symptoms, history of contact with hepatitis A suspected patients, history of travel abroad, conditions of water distribution in the facility, dietary history, resident's outdoor activities, and history of eating and drinking outside the facility. However, the conversations with residents were difficult because most of them were mentally impaired, and thus could not answer most of the interview questions. Therefore, most of the interview questions were answered by the teachers. Only clinical symptoms could be investigated in the individual interviews with residents. Information collected from the teachers for the analysis included the history of traveling abroad, water distribution in the facility, eating history, and outdoor activities for the disabled residents. However, collecting information on the residents' outside eating and drinking history and history of contact with people suspected of having hepatitis A was impossible. Detailed information such as the floor plan of the living unit, daily schedules, and the pattern and frequency of contact among subjects was examined.
Investigation of clinical and environmental specimens
On July 25, for clinical specimens, blood sampling was conducted from 51 disabled residents, 17 teachers (one of the 18 teachers, who had an HAV vaccination history, was excluded), and 13 staff members. The stool specimens were collected from the three confirmed patients to be sent to the KCDC for tests. For the blood tests, antibody tests for HAV IgM and IgG in 81 specimens and HAV genetic tests were performed in the three confirmed cases. The hepatitis B virus serologic test was also performed in one patient with hepatitis B. The HAV genetic test was conducted from stool specimens. For the genetic test of the blood and stool, a reverse transcription polymerase chain reaction (RT-PCR) test was performed. This test was conducted using eight Korean strains of HAV. Three of the eight strains (2010-HAV-JH-VP3-[4], 2010-HAV-JH-VP3-[9], and 2010-HAV-JH-VP3-[10]) were acquired from patients in Jeju island, three more (EU049550, EU049563, and EU049548) were from Gyeonggi province, one of them (KNIH-GS-07-01) was from Gaeseong industrial district, and one of them (KNIH-JN-08-01) was from South Jeolla province. During the monitoring period, additional patients were immediately hospitalized and given the HAV IgM antibody test; however, the genetic test was not performed. The last case occurred on August 29, and genetic tests from the blood and stool were performed for this case.
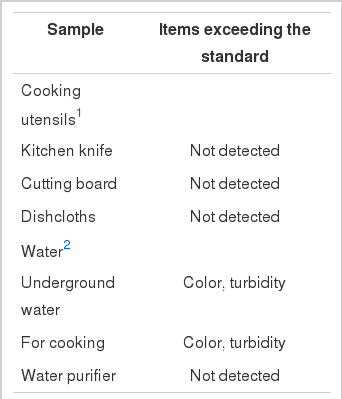
Microbiological tests were performed for Salmonella species, Shigella species, Vibrio species, Escherichia coli, Staphylococcus aureus, Listeria monocytogenes, Campylobacter jejuni, Clostridium perfrigens, Bacillus cereus, and Yersinia enterocolitica with cooking utensils including kitchen knives, cutting boards, and dishcloths as environmental specimens. Filtered water as a source of drinking water, cooking water, and groundwater was sent to the Institute of Health Environment and the public health center in the autonomous district to test for potability. Color, turbidity, odor, taste, NHn-N, NO3-N, total colony counts, total coliforms, fecal coliforms, KMnO4 consumption, total solids, pH, Cl-, Al, Mn, and F were evaluated in the test. Testing of preserved foods was not possible to perform because it was difficult to estimate the date of exposure of these foods, and the HAV incubation period was long.
Case definition
A hepatitis A case was primarily defined as case that occurred among the disabled residents, teachers, staff members, and visitors in facility A since July 10, 2011, which was the date of the attack in the initial case. The final case definition was determined again with the results of the serologic test. Considering the incubation period, a hepatitis A case was defined as occurring among the disabled residents, teachers, and staff members of facility A after June, 2011, with a combination of IgM anti-HAV seropositivity from the antibody test and at least one of the following symptoms: fever, chills, myalgia, nausea, vomiting, diarrhea, abdominal pain, fatigue, loss of appetite, itching, dark urination, and jaundice. The date of the occurrence of the hepatitis A was defined as the date of the onset of symptoms.
Subclinical infection investigation
A subclinical infection was defined as a case among the disabled residents, teachers, and staff members of facility A since June, 2011 with IgM anti-HAV seropositivity in the antibody test but without any of the following symptoms: fever, chilling, myalgia, nausea, vomiting, diarrhea, abdominal pain, fatigue, loss of appetite, itching, dark urination, and jaundice.
Statistical analysis
The attack rate by sex was compared using Fisher's exact test. The attack rates by age, type of subject (disabled resident, teacher, or staff member), and living unit was analyzed with the log likelihood test because the expected frequencies of the attack rates were insufficient to use the chi-squared test. All statistical analyses were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). To calculate the 95% confidence interval of the attack rate with the following equation, the values of the quadratic equation were calculated by assigning π, which was the population fraction, to an unknown variable. These values were for the minimum and the maximum values of the 95% confidence interval [7]. The equation used is as follows:
RESULTS
Epidemic Curve
The initial case occurred on July 10, and two additional cases occurred on July 14. During the active and passive surveillance, three cases occurred on August 3, another three cases on August 4, a case on August 5, three cases on August 6, and two cases on August 9. With the last case on August 29, the total number of cases came to 16 (Figure 2).

Cases of hepatitis A at living facilities for the disabled, by time of onset, July to August 2011. Each square denotes a patient and his/her living unit number in the corresponding square on the curve. The base sequences of 4 cases in July 10, July 14, and August 29 were identical. The other cases were not tested by reverse transcription polymerase chain reaction.
Result of Environmental Investigation and Attack Rate by Resident's Living Unit
The 51 disabled residents lived in 7 living units. A recreation hall was located in the center of the building. There were four living units named A, B, C, and D and three living units named E, F, and G in the hallways on both sides (Figure 3). Each unit (units A and B, units C and D, and units F and G) was connected with another through balconies; however, the pairs of units A and B and units F and G each included one unit with reported cases and one with no case (Figure 3). Each unit had two rooms and a bathroom; each room had a door connecting to the bathroom that had two toilets and a shower.

Floor plan of accommodations. Males and females lived in separate living unit; units A to E for male, units F and G for female. Units A and B, units C and D, and units F and G are connected by balconies.
The male and female residents did not enter units for the opposite sex; however, they could enter other units for the same sex. In addition, they freely moved around the recreation hall and hallways. In addition, they were able to come in contact with each other easily during programmed events and regular daytime activities. There were various programs, and most of them were group programs performed in an assembly hall and an audiovisual room.
By unit, there were 6 cases out of 7 susceptible persons (85.7%) in unit C, 5 out of 8 (62.5%) in unit B, two out of 6 (33.3%) in unit E, and one out of 4 (25.0%) in each of units D and G, and the differences among units were statistically significant (p=0.003). No cases occurred in unit A or F (Table 1, Figure 3).
Symptom Investigation
All of the 16 cases complained of fever. In order of frequency, there were 8 cases (50.0%) with fatigue; 7 cases (43.8%) each of loss of appetite, nausea, and vomiting; 6 cases (37.5%) of the chills; abdominal pain in 5 cases (31.3%); and jaundice in 3 cases (18.8%). Three cases with jaundice occurred on July 10 and 14 and August 3 (data not shown).
Results of Drinking and Cooking Water and Food Investigation
Institutional foodservice was available for the disabled residents, teachers, and staff members. The same menus were provided to all of them during the two month period. Food trays, spoons, and chopsticks were used in common without separation among the groups. Due to the lack of a water supply system, filtered water from groundwater and boiled water were used for drinking water. Groundwater was used for cooking. The disabled residents were found to drink groundwater from the bathroom.
According to the results of the investigation of drinking and cooking water and cooking utensils in Table 2, bacteria were not found from the bacteria test on kitchen knives, cutting boards, or dishcloths. Nor were bacteria found in the filtered water and groundwater for drinking and cooking; however, the color and the turbidity of the cooking water and groundwater were judged to be unfit for drinking. The report on the 47-item drinking water quality examination of groundwater from the P city waterworks had determined the groundwater to be suitable for drinking on December 22, 2010; however, it was then found to be unsuitable due to color, turbidity, iron, and manganese on July 5, 2011. This result was corresponded with the color and turbidity results of the present study.
The kitchen was examined by the sanitary instructor team of the public health center, and none of the foodservice employees were found to have injuries on their hands or complaints such as diarrhea. Health examinations were performed on all of the foodservice employees. There was a possibility that visitors could bring food in from outside; however, there was no chance that the three cases of July could have eaten together.
Result of Clinical Specimen Investigation
From the antibody test on July 25, 15 residents out of 51 were identified to be seropositive for IgG anti-HAV. The three confirmed cases with hepatitis A showed IgG. Since they showed symptoms beginning on July 10 to 14, it can be concluded that the IgG antibody was converted to positive around July 25, which was the date of the blood sampling. The infection risk in the other IgG positive 12 residents was considered to be low when these residents were exposed to HAV. Besides the three confirmed cases, an additional subject showed seropositivity in the IgM anti-HAV test. However, this subject had no symptoms, and the result of the genetic test was negative. Among the 18 teachers and 13 staff members, 30 subjects, that is, all except one person with a vaccination history, underwent the serologic test. Fourteen cases of IgG anti-HAV seropositivity were confirmed, and there was no subject with IgM anti-HAV positivity (Table 1).
To confirm hepatitis A, an additional antibody test was performed in the cases that occurred after the antibody test conducted on July 25. Thirteen cases with symptoms were confirmed with IgM anti-HAV seropositivity from the additional test. The results of the serologic test relative to the termination point of the epidemic are shown in Table 1.
HAV RNA was detected in the initial three cases, and their genotype was confirmed with IA. These three cases were infected from the same source because the genomic sequence similarity corresponded 100% in each of their three strains (2011-KJO-WTK-2-14, 2011-KJO-JHS-2-23, and 2011-KJO-OHJ-2-30). The percent identity in common with existing Korean strains was 94.1% to 96.8%. HAV RNA were found in two out of three stool specimens.
The genomic sequence similarity in the additional strain from the case that occurred on August 29 corresponded 100% with the strains from the initial three cases from July 10 to 14. By this result, it was confirmed that this case (which occurred on August 29) was disseminated from the same virus. HAV RNA was also found in the stool specimen of this additional case.
General Characteristics and Attack Rate
The subjects' general characteristics and attack rates by age, sex, and work position are shown in Table 1. Eleven of the residents, 6 teachers, and 8 staff members out of 81 showed IgM seronegativity and IgG seropositivity. One teacher with an HAV vaccination history was not tested; however, this individual was considered to have immunity. Thus, 26 people were excluded from being counted in the attack rates (Table 1).
According to the case definition, the number of cases was 16 (15 disabled residents and one teacher) among all of the subjects, and the number of susceptible persons was 56. Therefore, the attack rate was 28.6%. There were 15 cases out of the 40 males (37.5%) and one case out of the 16 females (6.3%). The attack rate in the males was significantly higher than in the females (p=0.023). There were 15 cases out of the 40 residents (37.5%), one case out of the 11 teachers (9.1%), and no one among the staff. The attack rate in the disabled residents was high and statistically significant (p=0.025). By the age, the attack rate in the teens was 7 cases out of 12 (58.3%) and that of those in their 30s was 4 cases out of 12 (33.3%); thus, their attack rate was high (p=0.033) (Table 1).
The attack rate in the disabled residents was 37.5%. There were 14 cases out of the 31 males (45.2%) and one case out of the 9 females (11.1%). Although the attack rate in the males was higher than in the females, the difference was not significant (p=0.117). By age, the attack rate in the teens was 7 cases out of 12 (58.3%) and those in their 30s was 4 cases out of 8 (50.0%). Their attack rates were high; however, there was no significant difference (p=0.091) (Table 1).
Subclinical Infection Rate
Besides the 16 cases confirmed by serology and symptoms, one subject was positive for IgM anti-HAV. However, this subject was classified as having a subclinical infection because no symptoms occurred. The number of confirmed cases was 16, and the subclinical infection rate was 5.9% (1/17).
Outside Activity of Cases Occurring in July
The possibility of being exposed to HAV from the outside was examined in the three cases occurring from July 10 to 14. Among the outside activities of disabled residents in facility A, some residents went to religious services and attended one of the two special schools. Two male cases out of the three that occurred in July shared a unit, and they rarely participated in outside activities. On the other hand, the disability of the female resident was not severe; thus, she was active outside the facility. She participated in religious activities and also attended a special school. There was no opportunity in which all three of these cases could participate in outside activities simultaneously during the estimated risk period. Furthermore, there had been no report of hepatitis A in the places where the resident participated in outside activities. The occurrence of hepatitis A was examined by visiting the two special schools that the residents of facility A attended on October 4, and there was no occurrence of hepatitis A found.
History of Contact with Insiders and with Visitors
Two teachers were assigned in a unit to assist disabled residents. An additional four teachers moved among the units as alternate care givers. The male teachers were permitted to enter males' units, and the female teachers were permitted to enter the units of both sexes. After confirming the outbreak of hepatitis A, teachers positive for IgG anti-HAV assisted the infected cases and supervised residents to minimize the contact with one another during the outbreak period. The only male teacher who contracted hepatitis A had worked in units A, B, C, and E from July 1 to 16 and in units A, B, C, and D from July 17 to the date of symptom onset.
Visitors who were relatives of residents had no opportunity to come in contact with all of the three cases that occurred in the middle of the July at the same time. No visitor had been diagnosed with hepatitis A or its symptoms during the expected exposure period (May 20 to June 25) for the cases that occurred in July, according to the results of telephone interviews.
Volunteers mainly assisted with and bathing the residents and cleaning. They cleaned outside of the living units. Volunteers assisted the disabled residents of the same sex in bathing in the bathroom located in the unit. Contact with the opposite sex was not limited among the volunteers and residents except at bath time; thus, the volunteers were available to come into contact with residents of the opposite sex in places other than the residents' units. The volunteers came from two areas, K and P cities, and the number of residents of P city was higher than that of K city. Those with a volunteer history at facility A were searched for among the cases of hepatitis A reported to K and P cities; however, no volunteers appeared in the list of reported cases.
DISCUSSION
It was concluded that the causal pathogen of this outbreak was HAV because 16 cases with clinical symptoms of hepatitis A showed IgM anti-HAV seropositivity in a serologic test. HAV strains can have one of seven genotypes. Four of them (I, II, III, and VII) have been detected in the human body [8]; the other three of them (IV, V, and VI) have been isolated from animals [9]. The genotype isolated from this outbreak was IA, which was detected from cases in the early 2000s [10,11].
RT-PCR tests were performed in the initial three cases that occurred from July 10 to 14 and the last case that occurred on August 29. Their genotypes and genomic sequences from the strains were 100% identical, which means they were disseminated from the same virus.
The original source of infection at facility A could be either of two possibilities. One option would be from foodborne or waterborne pathogens. Another source could be from the contact with a person having an infection history.
Waterborne infection was possible because groundwater, filtered water, and boiled water were used for drinking, and groundwater was used for cooking with no water filtration system at facility A. However, the possibility of waterborne infection was less likely because cases of waterborne infection would continuously occur during the same period. The possibility of infection by cooking water and cooking utensils was also not very high. The same menus were provided by institutional foodservice to the disabled residents, teachers, and staff during the two-month period. Food trays, spoons, and chopsticks were used for common. Because 82 people used the same food trays, spoons, and chopsticks, and only three cases occurred three weeks earlier than the other cases, infection by cooking utensils was unlikely. The possibility of infection by food from outside was also low because there was no way that the initial three cases could have eaten outside food together. If cases had been disseminated from filtered drinking water, cooking water, or food, the size of the outbreak would have been greater, and a unimodal distribution on an epidemic curve would be shown [12]. Therefore, the possibility of infection by water and food can be excluded.
The other possibility is from person-to-person contact. The interval of occurrence of the cases was about three weeks: July 10 to 14, August 3 to 9, and August 29. In addition, a long and irregular pattern was shown on the epidemic curve. Therefore, infection by a personal contact was suspected in this outbreak. Teachers, staff members, visitors, and volunteers could be considered potential transmission vectors inside the facility. Cases could be disseminated from teachers; however, there is no possibility that this occurred because no teacher had symptoms before the occurrence of the initial three cases, and there was no teacher with subclinical infection according to the result of the serologic test on July 25. The same logic could be applied to the staff. The possibility of infection from visitors is less likely because there was no opportunity in which the initial three cases that occurred in July could have simultaneously come into contact with any of the visitors.
Contact with the opposite sex was not limited for volunteers except at bath time. Furthermore, volunteers were available to come into contact with residents outside the living units without any limitations. Thus, if there were patients in the incubation period or with subclinical infection among the volunteers, there could have been a possibility that the initial three cases were simultaneously disseminated from them. However, there was no one who responded as being involved as a volunteer at facility A among the cases of hepatitis A reported to K and P cities. Therefore, it cannot be concluded with certainty that a volunteer was the primary infection source. In sum, the possibility that the HAV outbreak at facility A could have been started by person-to-person spread is high, and volunteers are suspected to be the most likely infection source.
The interval of the three cases that occurred from July 10 to 14 was only four days; thus it is difficult to conclude that any of these cases could have been disseminated from one another. Furthermore, the case that occurred on July 10 had jaundice on July 20, and the case that occurred on July 14 had jaundice on July 21. The infectious period is around 2 to 3 weeks before jaundice to a week after jaundice, or two weeks before symptoms to a week after symptoms [13,14]. Therefore, the possible infectious period of one case from another would be from July 1 to 16; July 16 was the date of hospitalization of the three cases. The mean incubation period of hepatitis A is 28 days, and the possible incubation period is from 15 days to 50 days [13]. As a result, it can be assumed that these three cases were exposed during the same period. Calculating the exposure date by the mean incubation period, the exposure date should have been between June 12 and 15. Using July 10 as the reference, the possible exposure date would have been between May 20 and June 25. Because the two male cases shared unit B, they could have been infected at the same time by a person-to-person route. While a female case lived in unit G, her case could have been disseminated by the same person due to her active outside activity. Thus, it is assumed that the initial three cases were disseminated by personal contact from the same person.
Twelve cases occurred between August 3 and 9 and showed IgM anti-HAV seronegativity in the antibody test on July 25. This antibody is found 5 to 10 days after exposure to the antigen [13]. Considering the estimated exposure period, these 12 cases could not have been exposed during the same period as the initial three cases. Considering the infectious period of the cases that occurred in July (from July 1 to 16), and the incubation period, it is reasonable to assume that the 12 cases were infected by the initial three cases. The male teacher who took care of the initial three cases after hospitalization showed IgM anti-HAV seronegativity in the antibody test on July 25; however, after symptoms appeared, the result was converted to IgM positivity on August 6. It is assumed that the male teacher's case was disseminated from the initial three cases. However, the cases that occurred between August 3 and 9 could have been infected by mutual spread. One case that occurred on August 3 was hospitalized with jaundice on August 5 (Hospitalization was unavailable on August 3 due to a shortage of patient rooms. Thus, this case was isolated in facility A); thus, the possible infectious period of this case was between July 15 and August 3.
The last case that occurred on August 29 had been vaccinated on July 29 because IgM and IgG were negative in the serologic test on July 25. The preventive effect of the hepatitis vaccine is higher than 94% a month after the initial vaccination [2]. Thus, it was concluded that this case was disseminated from the residents or the male teacher with an infectious period in August after the vaccination but before formation of IgG anti-HAV. In this last case, a vaccination failure issue should also be considered. Vaccination failure means that a target pathogen (antigen) develops a disease in spite of being vaccinated, and this condition is caused by one of the following two reasons: vaccine failure and failure to vaccination. Vaccine failure means that the disease develops despite taking into account the incubation period and the normal delay for the protection to be acquired. Other cases of vaccine failure are those in which the vaccination effect is not certain for the specific disease, or the particular marker of protection is not produced [15]. Failure to vaccinate is caused by administrative error, storage failure, or an inappropriate time and number of primary and/or booster vaccinations [15]. Thus, it could be concluded that this case was caused by the failure to vaccinate rather than vaccine failure because the interval between the exposure date (August 1), which was estimated from the mean incubation period, of the last case and the vaccination date was not significantly different.
Because no additional case had occurred after the last occurrence date plus the longest possible incubation period, and the last vaccination was performed on August 3, the end of the outbreak was declared on October 21, 2011.
To calculate the attack rate, the number of cases is divided by the number of exposed persons; however, in this study, the number of cases was divided by the number of susceptible exposed persons (a susceptible exposed attack rate was calculated). The measurement method is very important because it affects the attack rate. The method used in the present study is an objective method for measuring infectivity. However, this method is difficult to apply without identified immunologic results (antibody tests) [16].
Reviewing the attack rate by sex, the attack rate in male residents was significantly higher, and there was only a case among the female residents because the female residents had a smaller chance of coming into contact with the males, who were using different units. Another reason is that the female residents had fewer opportunities to come into contact with the male teacher with symptoms.
For the attack rate by living unit, the attack rates of units B and C were higher than those of the other units. The number of people with immunity in units B, C, and E was one each, and there was no one with immunity in unit F. Thus, the number of susceptible people was relatively high, which means the attack risk was high. Unit F was occupied by female residents, and unit E, which was occupied by male residents, was distant from the other males' units. For these reasons, it is assumed that the unit F and E attack rates were low. No cases occurred in unit A, which was connected to unit B through a balcony; however, an additional case was reported on August 29 in unit D which was connected with unit C. The risk of spread through the balcony would be low because moving through balconies was controlled after the occurrence of the initial case. Frequent contact among the residents in units B and C could be a potential reason; however, no concrete connection was found. It could be assumed that no occurrence in unit A was caused by the relatively low number of susceptible persons and less chance of contact.
Estimating the transmission route among the units by the male teacher's working history, the male teacher had worked in unit B in the early part of July, which was the period of the expected exposure of the male teacher. He had worked in units A, B, C, and D, and was mostly assigned to units B and D beginning in the middle of July, which was the communicable period. Explaining the transmission to units with only the male teacher's working history has limitations; however, it could be assumed that he carried the virus to units B and C, places with a relatively high number of susceptible people among units A, B, C, and D. He could have spread HAV to the case in unit D, where he was assigned relatively often.
The subclinical infection rate of 5.9% was lower than that found in previous studies [17,18]. The reason for the lower rate must be that an antibody test was performed in only new cases with symptoms during the monitoring period. For a more complete investigation, the antibody test should have been repeated at the ending point of the investigation for subjects with IgG and IgM seronegativity in the initial antibody test. The attack rate could also be underestimated by ignoring mild symptoms because asymptomatic infection was not considered. Furthermore, these asymptomatic healthy carriers may have been the source of infection because they were not isolated.
It could be estimated that this outbreak occurred due to person-to-person spread; however, the initial source of infection was not identified. The only method for doing so would have been to collect data from all the volunteers, who were considered to be an infection source, based on the history taking on volunteer activity at facility A in the reported hepatitis A cases. Another limitation of this study was that we did not examine personal contact between local persons reported to be infected and facility volunteers.
The reason volunteers were suspected to be the source of infection was that most of them wash their hands only after volunteering. During activities involving frequent contact with people such as medical practice, the people performing these activities do not always wash their hands before contact. The cases of the volunteers are similar [19,20]. Although the same behavior pattern could be found among the teachers, the possibility that the male teacher was the primary source of infection is extremely unlikely given the result of his antibody test.
To verify infection from the volunteers, analysis of detailed volunteering schedules, records of volunteering activities, their contact information, and an institutional strategy and social atmosphere necessary to support contacting them for additional information would be necessary. However, it would be difficult in practice to collect the volunteers' personal contact information and to contact them to examine whether symptoms exist or not. For these reasons, it could not be concluded with certainty that volunteers who were in the incubation period or had a subclinical infection spread the virus. Nevertheless, given its likelihood, sanitation for volunteers should be emphasized. In particular, hand washing must be performed before activities. It also should be repeated when they are contaminated from urine, feces, and nasal discharge during contact activities. Although it would be difficult to ask volunteers who visit to provide assistance for social reasons to perform hand washing, it is essential to prevent them from being carriers for infectious diseases. Furthermore, it is necessary to prevent themselves from contracting diseases.
The teacher who was the only male case besides the disabled residents could have been infected and have been a carrier after caring for the initial three cases before they had been diagnosed with hepatitis A. In addition, he could have spread the virus by active contact with other residents after dissemination but before showing symptoms. Therefore, it is better that a person with objectively confirmed immunity cares for patients during an outbreak.
In this outbreak, it was possible to prevent the spread of the disease by fast vaccination treatment after the first cases were reported. Even though the teachers and staff were vaccinated five days later than the residents because of an inadequate vaccine supply, severe spreading could be prevented by vaccinating the vulnerable group first. To prevent hepatitis A, a hepatitis A vaccine or immunoglobulin is injected. After common exposure, the hepatitis A vaccine is recommended for healthy people aged from 12 months to 40 years, and the immunoglobulin inoculation is recommended for people aged 41 and over [21]. Both the hepatitis A vaccine and immunoglobulin are available to use in people who have intimate personal contact such as sexual contact and family relationships.
Susceptible persons would be exposed to the patient's feces, in which the most pathogens would be present because there were many people using diapers in facility A. Moreover, the antibody could not be produced in the appropriate time by vaccination alone because the initial cases occurred between July 10 and 14, and the date of vaccination was on July 29 and after, which was two weeks after the initial outbreak [22]. Therefore, simultaneous vaccination with the hepatitis A vaccine and immunoglobulin could be considered for people who changed a patient's diaper or shared units with a hepatitis patient. The same would apply to similar situations.
To increase the vaccination rate for hepatitis A in adolescent and adult groups involved in institutional foodservice and active outdoor activities, policies for governmental support are essential. To increase vaccine coverage rates in youth and adult groups, additional campaigns and efforts targeting them are necessary because the progress of hepatitis A is more serious in young adults and middle-aged people than in young children, and there are fewer opportunities to be vaccinated in youth and adult groups than in infants.
The primary limitation in this epidemiological investigation is that most of the responses were acquired from teachers instead of the residents themselves because face-to-face interviews with them were impossible due to the mental impairment of most of the residents.
The next limitation is that accurate data collection by memory was difficult during the estimated exposure period because the incubation period for hepatitis A is long.
Thirdly, a complete investigation was practically impossible due to the large number of volunteers without personal contact information and their irregular visiting schedules. Volunteer histories were investigated and compared to the reported cases of hepatitis A of P and K cities; however, there was no relationship. In addition, reported data may not be accurate because not every case of hepatitis A is reported.
Finally, the antibody test for hepatitis A was only performed without a genetic test in the case that occurred in August and in the remaining subjects without symptoms. Therefore, the number of cases may have been underestimated. This limitation could affect the subclinical infection rate. Furthermore, it would be difficult to examine their exact relationships in all cases.
Nevertheless, the present epidemiological investigation is meaningful as a reference for future research because serologic data was collected from an almost complete enumeration in a closed group. Moreover, a susceptible exposure attack rate was calculated as a practical indicator of the attack rate, and the subclinical infection rate was analyzed. In the attempt to identify the source of infection, the possibility of infection by a volunteer was assumed, and the importance of hand washing before activities could be emphasized. Therefore, the possible spread of diseases should be prevented by complete sanitation when volunteering.
ACKNOWLEDGEMENTS
Special thanks is extended to the KCDC staff and all the people who supported this epidemiological investigation.
Notes
The authors have no conflicts of interest with the material presented in this paper.