How Well Do U.S. Primary Care and Obstetrics and Gynecology Clinicians Screen for Pregnancy Complications at Well Woman Visits? A Retrospective Cohort Study
Article information
Abstract
Objectives
Pregnancy complications, including pre-eclampsia, gestational diabetes (GDM), and perinatal mood and anxiety disorders (PMADs), impact long-term health. We compared the frequency of screening documentation for pregnancy complications versus a general medical history at well woman visits between providers in primary care and obstetrics and gynecology.
Methods
We conducted a retrospective cohort study of subjects with at least 1 prior birth who presented for a well woman visit in 2019–2020. Charts were reviewed for documentation of a general medical history (hypertension, diabetes, and mood disorders) versus screening for comparable obstetric complications (pre-eclampsia, GDM, and PMADs). The results were compared using the McNemar and chi-square tests as appropriate.
Results
In total, 472 encounters were identified, and 137 met the inclusion criteria. Across specialties, clinicians were significantly more likely to document general medical conditions than pregnancy complications, including hypertensive disorders (odds ratio [OR], 2.45; 95% confidence interval [CI], 1.18 to 5.48), diabetes (OR, 7.67; 95% CI, 3.27 to 22.0), and mood disorders (OR, 10.5; 95% CI, 3.81 to 40.3). Obstetrics and gynecology providers were more likely to document any pregnancy history (OR, 4.50; 95% CI, 1.24 to 16.27); however, they were not significantly more likely to screen for relevant obstetric complications (OR, 2.49; 95% CI, 0.90 to 6.89). Overall, the rate of pregnancy complication documentation was low in primary care and obstetrics and gynecology clinics (8.8 and 19.0%, respectively).
Conclusions
Obstetrics and gynecology providers more frequently documented a pregnancy history than those in primary care; however, the rate was low across specialties, and providers reported screening for clinically relevant complications less frequently than for general medical conditions.
INTRODUCTION
The mean duration of a human pregnancy is 280 days; however, the implications can last a lifetime. Complications that occur during pregnancy can increase the risk of developing long-term health conditions. Pre-eclampsia, a disease unique to the second half of pregnancy, is characterized by new-onset hypertension that may be accompanied by certain symptoms and laboratory abnormalities [1]. Numerous studies have linked this condition to the development of cardiovascular disease, including chronic hypertension [2–6]. Likewise, women diagnosed with gestational diabetes (GDM), carbohydrate intolerance in pregnancy mediated by placental hormone production, have a 7-fold higher risk of developing type 2 diabetes [7–9]. Associations have similarly been drawn between perinatal mood and anxiety disorders (PMADs), including perinatal depression, and long-term morbidity [10].
As a result of these risks, major medical organizations have developed guidelines based primarily on expert consensus and observational studies to enhance the prevention and detection of illness after pregnancy complications. The American Diabetes Association and American College of Obstetricians and Gynecologists (ACOG) recommend lifetime screening every 1–3 years for adult-onset diabetes in women with a history of GDM [11]. Likewise, the American Heart Association and the European Society of Cardiology (of which the Korean Society of Cardiology is an affiliate member) advise that clinicians screen patients for clinically relevant pregnancy complications as part of routine evaluations [12–14].
A well woman visit, generally performed by a clinician in primary care or obstetrics and gynecology, represents an opportunity to screen at-risk women by obtaining a relevant pregnancy history. It is a mandated benefit for all health plans under the U.S. Patient Protection and Affordable Care Act [15]. The intent of the visit is to address family planning needs and age-appropriate preventive care such as immunizations and screening, including for breast and cervical cancer [15,16]. The Women’s Preventive Services Initiative, a federally funded program led by ACOG and the Health Resources and Services Administration, recommends these preventive services for women age 13 and above [17]. Despite societal guidelines, the rate at which providers screen for relevant obstetric complications appears to be poor. A recent study of internists, for example, demonstrated a significantly lower screening rate for a history of pre-eclampsia than for non-pregnancy-related cardiovascular risk factors, such as smoking, hypertension, or diabetes [18].
The objectives of our study were to evaluate the rate at which clinicians document an obstetric history at well woman visits, including screening for a history of pre-eclampsia, GDM, and/or PMADs matched to the non-pregnancy-related medical conditions of chronic hypertension, diabetes, and/or mood disorders, respectively, and to compare the results by specialty. Because clinicians in obstetrics and gynecology provide prenatal, intrapartum, and postpartum care, we hypothesized that they would be more likely than their primary care colleagues to screen for a pregnancy history at well woman encounters.
METHODS
Study Design and Site
We conducted a retrospective cohort study from January 1, 2019 through December 31, 2020 at a large, tertiary medical center that provides primary and specialty care to United States military servicemembers and their dependents.
Inclusion and Exclusion Criteria
Potentially eligible subjects were identified using International Classification of Diseases, 10th revision (ICD-10) codes for a routine well woman visit (Z01.4 series). Subjects were included if they presented to the primary care or obstetrics and gynecology departments or their affiliated satellite clinics for a well woman visit. Subjects were required to be age 18–48 at the time of the encounter, with at least 1 prior birth, and not currently pregnant.
Each subject’s encounter was reviewed in the electronic health record by an investigator (EDM) with a subset of encounters audited by a second investigator (AST). Demographic information was collected, including subjects’ age, race, body mass index (BMI), and military or dependent status. Each chart was then reviewed for any notation of a pregnancy history. For classification purposes, we did not consider isolated documentation of a cesarean delivery in the surgical history as sufficient to meet the criteria for obtaining a pregnancy history. The encounter was assessed for documentation of a general medical history compared to screening for pregnancy complications. Specifically, charts were evaluated for documentation of screening for chronic hypertension, diabetes mellitus, mood disorders, pre-eclampsia, GDM, and PMADs.
Statistical Analysis
Statistical analysis of the primary outcome (frequency of documentation of pregnancy complications compared to general medical complications) was performed using the McNemar test for paired nominal data. Subjects with a documented history of chronic hypertension were excluded from the pre-eclampsia history-taking analysis, given the potential for confounding as to whether an obstetric history was forgone due to its irrelevance in the face of the patient’s chronic medical condition or true oversight of obstetric history. Similarly, subjects with a documented history of diabetes mellitus were excluded from the GDM analysis and subjects with a history of chronic mood disorders were excluded from the analysis of PMADs. The chi-square test of independence was performed to assess the secondary outcome (comparing the frequency at which primary care versus obstetrics and gynecology providers documented a pregnancy history). Lastly, the documentation rate of pregnancy complications was reported and compared for both specialties. A p-value <0.05 was considered statistically significant.
Ethics Statement
The study was approved by the Institutional Review Board at Naval Medical Center Portsmouth (Portsmouth, VA, USA) as a retrospective chart review with a waiver of signed informed consent and complied with the U.S. Federal Policy for the Protection of Human Subjects.
RESULTS
Based on review of ICD-10 coding data, a total of 472 well woman visits were identified over the 24-month period. After review, 335 subjects were excluded. The reasons for exclusion were no history of a prior birth (n=195), outside the prespecified age range (n=83), and inappropriately coded encounters (n=57). Therefore, 137 subjects were included in the final analysis.
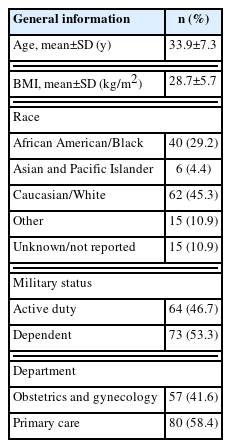
The mean age at the time of the visit was 33.9 years. The majority (58.4%, n=80) of subjects were seen in the primary care department and the remaining 41.6% (n=57) in obstetrics and gynecology. The study population was diverse, with 45.3% Caucasian/White, 29.2% African American/Black, and 4.4% Asian or Pacific Islander. The remaining subjects were of an unspecified or unreported race. The mean BMI at the time of the encounter was 28.8±5.7 kg/m2. The study population was approximately evenly divided between military members and their dependents. Additional demographic data are reported in Table 1.
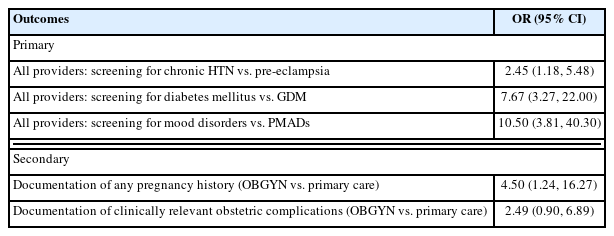
In terms of the primary outcome, clinicians were significantly more likely to document screening for general medical conditions than for comparable pregnancy complications, with odds ratios (ORs) of 2.45 (95% confidence interval [CI], 1.18 to 5.48) for chronic hypertension compared to pre-eclampsia, 7.67 (95% CI, 3.27 to 22.0) for diabetes mellitus compared to GDM, and 10.50 (95% CI, 3.81 to 40.30) for mood disorders compared to PMADs.
Clinicians in the obstetrics and gynecology department were more likely than their primary care counterparts to document any mention of a pregnancy history (OR, 4.50; 95% CI, 1.24 to 16.27). However, they were not significantly more likely to report screening for clinically relevant complications as recommended in societal guidelines (OR, 2.49; 95% CI, 0.90 to 6.89) (Table 2).
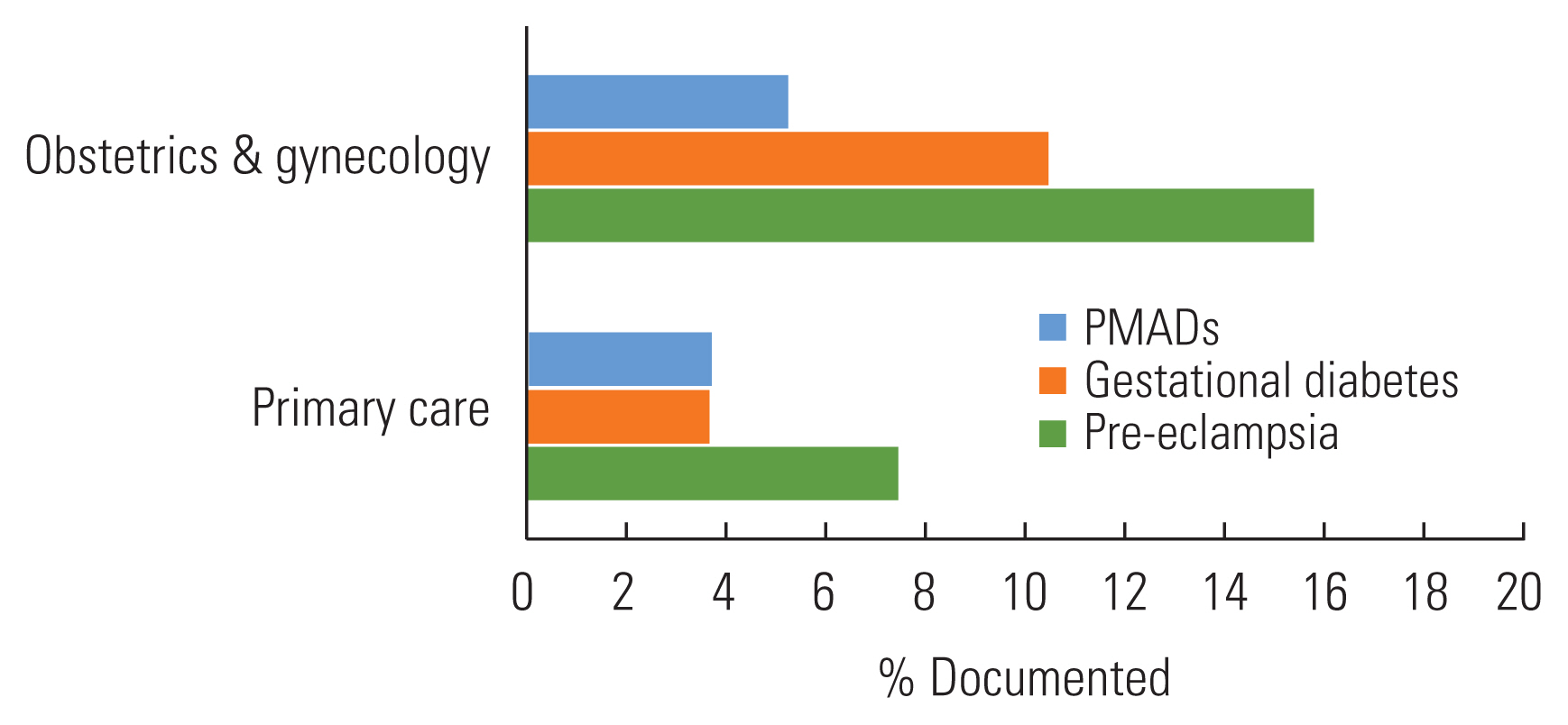
Overall, the rate of clinically relevant pregnancy complication documentation was low in primary care and obstetrics and gynecology clinics (8.8 and 19.0%, respectively), and not significantly different between the 2 departments (p=0.07, Figure 1).
DISCUSSION
In a study population of women presenting for preventive health visits, we demonstrated that clinicians commonly failed to document any pregnancy history and were significantly more likely to screen for general medical conditions than obstetric complications such as pre-eclampsia, GDM, and PMADs despite societal recommendations and their long-term health implications. While providers in obstetrics and gynecology are significantly more likely to document a pregnancy history than their primary care counterparts, they are not more likely to screen for clinically relevant obstetric complications. This gap represents a missed opportunity to identify risk factors early on, initiate targeted interventions or surveillance, and potentially improve outcomes.
Our results are consistent with prior research demonstrating a low screening rate for pre-eclampsia by internists compared to non-pregnancy-related risk factors for cardiovascular disease [18]. Similarly, a study conducted in India among key stakeholders in women’s health, including policymakers, clinicians, and patients demonstrated a limited understanding of the long-term health implications of GDM and hypertensive disorders of pregnancy [19].
Taken together, these findings suggest a need to develop a new strategy. Given that providers in obstetrics and gynecology did not obtain a more thorough pregnancy history than those in primary care, it is unlikely that shifting more well woman visits to this specialty will improve screening rates. Potential options include more robust education in taking a pregnancy history for clinicians in training and public health campaigns to educate women and their providers about the need to screen and the long-term health implications of pregnancy complications. Harnessing technology is another option, such as embedding screening tools into well woman visit templates in the electronic health record.
Our study has several strengths and some limitations. Though conducted in a single healthcare system, our study population was diverse, and visits took place in a variety of settings, including a large tertiary care medical center and smaller, affiliated satellite clinics. Additionally, the clinicians performing well woman visits were of a variety of provider types, including physicians, nurse practitioners, and physician assistants. The combination of these factors enhances the generalizability of our results, although our sample size precluded us from stratifying results based on provider type. Additionally, all visits were reviewed by the same investigator, ensuring consistency, and a subset of encounters was audited by a second investigator for accuracy.
This study is somewhat limited by its retrospective design and reliance on documentation in electronic health records. The option to “copy forward” a note, for example, could lead to documentation of a condition without actual screening. Prior research suggests that the act of “copying forward” is common in clinical practice, with the potential to compromise documentation integrity and trust [20]. It is also possible that clinicians screened subjects for medical conditions but did not document negative responses. However, failure to document pertinent positive and negative conditions limits the ability to act on them.
Our study population consisted of United States military service members and their dependents within a single healthcare system. This population and the care they receive are generally reflective of the broader United States population, although it could still impact the generalizability of the results. Lastly, our study was not powered for our secondary outcomes. Therefore, we cannot be certain that the absence of observed differences between groups was not the result of insufficient power.
In summary, clinicians in our study often failed to obtain a pregnancy history and screen subjects for clinically relevant obstetric complications at well woman visits, regardless of specialty. This suggests a need to reassess history-taking in medical education and efforts to raise awareness among medical providers and the public about the long-term implications of pregnancy complications.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Medvescek ED, Thagard AS, Shvartsman K. Data curation: Medvescek ED, Thagard AS. Formal analysis: Medvescek ED, Thagard AS, Raiciulescu S, Shvartsman K. Funding acquisition: None. Methodology: Medvescek ED, Thagard AS, Shvartsman K. Writing – original draft: Medvescek ED, Thagard AS. Writing – review & editing: Medvescek ED, Thagard AS, Raiciulescu S, Shvartsman K.
ACKNOWLEDGEMENTS
The views expressed in this manuscript reflect the results of research conducted by the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of the Air Force, Uniformed Services University, Department of Defense, or the United States Government.
EDM and AST are military service members and KS and SR are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a United States Government work as a work prepared by a military service member or employee of the United States Government as part of that person’s official duties.