Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 46(3); 2013 > Article
-
Original Article
Medical Care Utilization During 1 Year Prior to Death in Suicides Motivated by Physical Illnesses - Jaelim Cho1, Won Joon Lee1, Ki Tae Moon2, Mina Suh3, Jungwoo Sohn1, Kyoung Hwa Ha1, Changsoo Kim1, Dong Chun Shin1, Sang Hyuk Jung4
-
Journal of Preventive Medicine and Public Health 2013;46(3):147-154.
DOI: https://doi.org/10.3961/jpmph.2013.46.3.147
Published online: May 31, 2013
1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
2Samsung Life Insurance, Seoul, Korea.
3National Cancer Center, Goyang, Korea.
4Department of Preventive Medicine, Ewha Womans University School of Medicine, Seoul, Korea.
- Corresponding author: Changsoo Kim, MD, PhD. 50 Yonsei-ro, Seodaemun-gu, Seoul 120-749, Korea. Tel: +82-2-2228-1880, Fax: +82-2-392-8133, preman@yuhs.ac
Copyright © 2013 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- Many epidemiological studies have suggested that a variety of medical illnesses are associated with suicide. Investigating the time-varying pattern of medical care utilization prior to death in suicides motivated by physical illnesses would be helpful for developing suicide prevention programs for patients with physical illnesses.
-
Methods
- Suicides motivated by physical illnesses were identified by the investigator's note from the National Police Agency, which was linked to the data from the Health Insurance Review and Assessment. We investigated the time-varying patterns of medical care utilization during 1 year prior to suicide using repeated-measures data analysis after adjustment for age, gender, area of residence, and socioeconomic status.
-
Results
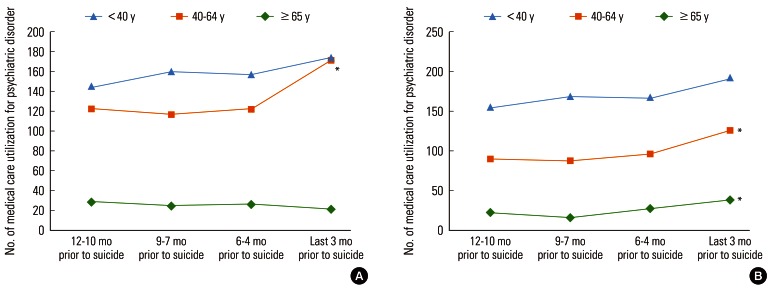
- Among 1994 suicides for physical illness, 1893 (94.9%) suicides contacted any medical care services and 445 (22.3%) suicides contacted mental health care during 1 year prior to suicide. The number of medical care visits and individual medical expenditures increased as the date of suicide approached (p<0.001). The number of medical care visits for psychiatric disorders prior to suicide significantly increased only in 40- to 64-year-old men (p=0.002), women <40 years old (p=0.011) and women 40 to 64 years old (p=0.021) after adjustment for residence, socioeconomic status, and morbidity.
-
Conclusions
- Most of the suicides motivated by physical illnesses contacted medical care during 1 year prior to suicide, but many of them did not undergo psychiatric evaluation. This underscores the need for programs to provide psychosocial support to patients with physical illnesses.
- The suicide rates of the Republic of Korea (ROK) have been the highest among developed countries since 2003, reaching 31.2 per 100 000 inhabitants in 2010 [1]. Many epidemiological studies have suggested that a variety of medical illnesses such as cancer [2-5], diabetes mellitus [6], and spinal cord injury [7] are associated with suicide. These physical illnesses are attributed to 25% of suicides, and the percentage increases with age [8]. A case-control study using psychological autopsy data suggested that physical illness is the most frequent life problem related to suicide and contributes to 62% of suicides in older people [9]. Considering that the suicide rates of the elderly in the ROK have been increasing [10], it is necessary to develop suicide prevention programs for patients with physical illnesses.
- In line with this, investigating the time-varying pattern of medical care utilization, including mental health care, prior to suicide would be helpful. A previous study on the pattern of medical care utilization prior to suicide was conducted in the ROK [11], but the issue of suicides motivated specifically by physical illnesses has not been elucidated. Previous studies have suggested that less than 10% of the elderly contact mental health care during 1 year prior to suicide although more than 30% of all ages do [12] and 40% of older suicides are motivated by chronic physical illnesses in the ROK [13]. Collectively, suicides motivated by physical illnesses might access mental health care less frequently than other suicides, and their pattern of medical care utilization would need to be assessed, including demographic factors influencing the pattern. Thus, this study concentrated on the pattern of medical care utilization including mental health care during 1 year prior to death in suicides motivated by physical illnesses.
INTRODUCTION
- Data Sources
- To investigate medical care utilization during 1 year prior to death in suicides motivated by physical illness, we obtained data from the National Police Agency and Health Insurance Review and Assessment (HIRA). The National Police Agency provided data on 8413 suicides in 2004 identified by the investigator's notes, which included the motivation for suicide. Physicians (KT Moon and JY Park) reviewed the findings in the investigator's notes and found that 2169 suicides (25.8%) were motivated by physical illnesses such as cancer, chronic obstructive pulmonary disease (COPD), dementia, and disability [13]. Among 2169 deaths described as suicides by the investigator's notes, 1994 subjects were confirmed as suicides by the researchers of previous studies [11,14]. Information on medical care utilization during 1 year prior to suicide was obtained by linking to the data from HIRA. The data consisted of a diagnosis code according to the International Classification of Diseases, 10th revision, the date of diagnosis, medical expenditures, and health insurance premium rates. We excluded the last medical care utilization data from the analysis because suicide could be reported during the last hospital care or admission and this case could be related to a fatal suicide attempt. The institutional review board of Yonsei University Health System approved this study (approval number 4-201-0273).
- Statistical Analysis
- Demographic variables such as age, gender, area of residence, and socioeconomic status were considered to be confounders related to medical care utilization [15]. The study population was categorized into three age groups: <40, 40 to 64, and ≥65 years of age. We acquired information on the area of residence classified as metropolitan, urban, or rural. Based on the health insurance premium rate, socioeconomic status was divided into quintiles and the lowest quintile (quintile 1) included Medical Aid beneficiaries. Comparisons of age, gender, residence, and socioeconomic status with the demographics of those who had not contacted medical services during the same period were conducted with chi-squared tests. We performed multiple logistic regression analysis to examine factors associated with not contacting medical care during 1 year prior to suicide. As described in a previous study [11], the time-varying patterns of medical care utilization in suicides for physical illness were analyzed across quarters during a year prior to suicide. We used repeated-measures data analysis ('proc mixed' procedure) after adjusting for age, gender, residence, and socioeconomic status. Interaction terms (quarter×age group, quarter×gender, quarter×residence, and quarter×socioeconomic status) were included in the statistical models, and none was significant. Subgroup analyses of medical care visits for any reason were conducted after stratification of disease groups: cancer (C00-C99), hypertension (I10-I15), diabetes mellitus (E10-E14), ischemic heart disease (I20-I25), and COPD including asthma (J40-J46). After stratification of age and gender, we analyzed the pattern of medical care visits for psychiatric disorders (F00-F99) after adjusting for residence, socioeconomic status, and diseases. Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA), and all analyses were blinded to the identity of suicides by the use of randomly generated identification numbers.
METHODS
- Among 1994 suicides for physical illness, the number of ≥65-year-old suicides was 1216 (61.0%), while 1893 (94.9%) suicides contacted medical care services during 1 year prior to suicide (Table 1). Comparisons between those who contacted medical care during 1 year prior to suicide and those not making any contacts showed significant differences in their age (p<0.001), gender (p=0.006), and socioeconomic status (p=0.013). The median values (interquartile range) in the number of medical care visits and total medical expenditures during 1 year prior to suicide were 16 (17) and 904 605 won (2 433 020 won), respectively (where 1 000 000 won is approximately 1000 US dollar). The number of suicides who had medical care visits for psychiatric disorders was 445 (22.3%). In multiple logistic regression analysis, several characteristics including being <40 years old (vs. ≥65 years old; odds ratio [OR], 5.04; 95% confidence interval [CI], 2.76 to 9.19), men (OR, 1.75; 95% CI, 1.08 to 2.83), and the lowest socioeconomic status (vs. the highest; OR, 2.57; 95% CI, 1.12 to 5.87) were associated with not contacting medical care during 1 year prior to suicide (data not shown).
- In Table 2, the number of medical care visits during a year prior to suicide showed the same median values in quarters, but the temporal changes in the number of visits were statistically significant across quarters (p<0.001). Among age groups and gender, there were significant differences (p<0.001, p<0.001), but no differences for residence (p=0.093) or socioeconomic status (p=0.087).
- Individual medical expenditures remarkably increased as the date of suicide approached (p<0.001), as shown in Table 3. The medical expenditures showed no differences by gender (p=0.400) or residence (p=0.905), but the differences among age groups (p<0.001) and socioeconomic status (p=0.019) were significant.
- After stratification by disease group (Table 4), the number of medical care visits was found to have increased significantly during 1 year prior to suicide, with the exception of individuals with ischemic heart disease (p=0.391). In terms of medical expenditures, individuals with cancer (p<0.001), hypertension (p<0.001), diabetes mellitus (p<0.001), ischemic heart disease (p=0.022), and COPD (p<0.001) showed significant increases across quarters.
- Among the six age/gender groups (Figure 1), the number of medical care visits for psychiatric disorders prior to suicide significantly increased in 40- to 64-year-old men (p=0.002), <40-year-old women (p=0.011), and 40- to 64-year-old women (p=0.021) after adjustment for residence, socioeconomic status, and morbidity.
RESULTS
- Suicides motivated by physical illnesses had contact with medical care services more frequently and spent more on medical services as suicide approached. The number of medical care visits for psychiatric disorders also showed an increase during 1 year prior to suicide in underlying disease groups including cancer and COPD. As expected, more subjects accessed medical care during 1 year prior to death in suicides motivated by physical illnesses (94.9%) than among all suicides (83.7%) [11]. However, about 5% of suicides motivated by physical illnesses did not receive medical care during 1 year prior to suicide, and they were more likely to be <65-year-old men with low socioeconomic status. Under the detailed review of the investigator's notes, it was found that suicides without medical care utilization during 1 year prior to suicide included ≥65-year-old suicides with dementia and <65-year-old suicides with disability due to stroke or spinal cord injury. The disabled are known to be at high risk of suicide [16], and in case of dementia, its association with suicide is unclear, but depression could be the prodromal symptom of dementia [17]. Disabled and dementia patients are less likely to contact medical care prior to suicide, so community support programs need to be developed and maintained for suicide prevention.
- Among suicides motivated by physical illness, 22.3% accessed medical care for psychiatric disorders, and the percentage was lower than that of all suicides (25.0%) in 2004. Those who contacted mental health care included patients with hypertension (32.1%), COPD (20.7%), diabetes mellitus (20.2%), and cancer (12.6%). In Western countries, it is known that about 90% of suicides are associated with underlying psychiatric disorders [18,19], but the relationship between underlying psychiatric disorders and suicide might be weaker in Asian countries [20]. A Chinese psychological autopsy study suggested that 48% of suicides aged 15 to 34 years had underlying psychiatric disorders [21]. Comparing the present study to the Chinese study might be inadequate because our study subjects included all ages, but further analysis showed that 31.3% of suicides for physical illness aged 15 to 34 years accessed medical care for psychiatric disorders. In light of the findings from the Chinese study, the percentage of those who underwent psychiatric consultation might be lower than that of suicides who have suffered from underlying psychiatric disorders. That is, most of suicides motivated by physical illnesses underwent medical care during 1 year prior to suicide, but many of them did not undergo psychiatric evaluation. This underscores the need for programs to provide psychosocial support to patients with physical illnesses. In practice, for example, psychosocial interventions such as patient education and social support for cancer patients is effective for improving the quality of life [22], which is inversely associated with increased risk for suicide [23].
- Among suicides with physical illness, 291 (14.6%) suicides received medical care for cancer in the present study, but previous studies showed that 649 (5.6%) cancer patients were included in all suicides in 2004 [11,14]. This suggests that every patient with cancer among suicides might not be motivated by cancer, but the discrepancy could also be derived from the fact that the number of unknown motivations for suicide was 2355 (28.0%) in the data from the National Police Agency. In addition, the remarkable increase in medical costs over time prior to suicide in the present study suggests that economic instability might contribute to the motivation toward suicide Bin addition to disease severity, its treatment, or psychosocial response to progression [5].
- Age and gender are well-known factors related to medical care utilization, and the frequency of medical care utilization is higher in the elderly and women [24]. In terms of the number of medical care visits, there were statistically significant differences among age groups and between men and women in the present study, with the 65-year-old or older group and women accessing medical care more frequently, as expected. Meanwhile, there was no notable difference among metropolitan, urban, and rural area of residence in either the number of visits or the medical expenditures, which is consistent with a previous study comparing health service utilization in urban and rural Korea [25]. The difference in socioeconomic status was observed only in total medical expenditures, and a notable finding was that the lowest socioeconomic level showed relatively high costs compared to the other groups throughout the whole period and the highest socioeconomic level showed a dramatic increase during the last 3 months prior to suicide. This suggests that patients with chronic physical illness requiring medical expenditures for long periods of time might fall to the lowest socioeconomic level and have severe psychosocial stress, leading to suicide motivated by chronic physical illness. Furthermore, those with the highest socioeconomic status might be newly diagnosed as having severe physical illness requiring massive treatment, followed by sudden economic instability and psychosocial stress. This highlights the need for short-term intensive intervention in addition to long-term management for suicide prevention in patients with chronic physical illnesses in health care.
- The proportion of the elderly was the highest among suicides motivated by physical illnesses, which is consistent with previous studies that suggested physical illness was associated with higher suicide risk among the elderly [9,26,27]. After stratification of age and gender, 40- to 64-year-old suicides motivated by physical illnesses contacted mental health care significantly more frequently during the last quarter prior to suicide compared to the first quarter, but the difference was not observed to be significant in the elderly. According to previous studies, most depressed older patients are undiagnosed or misdiagnosed as physical illnesses [28-30]. Besides, depression tends to be manifested by physical symptoms rather than psychiatric symptoms more in the Asian elderly [31]. Therefore, strategies for suicide prevention should include early detection of suicidal thoughts and prompt intervention, and education and training in suicide prevention should be mandatory in general practitioners or other non-psychiatric physicians [32].
- The present study identified suicides motivated by physical illnesses using national data. Through national record linkage, we conducted the first study, to our knowledge, on the pattern of medical care utilization in suicides motivated by physical illnesses. However, several limitations should be noted. First, the motivation toward suicide in the findings of the investigator's notes was arbitrarily classified. However, this might be inevitable because the investigator's note had no common form for its terms about the motivation for suicide. In addition, we regarded any obscurity and any discordance between two physicians' classification as unknown reasons (n=2355, 28.0%), and this might have caused the number of suicides for physical illnesses to be underestimated. Second, suicide data from the National Police Agency did not cover all suicides, so this would lead to a discrepancy with the national death statistics (n=11 523). The number of common suicides between suicide data from the National Police Agency and the national death statistics was 7744 (67.2%), and it was revealed that 669 subjects were not suicides by post-mortem examination. To reduce the incompleteness of data, further psychological autopsy studies including post-mortem examination and in-depth interviews with family members and close associates [33] would be needed. Nonetheless, the data from the National Police Agency is the most accessible information on the motivations for suicides in a limited setting, so it could be a basis on which to conduct further psychological autopsy studies.
- A majority of suicides motivated by physical illnesses received medical care services during 1 year prior to suicide, and medical expenditures significantly increased prior to suicide. Focusing on psychiatric disorders, suicides motivated by physical illnesses contacted psychiatrists more frequently as the date of suicide approached. However, the pattern of increase in the number of visits was significant only in the 40-to 64-year-old men and women after stratification by age and gender. The proportion of those who had contact with psychiatrists among suicides motivated by physical illnesses was lower than that of suicides overall. Suicide prevention strategies for suicides motivated by physical illnesses such as psychosocial support and education for early detection of suicidal thoughts should be implemented with consideration for these characteristics of medical care utilization including mental health care.
DISCUSSION
ACKNOWLEDGEMENTS
- 1. Statistics Korea. Annual report on the cause of death statistics 2004. 2005. cited 2013 Feb 20. Available from: http://kosis.kr (Korean)
- 2. Levi F, Bulliard JL, La Vecchia C. Suicide risk among incident cases of cancer in the Swiss Canton of Vaud. Oncology 1991;48(1):44-47. 1987498ArticlePubMed
- 3. Storm HH, Christensen N, Jensen OM. Suicides among Danish patients with cancer: 1971 to 1986. Cancer 1992;69(6):1507-1512. 1540887ArticlePubMed
- 4. Labisi O. Suicide risk assessment in the depressed elderly patient with cancer. J Gerontol Soc Work 2006;47(1-2):17-25. 16901875ArticlePubMed
- 5. Miller M, Mogun H, Azrael D, Hempstead K, Solomon DH. Cancer and the risk of suicide in older Americans. J Clin Oncol 2008;26(29):4720-4724. 18695256ArticlePubMed
- 6. Kyvik KO, Stenager EN, Green A, Svendsen A. Suicides in men with IDDM. Diabetes Care 1994;17(3):210-212. 8174449ArticlePubMed
- 7. DeVivo MJ, Black KJ, Richards JS, Stover SL. Suicide following spinal cord injury. Paraplegia 1991;29(9):620-627. 1787986ArticlePubMed
- 8. Mackenzie TB, Popkin MK. Medical illness and suicide. In: Blumenthal SG, Kupfer DJ, editors. Suicide over the life cycle: risk factors, assessment, and treatment of suicidal patients. Washington, DC: American Psychiatric Press; 1990. p. 205-232
- 9. Harwood DM, Hawton K, Hope T, Harriss L, Jacoby R. Life problems and physical illness as risk factors for suicide in older people: a descriptive and case-control study. Psychol Med 2006;36(9):1265-1274. 16734947ArticlePubMed
- 10. Shah A, Bhat R, MacKenzie S, Koen C. Elderly suicide rates: cross-national comparisons of trends over a 10-year period. Int Psychogeriatr 2008;20(4):673-686. 17963591ArticlePubMed
- 11. Cho J, Kang DR, Moon KT, Suh M, Ha KH, Kim C, et al. Age and gender differences in medical care utilization prior to suicide. J Affect Disord 2013;146(2):181-188. 23017538ArticlePubMed
- 12. Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry 2002;159(6):909-916. 12042175ArticlePubMedPMC
- 13. Park JY, Jung SH, Kim JH, Chae YM. Suicidal incidence, methods and reasons of committed suicide according to age and sex in South Korea, 2004. J Korean Assoc Soc Psychiatry 2007;12(2):68-77. (Korean)
- 14. Park JY, Moon KT, Chae YM, Jung SH. Effect of sociodemographic factors, cancer, psychiatric disorder on suicide: gender and age-specific patterns. J Prev Med Public Health 2008;41(1):51-60. (Korean). 18250606ArticlePubMedPDF
- 15. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995;36(1):1-10. 7738325ArticlePubMed
- 16. Agerbo E, Sterne JA, Gunnell DJ. Combining individual and ecological data to determine compositional and contextual socio-economic risk factors for suicide. Soc Sci Med 2007;64(2):451-461. 17050054ArticlePubMed
- 17. Rubio A, Vestner AL, Stewart JM, Forbes NT, Conwell Y, Cox C. Suicide and Alzheimer's pathology in the elderly: a case-control study. Biol Psychiatry 2001;49(2):137-145. 11164760ArticlePubMed
- 18. Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry 2004;4: 37. 15527502ArticlePubMedPMC
- 19. Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsä ET, Kuoppasalmi KI, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry 1993;150(6):935-940. 8494072ArticlePubMed
- 20. World Health Organization. Suicide risk high for young people. 2009. cited 2013 Apr 26. Available from: http://www.who.int/mediacentre/multimedia/podcasts/2009/suicide_prevention_20090915/en/
- 21. Zhang J, Xiao S, Zhou L. Mental disorders and suicide among young rural Chinese: a case-control psychological autopsy study. Am J Psychiatry 2010;167(7):773-781. 20395398ArticlePubMedPMC
- 22. Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Educ Couns 2003;50(2):179-186. 12781933ArticlePubMed
- 23. Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet 2002;360(9347):1728-1736. 12480425ArticlePubMed
- 24. Jeon GS, Choi ES, Lee HY. Gender-related difference in the utilization of health care services by Korean adults. J Korean Acad Public Health Nurs 2010;24(2):182-196. (Korean)
- 25. Joo K, Kim H, Lee S, Min H. A comparative study on medical utilization between urban and rural Korea. Korean J Prev Med 1996;29(2):311-330. (Korean)
- 26. Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med 2004;164(11):1179-1184. 15197042ArticlePubMed
- 27. Quan H, Arboleda-Flórez J, Fick GH, Stuart HL, Love EJ. Association between physical illness and suicide among the elderly. Soc Psychiatry Psychiatr Epidemiol 2002;37(4):190-197. 12027246ArticlePubMed
- 28. Borson S, Barnes RA, Kukull WA, Okimoto JT, Veith RC, Inui TS, et al. Symptomatic depression in elderly medical outpatients. I. Prevalence, demography, and health service utilization. J Am Geriatr Soc 1986;34(5):341-347. 3958408ArticlePubMed
- 29. Koenig HG, George LK, Peterson BL, Pieper CF. Depression in medically ill hospitalized older adults: prevalence, characteristics, and course of symptoms according to six diagnostic schemes. Am J Psychiatry 1997;154(10):1376-1383. 9326819ArticlePubMed
- 30. Crawford MJ, Prince M, Menezes P, Mann AH. The recognition and treatment of depression in older people in primary care. Int J Geriatr Psychiatry 1998;13(3):172-176. 9565839ArticlePubMed
- 31. Chiu HF, Takahashi Y, Suh GH. Elderly suicide prevention in East Asia. Int J Geriatr Psychiatry 2003;18(11):973-976. 14618546ArticlePubMed
- 32. De Leo D. Suicide over the lifespan: the elderly. In: Kastenbaum R, editor. Macmillan encyclopaedia of death and dying. New York: Thomson Gale; 2003. p. 837-843
- 33. Hawton K, Appleby L, Platt S, Foster T, Cooper J, Malmberg A, et al. The psychological autopsy approach to studying suicide: a review of methodological issues. J Affect Disord 1998;50(2-3):269-276. 9858086ArticlePubMed
REFERENCES
| Total (n = 1994) | Medical care utilization (n = 1893) | No medical care utilization (n=101) | p-value | |
|---|---|---|---|---|
| Age (y) | ||||
| <40 | 117 (5.9) | 99 (5.2) | 18 (17.8) | <0.001 |
| 40-64 | 661 (33.2) | 618 (32.6) | 43 (42.6) | |
| ≥65 | 1216 (61.0) | 1176 (62.1) | 40 (39.6) | |
| Gender | ||||
| Men | 1253 (62.8) | 1176 (62.1) | 77 (76.2) | 0.006 |
| Women | 741 (37.2) | 717 (37.9) | 24 (23.8) | |
| Residence | ||||
| Metropolitan | 648 (32.5) | 614 (32.4) | 34 (33.7) | 0.86 |
| Urban | 1053 (52.8) | 999 (52.8) | 54 (53.5) | |
| Rural | 293 (14.7) | 280 (14.8) | 13 (12.9) | |
| Socioeconomic status1 | ||||
| Quintile 1 | 701 (35.2) | 663 (35.0) | 38 (37.6) | 0.013 |
| Quintile 2 | 301 (15.1) | 281 (14.8) | 20 (19.8) | |
| Quintile 3 | 318 (16.0) | 295 (15.6) | 23 (22.8) | |
| Quintile 4 | 312 (15.7) | 299 (15.8) | 13 (12.9) | |
| Quintile 5 | 362 (18.2) | 355 (18.8) | 7 (6.9) | |
| Medical care utilization during 1 year prior to suicide | ||||
| No. of visits, median (IQR) | 16 (8, 25) | |||
| Total medical expenditures (in thousands of Korean won), median (IQR) | 905 (231, 2664) | |||
| Cancer (C00-C99) | 291 (14.6) | |||
| Hypertension (I10-I15) | 595 (29.8) | |||
| Diabetes mellitus (E10-E14) | 374 (18.8) | |||
| Ischemic heart disease (I20-I25) | 124 (6.2) | |||
| Chronic obstructive pulmonary disease or asthma (J40-J46) | 347 (17.4) | |||
| Psychiatric disorder (F00-F99) | 445 (22.3) |
|
No. of medical care visits in individuals |
|||||
|---|---|---|---|---|---|
| 12-10 mo prior to suicide | 9-7 mo prior to suicide | 6-4 mo prior to suicide | Last 3 mo prior to suicide | p-value | |
| Total subjects | 4.0 (1.0, 6.0) | 4.0 (1.0, 6.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | <0.0011 |
| Age (y) | |||||
| <40 | 1.0 (0.0, 4.0) | 1.0 (0.0, 4.0) | 2.0 (0.0, 5.0) | 2.0 (0.0, 5.0) | <0.001 |
| 40-64 | 3.0 (1.0, 6.0) | 3.0 (1.0, 6.0) | 3.0 (2.0, 6.0) | 4.0 (1.0, 7.0) | |
| ≥65 | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | |
| Gender | |||||
| Men | 3.0 (1.0, 6.0) | 3.0 (1.0, 6.0) | 4.0 (1.0, 7.0) | 4.0 (2.0, 6.0) | <0.001 |
| Women | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 5.0 (2.0, 8.0) | |
| Residence | |||||
| Metropolitan | 4.0 (1.0, 7.0) | 4.0 (1.0, 7.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 0.09 |
| Urban | 3.0 (1.0, 6.0) | 4.0 (1.0, 6.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | |
| Rural | 4.0 (1.0, 7.0) | 4.0 (2.0, 6.0) | 4.0 (2.0, 8.0) | 4.0 (2.0, 8.0) | |
| Socioeconomic status2 | |||||
| Quintile 1 | 4.0 (1.0, 6.0) | 4.0 (2.0, 6.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 0.09 |
| Quintile 2 | 3.0 (1.0, 6.0) | 3.0 (1.0, 6.0) | 3.0 (2.0, 6.0) | 3.0 (1.0, 6.0) | |
| Quintile 3 | 3.0 (1.0, 6.0) | 4.0 (1.0, 6.0) | 3.0 (2.0, 6.0) | 4.0 (2.0, 7.0) | |
| Quintile 4 | 3.0 (1.0, 6.0) | 3.0 (1.0, 6.5) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | |
| Quintile 5 | 4.0 (2.0, 6.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 8.0) | 5.0 (2.0, 7.0) | |
Values are expressed as median (interquartile range).
1 Significant difference among quarters (within-group). Other p-values refer to among subgroups (between-group); using repeated-measures data analysis after adjusting for age, gender, residence, and socioeconomic status.
2 Based on the health insurance premium rate. Quintile 1 included Medical Aid beneficiaries.
| 12-10 mo prior to suicide | 9-7 mo prior to suicide | 6-4 mo prior to suicide | Last 3 mo prior to suicide | p-value | |
|---|---|---|---|---|---|
| Total subjects | 82 (18, 296) | 85 (20, 311) | 108 (23, 454) | 153 (28, 746) | <0.0011 |
| Age (y) | |||||
| <40 | 23 (0, 155) | 18 (0, 162) | 48 (0, 279) | 57 (0, 371) | <0.001 |
| 40-64 | 78 (12, 353) | 75 (14, 315) | 114 (23, 618) | 162 (23, 914) | |
| ≥65 | 89 (24, 295) | 98 (28, 319) | 112 (28, 406) | 156 (38, 698) | |
| Gender | |||||
| Men | 69 (11, 290) | 73 (15, 285) | 95 (20, 459) | 128 (22, 746) | 0.40 |
| Women | 106 (28, 305) | 106 (28, 339) | 124 (30, 450) | 203 (42, 739) | |
| Residence | |||||
| Metropolitan | 85 (19, 348) | 88 (24, 349) | 112 (23, 421) | 156 (33, 795) | 0.91 |
| Urban | 77 (17, 283) | 81 (17, 285) | 101 (22, 491) | 141 (27, 736) | |
| Rural | 92 (18, 266) | 106 (28, 327) | 122 (29, 440) | 182 (32, 727) | |
| Socioeconomic status2 | |||||
| Quintile 1 | 94 (18, 319) | 102 (24, 353) | 124 (22, 505) | 161 (34, 761) | 0.02 |
| Quintile 2 | 60 (18, 232) | 59 (14, 208) | 78 (21, 349) | 106 (18, 415) | |
| Quintile 3 | 76 (14, 272) | 86 (17, 282) | 81 (18, 368) | 101 (18, 565) | |
| Quintile 4 | 80 (17, 308) | 75 (18, 281) | 119 (30, 559) | 156 (29, 782) | |
| Quintile 5 | 80 (20, 330) | 95 (26, 391) | 112 (30, 429) | 207 (50, 1016) |
Values are expressed as median (interquartile range).
1 Significant difference among quarters (within-group). Other p-values refer to among subgroups (between-group); using repeated-measures data analysis after adjusting for age, gender, residence, and socioeconomic status.
2 Based on the health insurance premium rate. Quintile 1 included Medical Aid beneficiaries.
| 12-10 mo prior to suicide | 9-7 mo prior to suicide | 6-4 mo prior to suicide | Last 3 mo prior to suicide | p-value1 | |
|---|---|---|---|---|---|
| No. of medical care visits | |||||
| Cancer | 4.0 (2.0, 7.0) | 5.0 (3.0, 8.0) | 6.0 (3.0, 9.0) | 6.0 (4.0, 8.0) | <0.001 |
| Hypertension | 5.0 (3.0, 8.0) | 5.0 (3.0, 8.0) | 6.0 (3.0, 8.0) | 6.0 (3.0, 8.0) | 0.003 |
| Diabetes mellitus | 5.0 (3.0, 8.0) | 5.0 (3.0, 8.0) | 6.0 (3.0, 8.0) | 6.0 (3.0, 9.0) | <0.001 |
| Ischemic heart disease | 5.0 (3.0, 8.0) | 6.0 (3.0, 9.0) | 6.0 (3.0, 8.0) | 6.0 (3.0, 9.0) | 0.39 |
| COPD or asthma | 5.0 (3.0, 8.0) | 5.0 (3.0, 8.0) | 6.0 (3.0, 9.0) | 6.0 (4.0, 9.0) | <0.001 |
| Medical expenditures (in thousands of Korean won) | |||||
| Cancer | 168 (36, 758) | 195 (59, 1005) | 560 (100, 1908) | 1116 (265, 2862) | <0.001 |
| Hypertension | 131 (46, 381) | 136 (47, 402) | 160 (48, 534) | 204 (61, 736) | <0.001 |
| Diabetes mellitus | 133 (52, 486) | 160 (59, 583) | 235 (76, 945) | 272 (68, 1333) | <0.001 |
| Ischemic heart disease | 182 (56, 580) | 184 (71, 703) | 240 (37, 821) | 426 (74, 1412) | 0.02 |
| COPD or asthma | 137 (50, 363) | 162 (57, 486) | 219 (71, 742) | 248 (85, 1053) | <0.001 |
Figure & Data
References
Citations

- Suicide risk of chronic diseases and comorbidities: A Korean case-control study
Areum Song, Emily Jiali Koh, Weon-Young Lee, Shusen Chang, Jiseun Lim, Minjae Choi, Myung Ki
Journal of Affective Disorders.2024; 349: 431. CrossRef - Late-life suicide in an aging world
Diego De Leo
Nature Aging.2022; 2(1): 7. CrossRef - Risk factors for suicidal behavior in older adults
D.P. Ponomareva, M.S. Artemieva M.S. Artemieva
Vestnik nevrologii, psihiatrii i nejrohirurgii (Bulletin of Neurology, Psychiatry and Neurosurgery).2022; (1): 18. CrossRef - Innovating Technology-Enhanced Interventions for Youth Suicide: Insights for Measuring Implementation Outcomes
Hannah S. Szlyk, Jia Tan, Rebecca Lengnick-Hall
Frontiers in Psychology.2021;[Epub] CrossRef - Suicide prevention in older adults
Carlos Augusto de Mendonça Lima, Diego De Leo, Gabriel Ivbijaro, Igor Svab
Asia-Pacific Psychiatry.2021;[Epub] CrossRef - Suicide in late life: A viewpoint
Diego De Leo, Andrea Viecelli Giannotti
Preventive Medicine.2021; 152: 106735. CrossRef - Understanding the impact of clinical characteristics and healthcare utilizations on suicide among cancer sufferers: a case-control study in Hong Kong
Yu Vera Men, Tai-Chung Lam, Cheuk Yui Yeung, Paul Siu Fai Yip
The Lancet Regional Health - Western Pacific.2021; 17: 100298. CrossRef - Risk Factors for Suicide in a National Sample of Veterans With Multiple Sclerosis
Quinn D. Kellerman, Narineh Hartoonian, Megan L. Beier, Steven L. Leipertz, Charles Maynard, Trisha A. Hostetter, Jodie K. Haselkorn, Aaron P. Turner
Archives of Physical Medicine and Rehabilitation.2020; 101(7): 1138. CrossRef - Wearing a happy mask: mother’s expressions of suicidality with postpartum depression
Regina Praetorius, December Maxwell, Komal Alam
Social Work in Mental Health.2020; 18(4): 429. CrossRef - Adaptation of evidence‐based suicide prevention strategies during and after the COVID‐19 pandemic
Danuta Wasserman, Miriam Iosue, Anika Wuestefeld, Vladimir Carli
World Psychiatry.2020; 19(3): 294. CrossRef - Contact with primary and mental health care prior to suicide: A systematic review of the literature from 2000 to 2017
Kim Stene-Larsen, Anne Reneflot
Scandinavian Journal of Public Health.2019; 47(1): 9. CrossRef - Use of prescription medication prior to suicide in Norway
Anne Reneflot, Silje L. Kaspersen, Lars Johan Hauge, Jorid Kalseth
BMC Health Services Research.2019;[Epub] CrossRef - Use of primary healthcare services prior to suicide in Norway: a descriptive comparison of immigrants and the majority population
Carine Øien-Ødegaard, Anne Reneflot, Lars Johan Hauge
BMC Health Services Research.2019;[Epub] CrossRef - Clinical epidemiology of long-term suicide risk in a nationwide population-based cohort study in South Korea
Hyewon Lee, Woojae Myung, Chunsoo Lee, Junbae Choi, Ho Kim, Bernard J. Carroll, Doh Kwan Kim
Journal of Psychiatric Research.2018; 100: 47. CrossRef - Areas of uncertainties and unmet needs in bipolar disorders: clinical and research perspectives
Michael Bauer, Ole A Andreassen, John R Geddes, Lars Vedel Kessing, Ute Lewitzka, Thomas G Schulze, Eduard Vieta
The Lancet Psychiatry.2018; 5(11): 930. CrossRef - A study of people who attempted suicide referred to the emergency ward of Ali Ibn Abi Taleb hospital, Rafsanjan, Iran (2016)
Alireza Taherifard, Hassan Ahmadinia, Reza Vazirinejad, Zahra Javadi, Seyed Zia Tabatabaei, Mohsen Rezaeian
Journal of Occupational Health and Epidemiology.2018; 7(4): 201. CrossRef - Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data
Jee-Ae Kim, Seokjun Yoon, Log-Young Kim, Dong-Sook Kim
Journal of Korean Medical Science.2017; 32(5): 718. CrossRef - Effectiveness of Nursing Preventive Interventions in Suicide re- Attempts
B Ghanbari, SK Malakouti, M Nojomi, K Alavi, SH Khaleghparast, A Sohrabzadeh
Iran Journal of Nursing.2016; 29(99): 34. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


