Measurement and Decomposition of Socioeconomic Inequality in Metabolic Syndrome: A Cross-sectional Analysis of the RaNCD Cohort Study in the West of Iran
Article information
Abstract
Objectives
Socioeconomic inequality in metabolic syndrome (MetS) remains poorly understood in Iran. The present study examined the extent of the socioeconomic inequalities in MetS and quantified the contribution of its determinants to explain the observed inequality, with a focus on middle-aged adults in Iran.
Methods
This cross-sectional study used data from the Ravansar Non-Communicable Disease cohort study. A sample of 9975 middle-aged adults aged 35-65 years was analyzed. MetS was assessed based on the International Diabetes Federation definition. Principal component analysis was used to construct socioeconomic status (SES). The Wagstaff normalized concentration index (CIn) was employed to measure the magnitude of socioeconomic inequalities in MetS. Decomposition analysis was performed to identify and calculate the contribution of the MetS inequality determinants.
Results
The proportion of MetS in the sample was 41.1%. The CIn of having MetS was 0.043 (95% confidence interval, 0.020 to 0.066), indicating that MetS was more concentrated among individuals with high SES. The main contributors to the observed inequality in MetS were SES (72.0%), residence (rural or urban, 46.9%), and physical activity (31.5%).
Conclusions
Our findings indicated a pro-poor inequality in MetS among Iranian middle-aged adults. These results highlight the importance of persuading middle-aged adults to be physically active, particularly those in an urban setting. In addition to targeting physically inactive individuals and those with low levels of education, policy interventions aimed at mitigating socioeconomic inequality in MetS should increase the focus on high-SES individuals and the urban population.
INTRODUCTION
The rapid economic development of industrial societies in recent decades has yielded shifts in lifestyle patterns, contributing to the main elements of metabolic syndrome (MetS) [1]. MetS has become a serious public health issue around the globe [2] with an increasing trend over time [3]. Worldwide, over a billion individuals are now affected by MetS [4]. MetS is a group of risk factors that occur together, including abdominal obesity, insulin resistance, high blood pressure, high triglycerides, and low levels of high-density lipoprotein (HDL) cholesterol (HDL-C) [2]. MetS is associated with an increased risk of certain adverse health consequences such as type 2 diabetes and cardiovascular disease and their associated mortality [5,6]. MetS is affected by several factors, including individuals’ dietary patterns, socioeconomic status (SES), level of physical activity, age, sex, and genetic background [7-9].
The prevalence of MetS varies based on its definition and the location and composition of the study population [8,9]. The reported prevalence of MetS among adults mostly ranges from 12% to 35% in the literature [10]. The prevalence of MetS differs around the globe, particularly in Asian countries, due to the differing lifestyles of diverse ethnic populations [11]. A systematic review of Iranian adults aged ≥19 years showed a 10-60% prevalence of MetS, depending on age, sex, and location [12].
Previous research has investigated the association between the prevalence of MetS and various demographic and socioeconomic factors such as age, sex, income level, and education level to determine whether a socioeconomic gradient exists in the prevalence of MetS. Studies have shown that MetS is also related to SES when measured using parameters such as wealth, income, education, or job class. A meta-analysis showed that the risk of MetS was statistically significantly increased when associated with a socioeconomic gradient (odds ratio, 1.16) [10].
Although several studies in Iran and other countries [10,12] have assessed the relationship between socioeconomic factors and MetS, these studies did not measure the extent of the inequality in MetS or identify the contributing factors that explained such inequalities. The only study measuring the socioeconomic disparity in MetS in Iran focused on adolescents [13]. Little is known about the extent of the inequalities in MetS among middle-aged Iranian adults. To enhance our understanding of the inequality in MetS and the underlying factors in middle-aged adults, this study measured the extent of socioeconomic inequality in MetS among a sample of middle-aged Iranians and quantified the contribution of socioeconomic and demographic factors to those inequalities.
METHODS
Data Source and Sample
This study used baseline data obtained from the Ravansar Non-Communicable Disease (RaNCD) cohort study. The RaNCD is a regional study, part of the Prospective Epidemiological Research Studies in IrAN (PERSIAN), that assesses middle-aged adults (35-65 years) in the western district of Ravansar, Iran. The RaNCD is the first cohort study to explore non-communicable diseases in a Kurdish population. The Ravansar population is approximately 50 000 and all are of Iranian Kurdish ethnicity. The sample size enrolled for the RaNCD is proportional to all individuals covered by each health center in the Ravansar district. The original sample contained 10 065 middle-aged adults, of which 90 subjects were excluded because of missing data on variables used in this study. In total, data from 9975 individuals were analyzed in this study. Written informed consent was required for participant recruitment. Quality assurance (QA) and quality control (QC) measures were established by central and regional teams for QA/QC to confirm that all procedures were conducted in line with the protocol of the PERSIAN cohort. Further details on the design and the sampling procedures can be found elsewhere [14,15].
Outcome Variable
MetS was assessed according to the International Diabetes Federation (IDF) definition. According to the IDF, an individual has MetS if they have the mandatory criterion of a high waist circumference (≥90 cm for male and ≥85 cm for female) plus 2 or more of the following criteria: reduced HDL-cholesterol (HDL level <40 mg/dL in male and <50 mg/dL in female), elevated blood pressure (BP) (systolic/diastolic BP ≥130/85 mmHg or current treatment for hypertension), elevated triglyceride level (>150 mg/dL), and elevated fasting plasma glucose (≥100 mg/dL or previously diagnosed type 2 diabetes) [16]. Blood samples were collected to measure triglycerides, HDLcholesterol, and fasting blood glucose in the cohort participants. The colorimetric method was used to measure triglycerides and HDL-cholesterol levels. High waist circumference was defined as ≥0.9 m and ≥0.85 m for male and female, respectively. Sitting BP was measured twice on each arm after a 10-minute rest, and the average of the 2 measurements for each arm were calculated. The higher measurement of the 2 arms was considered the mean systolic BP and diastolic BP.
Socioeconomic Status
Based on previous studies, we utilized the wealth index, which was generated using principal component analysis (PCA), to measure SES. To estimate wealth scores, data on housing conditions and ownership of various durable assets (i.e., smartphone, freezer, vacuum cleaner, TV, dishwashing machine, car, motorcycle, rooms per capita, laptop, housing area [in meters squared], type of kitchen, and kind of house ownership) were included in the PCA model. The PCA generated a weight for each variable and then generated an index according to the sum of all weights of the included variables for each participant. The participants were categorized into 5 quintiles based on their wealth index. Details on measuring SES using PCA have been published elsewhere [17,18].
Demographic variables
Demographic data were collected on sex, age (35-45, 46-55, or 56-65 years), marital status (single/divorced/widowed, or married), and residence (rural or urban).
Health-related variable
The level of physical activity was measured using metabolic equivalent (MET) rates based on the self-reported daily activities of the RaNCD participants. One MET equals the amount of oxygen/energy consumed in 1 minute when quiet (resting metabolic rate), which is approximately 3.5mL/kg/min. Following the example, 4 METs requires 16mL/kg/min of energy [19], we calculated the METs for each activity using a compendium of physical activities [20]. The mean MET rates of the cohort participants were calculated (i.e., 41 METs/hr/day) and participants with less than the mean MET rate were considered to have an insufficient level of physical activity.
Statistical Analysis
Measuring inequalities in MetS
We used the concentration index (CI) to examine socioeconomic inequality in MetS. The CI is a summary measure that shows the extent of inequality in health or health-related outcomes that are systematically linked with SES [21,22].
The CI for MetS is given by:
where yi is the health outcome (MetS), and ri is the fractional rank of individual i in the socioeconomic index distribution (computed as ri =i/n), and μ is the proportion or mean of MetS. The CI shows whether MetS is concentrated among the poor or the rich and ranges from -1 to +1. The negative (positive) value denotes the disproportionate concentration of MetS among the poor (the rich). The higher the absolute value of CI, the greater the extent of inequality in MetS. A zero CI indicates that there are no socioeconomic-related inequalities in the distribution of MetS. As MetS was a binary variable, we employed a Wagstaff-type normalization method to quantify the CI in the range of −1 and +1, by multiplying the calculated CI by
Decomposition analysis
To identify the explaining factors of socioeconomic inequality in MetS, a decomposition analysis of the CI was conducted. It allowed us to calculate the extent to which socioeconomic, demographic, and health-related variables contributed to the socioeconomic inequality in MetS among the study population. Supposing a linear relationship between MetS, y, and a range of k determinants ( ) [25]:
The CI for MetS (y) can be written as:
where
Since MetS was defined dichotomously, a logistic model was employed to estimate the marginal effects (βk) of each determinant. Values of (βk) were used to estimate the contributions of k determinants to CIn. In this study, a p-value <0.05 indicated statistical significance. Stata version 16.0 (StataCorp., College Station, TX, USA) was used to analyze the data.
Ethics Statement
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences (KUMS) (ethics code: IR.KUMS.REC.1397.521).
RESULTS
A total of 9975 middle-aged adults were included in our analysis. Most of the study population were female (52.5%), aged 35-44 years (44.1%), lived in urban areas (59.4%), were married (90.3%), and had low levels of physical activity (64.0%). The overall prevalence of MetS was 41.7%, with a higher prevalence among females than males (44.5 and 38.5%, respectively). The prevalence of MetS was higher among those who were ≥55 years (51.9%), physically inactive (45.2%), and lived in an urban area (45.0%) (Table 1).
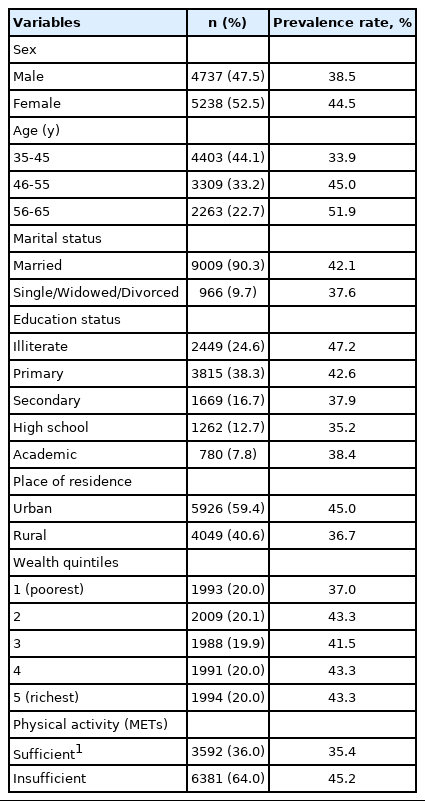
Determinant variables for the prevalence of metabolic syndrome among RaNCD cohort participants aged 35-65 in Iran
The overall CIn of MetS was 0.042 (95% confidence interval , 0.019 to 0.065). The value of CIn for MetS was 0.012 (95% confidence interval, -0.018 to 0.044) in female and 0.101 (95% confidence interval, 0.067 to 0.135) in male. A positive CIn sign indicated that MetS was more concentrated among the rich. The sign and value of the CIn were statistically significant (p<0.001) (Table 2).
A negative CI value for the predictor variables (CIk) suggested a disproportionate concentration of females, individuals aged 55-65 years, and physically inactive individuals among the poor. Also, the urban population and married participants were mainly concentrated among the rich (indicated by a positive CIk). A positive marginal effect indicated that the determinant had a positive association with MetS and had a high probability of MetS compared with the reference. The results of decomposition analysis indicated that the largest contributions to the observed inequalities in MetS came from SES, followed by residence, physical activity, and education level. SES contributed to 71.5% of the inequality in MetS. In addition, residence (46.7%), physical activity (32.2%), and education level (-30.2%) were explaining factors for observed inequality in MetS, respectively. The explained inequality in MetS was 0.040 and the residual (unexplained) CIn was 0.002 (Table 3).
DISCUSSION
The aim of the present study was to measure the extent of socioeconomic inequalities in MetS in a sample of Iranian adults aged 35-65 years. To the best of our knowledge, no published study has investigated the socioeconomic inequalities in MetS using inequality measures of middle-aged adults in Iran. Our findings reveal a pro-poor inequality in MetS. This study also identified the contribution of determinants to help explain the observed inequality. SES, residence, physical activity, and education were the most important contributors to the observed inequality. The prevalence of MetS was found to be higher in females, high-SES individuals, urban dwellers, and older age groups.
We also found a high overall prevalence of MetS in the study participants (41%), slightly higher than that reported by Nikbakht et al. [26]. They estimated the prevalence of IDF defined MetS at 37% in middle-aged adults in Iran. A possible explanation for this difference in prevalence may be that our study was conducted among the ethnic Kurdish population in western Iran, while the previous study was carried out in the Fars Province of southern Iran. Differences in nutritional and behavioral patterns as well as the environmental and geographical exposures of these 2 ethnicities can, to some extent, lead to a disparity in health-related outcomes. This is in line with a previous study that found a significant variation in the prevalence of MetS by region and ethnicity [27].
In addition to a high prevalence of MetS, an unequal distribution of MetS favoring the poor was found. The CIn for MetS had a positive sign, suggesting a higher concentration of MetS among rich middle-aged adults. Consistent with our findings, a previous study conducted on adolescents in Iran showed that the CI for cardiometabolic parameters was positive, which also indicated a higher concentration of these parameters among the rich [13].
We used the CI decomposition technique to estimate the contribution of each factor to the observed inequalities. As a preferred method in health inequalities studies, this approach provides insightful evidence for health policymakers to help them in designing effective policy interventions for reducing inequality in health. Our decomposition results identified 4 major contributors to inequality in MetS. SES was found to be the main contributor to the observed inequality, contributing 71.5% of the disparity in MetS. This means that if wealth was equally distributed across socioeconomic groups, then socioeconomic-related inequalities in MetS would decline by 71.5% (i.e., if there were no contribution from the SES variable, the degree of MetS inequality would have been 71.5% smaller).
We found that the prevalence of MetS increased with increasing wealth quintiles. Any controversy over the association between MetS and SES may be due to different definitions and socio-cultural contexts. However, consistent with our findings, previous studies in Iran have reported that high-SES significantly increases the risk of MetS [13] and obesity [28,29]. Similarly, other studies have indicated that the prevalence of MetS significantly increases with increasing SES in both low-and middle-income and high-income countries. In a study by Yang et al. [30], a lower prevalence of MetS was found in manual laborers and economically inactive men compared with men with non-manual jobs. A study by Joshi et al. [31] conducted in India indicated that women with high SES were >4 times more likely to have MetS compared to men with low SES. One possible explanation may be that SES can affect diet and nutritional patterns and, thus, BMI and serum lipid levels. In addition, individuals with high SES are more likely to afford plentiful energy-dense foods and drinks [32]. Another possible explanation is that individuals with high SES are more likely to have sedentary occupations, which, according to a previous study, have a higher risk of developing MetS [33].
We also identified the area of residence (rural or urban) as the second contributor to socioeconomic inequality in MetS. Affirming our results, studies conducted in Iran and other countries like India and Mexico also showed higher rates of MetS in urban populations [26,34,35]. In the previously mentioned Iranian study of adolescents, area of residence was the main variable related to inequalities in MetS. That study also found higher low-density lipoprotein-cholesterol levels, higher fasting blood sugar levels, lower HDL-cholesterol levels, and higher waist circumferences in the first compared to the last tertile of SES [13]. In the previous Iranian study of middle-aged adults, MetS was found to be more common in urban participants than rural participants, although this difference was not statistically significant [26]. Noshad et al. [36] also demonstrated that the urban population was significantly more likely to have MetS compared to rural residents. We found a higher prevalence of MetS among individuals in the richest wealth quintile and in the urban population. Increased wealth may lead to unhealthy habits in urban populations, such as the intake of energy-dense packaged food and sedentary lifestyles.
Physical activity was the third factor, contributing to 32.1% of wealth-related inequality in MetS. We found that participants with sufficient physical activity were less likely to have MetS when compared to those who were not active. Participants in the richest (fifth) SES quintile had the lowest proportion of sufficient physical activity (22.3%) followed by the fourth quintile. Consistent with our results, a previous study in Iran indicated that poor physical activity was more concentrated in high-SES groups. Even though more opportunities to be physically active are available to those with higher SES, the amount of time spent on physical exercise may be reduced because of the opportunity cost of time spent on physical activity [37]. Also, as shown in the present study, achieving a higher SES may require a longer workday with little free time to participate in physical and leisure activities.
Corroborating our findings, Costa et al. [38] also found that physically active individuals were 33% less likely to have MetS than physically inactive individuals. A meta-analysis of cohort studies conducted in Asia, Europe, South America, and the United States indicated that a high level of leisure-time physical activity was associated with a significantly lower risk of MetS. A moderate level of leisure-time physical activity was also associated with a lower risk of MetS, but was not statistically significant [39].
Education level made the largest negative contribution to inequality in MetS. It contributed significantly to reducing socioeconomic-related inequality in MetS. Our results showed that the proportion of participants with a high level of education was higher in rich groups than in poor groups (the CI of education had a positive sign). This may explain why education contributed significantly to reducing MetS inequality among the study population. In our study, participants with low education levels were at higher risk of MetS than those with high levels of education. Consistent with our findings, the study by Costa et al. [38] showed that less-educated individuals had a significantly higher prevalence of MetS using the absolute and relative inequality indices. A study on the risk factors of MetS among middle-aged adults in Iran also demonstrated that a higher level of education was associated with a decreased risk of MetS [40]. One possible explanation is that highly educated individuals are more likely to have greater health awareness and make better health-related choices.
This study is one of the first attempts to enhance our understanding of the magnitude of socioeconomic inequality in MetS. However, it clearly had some limitations. First, the crosssectional nature of the study limits our ability to know the causal relationship between MetS and the independent variables. Second, the findings might not be generalized to all adults aged 35-65 years in Iran because the study focused on only one district. Third, various factors such as dietary patterns can contribute to inequality in the prevalence of MetS between SES groups but were not assessed in our study. A future study investigating the contribution of dietary patterns would be interesting. In the future, it will also be important to explore changes and trends in MetS inequality using the data of all RaNCD waves. Moreover, the lack of studies measuring and decomposing the magnitude of socioeconomic inequality in MetS made it difficult to precisely compare our findings with those of previous related studies.
In conclusion, we found a significant pro-poor socioeconomic-related inequality in MetS in the middle-aged population in Iran, suggesting that MetS was more concentrated among the rich. SES, area of residence, physical activity, and education level were the important explaining factors of inequality in MetS in the Iranian middle-aged population. Policy interventions aimed at mitigating socioeconomic inequality in MetS should focus more attention on the rich, urban population, as well as the physically inactive and poorly educated. To this end, encouraging these groups to adopt healthy lifestyles by launching physical activity campaigns, particularly in urban areas, may be helpful. For example, health education programs could increase risk perception and physical activity in rich and urban populations, especially those with lower levels of education.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
This study was funded by Kermanshah University of Medical Sciences (KUMS) (grant No. 980483).
AUTHOR CONTRIBUTIONS
Conceptualization: Soofi M, Karamimatin B. Data curation: Soofi M. Formal analysis: Soofi M. Funding acquisition: Soofi M. Methodology: Soofi M, Karamimatin B. Project administration: Karamimatin B. Visualization: Karamimatin B, Najafi F. Writingoriginal draft: Soofi M. Writing-review and editing: Karamimatin B, Soltani S, Najafi F.
ACKNOWLEDGEMENTS
None.


