Frequency and Related Factors of Masked Hypertension at a Worksite in Korea
Article information
Abstract
Objectives
Masked hypertension is associated with metabolic risks and increased risk of cardiovascular disease. The purpose of this study was to identify the frequency of and risk factors of masked hypertension in Korean workers.
Methods
The study was conducted among 121 employees at a hotel in Gyeongju, Korea, from December 2008 to February 2009. We measured blood pressure (BP) both in the clinic and using 24-hour ambulatory BP monitors for all subjects. Hypertension was defined independently by both methods, and subjects were classified into four groups: true normotension, masked hypertension, white coat hypertension, and sustained hypertension.
Results
The frequency of masked hypertension in our study group was 25.6%. Compared with true normotension, the factors related to masked hypertension were male gender (odds ratio [OR], 10.7; 95% confidence interval [CI], 1.41 to 81.09), aging one year (OR, 0.88; 95% CI, 0.78 to 0.99), clinic BP 120-129/80-84 mmHg (OR, 8.42; 95% CI, 1.51 to 46.82), clinic BP 130-139 / 85-89 mmHg (OR, 12.14; 95% CI, 1.80 to 81.85), smoking (OR, 5.51; 95% CI, 1.15 to 26.54), and increase of total cholesterol 1 mg / dL (OR, 1.05; 95% CI, 1.02 to 1.08). In males only, these factors were clinic BP 120-129 / 80-84 mmHg (OR, 15.07; 95% CI, 1.55 to 146.19), clinic BP 130-139 / 85-89 mmHg (OR, 17.16; 95% CI, 1.56 to 189.45), smoking (OR, 11.61; 95% CI, 1.52 to 88.62), and increase of total cholesterol 1 mg/dL (OR, 1.05; 95% CI, 1.01 to 1.09).
Conclusions
The frequency of masked hypertension was high in our study sample. Detection and management of masked hypertension, a known strong predictor of cardiovascular risk, could improve prognosis for at-risk populations.
INTRODUCTION
In Korea, cardiovascular disease is one of the major causes of death [1], and hypertension is a major risk factor for cardiovascular disease. Hypertension has been reported to be as high as 35% and 21%, respectively, in population attributable risks of incidence of cerebrovascular disease and ischemic heart disease in men [2]. According to data from the 2007 National Health and Nutrition Survey, the prevalence of hypertension is 24.9% (men 27.1%, women 22.1%) for adults over 30 years of age [3]. Since it is expected that the incidence of hypertension will increase due to aging of the population, there have been numerous studies of hypertension prevalence, incidence and related factors, and the Korean national and local governments have increased investment in hypertension management policy.
Diagnosis of hypertension is simple, and is made when blood pressure (BP) is equal to or greater than 140/90 mmHg during at least two separate clinic visits. However, the validity of BP measurement is questionable because BP varies according to situation, and differs significantly due to inter-observer error, the white coat effect, and other factors [4].
BP measurement equipment, aneroid, electronic, and 24-hour ambulatory BP monitoring are currently used to assess BP. Among these methods, 24-hour ambulatory BP monitoring enables the continuous observance of changes in BP during activities of daily life, so that BP can be measured automatically at specific time intervals (every 30 minutes or every hour), resulting in very accurate measurements of BP. This method offers the advantage of being free from observer error. In the most recent treatment guidelines [5] for hypertension from the European Society of Hypertension (ESH) and European Society of Cardiology (ESC), and in the seventh report [4] of the 2003 US Hypertension Joint National Committee (JNC 7), it was reported that 24-h ambulatory BP is more valuable for predicting prognosis than other measures, as it more accurately assesses the risk of cardiovascular disease than measurements of BP made during clinic or office visits, and is closely related to damage to target organs [4,5].
Masked hypertension (or isolated ambulatory hypertension), which was first introduced by Devereux and Pickering as "white-coat normotension" in 1990 [6], is defined as apparent normotension by clinic or office measurement, but as hypertension by 24-h ambulatory BP monitoring. Recently, clinical interest in masked hypertension has increased, as it has been reported that masked hypertension is associated with target organ damage and cardiovascular risk [7-9].
Masked hypertension is present in 9% to 24% of the general population [8,9], and in 6% to 28% of patients with hypertension [10-12]. Related factors of masked hypertension include younger age, male gender, obesity, high clinic BP, drinking and smoking [9,13,14].
Although 24-hour ambulatory BP monitoring is essential for the diagnosis of masked hypertension, it is unfamiliar and limited to use in Korea. Moreover, research on 24-hour ambulatory BP monitoring is rare, and some studies have been conducted only in patients who have visited hospitals for precision diagnosis of hypertension [10,12]. Studies regarding the prevalence of masked hypertension and related factors in the general population are rare.
The present study measured clinic or office BP and 24-hour ambulatory BP in workers at a single worksite where all employees participation were possible, classified BP according to results of measurement, and identified related factors of masked hypertension for analysis.
METHODS
I. Study Subjects
The study was conducted in a sample of 121(89.0%) volunteers among 136 total hotel employees, in Gyeongju, Korea, from December 2008 to February 2009. BP was measured using an automatic sphyg-momanometer, and 24-hour ambulatory BP monitoring was conducted after completion of a structured questionnaire by participants. All participants provided informed consent. The Institutional Review Board of Dongguk University Gyeongju Hospital approved this study.
II. Methods
A) Questionnaire Survey
The questionnaires of general characteristics contained inquiries about gender, age, education, marital status, etc. The questionnaires of health related characteristics contained inquiries about drinking, smoking, regular exercise, presence or absence of doctor's diagnosis and medication of chronic disease such as hypertension, heart disease, dyslipidemia, etc. The questionnaires of occupational characteristics contained inquiries about division of work, work shift, occupational stress. The questionnaire survey was administered by nurses who were fully educated with regard to the purpose and methods of this study.
Occupational stress was measured using the Korean Occupational Stress Scale (KOSS), the validity and reliability of which has previously been evaluated [15]. Groups were classified as either high or low occupational stress based on the median value.
B) BP measurement
(1) Clinic BP measurement
Clinic BP measurements were made using an automatic sphygmomanometer (HEM-907, Omron Healthcare Co., Ltd., Japan), which is appropriate for AAMI/SP10 standards, according to standard procedures in the report of JNC 7 [4]. BP measure-ments were made at least twice for each subject with an interval of 2 minutes. In cases of measurement differences over 5 mmHg, the mean was calculated by including an additional measurement taken after 2 minutes. Hypertension was detected by clinic or office BP was defined when the systolic blood pressure (SBP) was equal to or greater than 140 mmHg, or when the diastolic blood pressure (DBP) was equal to or greater than 90 mmHg.
(2) 24-hour ambulatory BP monitoring
We measured 24-hour ambulatory BP using the Tonoport V (GE Marquette, WI, USA) after attachment of a properly-sized cuff on the left upper arm of each subject. Daytime BP was measured continuously over an interval of 30 minutes, from 6:00 AM to 10:00 PM, and nighttime BP was measured over an interval of 1 hour. During measurement, subjects were allowed to carry out routine daily activities, and a diary was provided for subjects to record subjective symptoms or changes in their physical or mental conditions.
We included 24-hour ambulatory BP data in analyses if the monitoring period included > 8 hours daytime and > 4 hours nighttime; these periods were estimated from the subjects' diaries. If the 24-hour ambulatory BP data for a given subject were not complete, that subject was retested on another day. Artifactual readings during 24-hour ambulatory BP monitoring were identified by heart specialists according to previously described criteria [16] and were omitted from analyses.
Hypertension by 24-hour ambulatory BP was defined when the mean daytime SBP was equal to or greater than 135 mmHg or when the mean daytime DBP was equal to or greater than 85 mmHg according to the report of JNC 7 and ESH and ESC guidelines for hypertension [4,5].
C) Diagnosis and classification of hypertension
Hypertension was defined independently by clinic BP and 24-hour ambulatory BP, and the subjects were classified into four groups without regard to previous diagnosis and medication of hypertension. First, the true normotension group was defined as subjects who were normotensive according to both methods; second, the sustained hypertension group was defined as subjects who were hypertensive by both methods; third, the masked hypertension group was defined as subjects who were normotensive by clinic or office BP but hypertensive by ambulatory BP; and fourth, the white coat hypertension group was defined as subjects who were hypertensive by clinic or office BP but normotensive by ambulatory BP.
III. Statistical Analysis
Categorical variables were represented as frequency and percentage, and continuous variables as mean ± standard deviation (SD). Categorical variables were compared by chi-square test or Fisher's exact test, while continuous variables were compared by t-test. With masked hypertension as a dependent variable, a multiple logistic regression analysis was conducted to identify levels of correlation and impact between individual variables considered. In first analysis, gender, age, clinic BP, total cholesterol, and smoking were adjusted, and in second analysis was conducted by gender. All data were analyzed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
I. General Characteristics of Subjects
Among a total of 121 subjects, there were 87 (71.9%) males and 34 (28.1%) females. The mean age across subjects was 35.1±9.3 years, while the mean male age was 37.3±8.0 years and the mean female age was 29.4±10.0 years. And 52 subjects (43.0%) were in their 30s, while 47 (54.0%) males were in their 30s and 25 (73.5%) females were in their 20s. And the other characteristics of subjects were shown in Table 1.
II. Frequency and Proportion of Hypertension According to Method of Measurement
Of the 121 total subjects, 37 (30.6%) subjects were hypertensive by clinic BP, and 65 (53.7%) subjects were hypertensive by ambulatory BP. Therefore, the proportion of hypertension detected significantly differed between the two measurement methods (p<0.01). According to age group, 4 (11.1%) subjects in their 20s were hypertensive by clinic BP, and 11 (30.6%) subjects were hypertensive by ambulatory BP, a difference that was significant (p<0.05). Nineteen (36.5%) subjects in their 30s were hypertensive by clinic BP, and 32 (61.5%) subjects in their 30s were hypertensive by ambulatory BP, another significant difference (p<0.05). For subjects in their 40s and 50s, the frequencies of hypertension detected by the two measurement methods did not significantly differ (Table 2).
III. Classification of Hypertension According to Clinic BP and Ambulatory BP
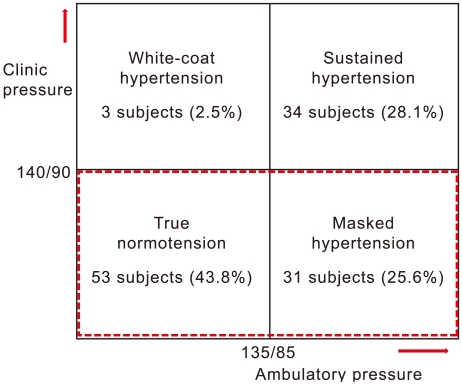
When subjects were classified into four groups according to clinic BP and ambulatory BP, 53 (43.8%) subjects were classified in the true normotension group, 34 (28.1%) subjects were classified in the sustained hypertension group, 31 (25.6%) subjects were classified in the masked hypertension group, and three (2.5%) subjects were classified in the white-coat hypertension group (Figure 1). There were 4 subjects under medication among 14 (11.6%) subjects who had been diagnosed with hypertension, and one of them were white-coat hypertension and 3 other subjects were sustained hypertension.
IV. Characteristics of the True Normotension Group and the Masked Hypertension Group
With regard to general characteristics, the proportion of males was significantly higher in the masked hypertension group than in the true normotension group (p<0.001), and the proportion of current smokers was significantly higher in the masked hypertension group (p<0.05)(Table 3).
With regard to clinical or biomedical characteristics, the daytime ambulatory SBP was significantly higher in the masked hypertension group (141.1±8.2 mmHg) than in the true normotension group (122.9±6.3 mmHg)(p<0.001), and the daytime ambulatory DBP was significantly higher in the masked hypertension group (90.4±6.4 mmHg) than in the true normotension group (77.8±5.2 mmHg)(p<0.001). The clinic SBP was significantly higher in the masked hypertension group (126.1±8.2 mmHg) than in the true normotension group (116.4±10.6 mmHg)(p<0.001), and the clinic DBP was significantly higher in the masked hypertension group (77.0±6.3 mmHg) than in the true normotension group (69.0±7.1 mmHg)(p<0.001). In addition, the waist circumference was significantly higher in the masked hypertension group than in the true normotension group (p<0.001). Body mass index (BMI), total triglyceride, and low density lipoprotein were significantly higher in the masked hypertension group than in the true normotension group (p<0.005)(Table 4).
V. Masked Hypertension Related Factors
Independent determinants of masked hypertension were identified by multiple logistic regression analysis. Compared with true normotension, the related factors of masked hypertension were male gender (OR, 10.7; 95% CI, 1.41 to 81.09), aging one year (OR, 0.88; 95% CI, 0.78 to 0.99), clinic BP 120-129/80-84 mmHg (OR, 8.42; 95% CI, 1.51 to 46.82), clinic BP 130-139/85-89 mmHg (OR, 12.14; 95% CI, 1.80 to 81.85), smoking (OR, 5.51; 95% CI, 1.15 to 26.54), and increase of total cholesterol 1 mg/dL (OR, 1.05; 95% CI, 1.02 to 1.08).
Most of the females included in our sample were in their 20s, and the frequency of masked hypertension in females was very low. Therefore, in some analyses we controlled for gender. In males alone, the related factors of masked hypertension were clinic BP 120-129/80-84 mmHg (OR, 15.07; 95% CI, 1.55 to 146.19), clinic BP 130-139/85-89 mmHg (OR, 17.16; 95% CI, 1.56 to 189.45), smoking (OR, 11.61; 95% CI, 1.52 to 88.62), and increase of total cholesterol 1 mg/dL (OR, 1.05; 95% CI, 1.01 to 1.09)(Table 5).
DISCUSSION
In Korea, the prevalence of hypertension has been reported 24.9% for adults over 30 years of age [3]. But, masked hypertension has been excluded because diagnostic procedures of hypertension were usually made according to clinic BP in most studies.
In the present study, the frequency of masked hypertension was as high as 25.6%, even in young healthy subjects. This is in agreement with the results of a previous study, in which the frequency of masked hypertension was reported to be 28.3% among subjects of precision inspection of BP in one Korean hospital [10]. The prevalence of masked hypertension has been reported to occur in about 9-24% of cases in studies conducted outside of Korea [7-9,13,17]. In our study, we defined hypertension as mean daytime 24-hour ambulatory BP over 135/85 mmHg, and therefore, there is a potential for controversy because the standard definition of hypertension is mean daytime BP of 130/80-135/85mmHg. Such definitions vary between studies.
In addition, as self measurement sphygmomanometers become more common, self or home BP has been providing inexpensive information for masked hypertension in many studies. But, it has been reported that most people do not understand how to take accurate BP measurements themselves [18]. Au contraire, the use of 24-hour ambulatory BP monitoring has numerous advantages over clinic BP or self-measurement BP. Data reflecting continuous changes in BP may be collected while subjects carry on with their daily activities and are not affected by observer error [19]. In addition, it can enable to monitor presence or absence of nocturnal BP dip to predict patient prognosis [20].
Clinic or office BP measurements are often subject to the white-coat effect, which was first reported by Mancia et al. [21] in 1987. The prevalence of white-coat hypertension differ between studies, and range between 20-75% [22-24]. In the present study, the frequency of white-coat hypertension was 2.5%, and relatively low than previous studies. But, we believe that the discrepancy between our study and previous studies may be explained by the fact that most prior studies were performed in elderly hospital patients who were considered to have hypertension.
Masked hypertension-related factors, such as current smoking, drinking, obesity, male gender, family history of hypertension, diabetes, hypertension medication, and high clinic or office BP values, have been reported [25,26]. But, in other study, no difference in frequency between treated and untreated patients have been reported [7]. And younger people who have more physical activity will tend to have higher daytime BP [27]. In Korea, one study among subjects of precision inspection of BP at one hospital, it was reported that of the possible related factors, current smoking was the only significant factor [10]. Risk factors associated with masked hypertension were increased in this study in subjects with high normal clinic or office BP compared to subjects with normal BP, in males, in younger subjects, in smokers, and when cholesterol levels were higher.
We did not detect any associations between masked hypertension and alcohol use, probably because 94.2% of the subjects reported using alcohol.
We found that occupational stress was not associated with masked hypertension in this study. Some previous studies have reported that the associations between masked hypertension and cardiovascular disease remains unclear [28,29], while others have reported cases of induced cardiovascular disease in the context of physiological reactions, such as increases in BP and hormones due to occupational stress [30]. Further prospective studies for the exploration of any causal relationships are warranted.
Fasting blood sugar and BMI, waist measurement, and liver function tests revealed significant differences in univariate analysis; however, there were no significant associations in logistic regression analysis.
We are unaware of any previous studies of cardiovascular disease in Korea comparing subjects with masked hypertension, normotension, and sustained hypertension. However, it has been reported that cases of atherosclerosis, which progresses without symptoms during the early disease period and often develops into myocardial infarction or cardiac arrest, can be predicted during the early disease period by tests that identify structural and functional changes of the artery, such as intimal-medial thickness of the carotid artery (cIMT) and pulse wave velocity (PWV) [31,32]. We hypothesized that it is possible to compare subjects with masked hypertension, normotension, and sustained hypertension.
This study has the following limitations. First, hypertension was diagnosed when the mean 24-hour ambulatory daytime BP was 135/85 mmHg or greater, but this definition may be controversial. Second, the number of patients with hypertension in our sample may have been under diagnosed by mean 24-hour ambulatory daytime BP, such that we could not evaluate any organ damage related to changes in daytime BP and whether or not BP decreased during the night. This shortcoming may be remedied by collecting follow-up measurements. Third, the number of subjects included in the present study was small, and our sample was relatively young. Follow-up studies or supplementation through large-scale community surveys are warranted.
We observed a rate of masked hypertension of 25.6% among the healthy young workers included in this study. In cases that changes in clinic BP are variable, it would be beneficial to make early diagnoses by measurement of 24-hour ambulatory BP in order to initiate interventions, such as consultations with cardiologists for evaluation of the heart, or initiation of efforts to stop smoking. Identification of the prevalence rate and risk factors of masked hypertension in communities is of great importance for the prevention and management of cardiovascular diseases.
ACKNOWLEDGEMENTS
This work was supported by the Korea Research Foundation Grant funded by the Korean Government (KRF-2008-331-E00082).
Notes
The authors have no conflicts of interest with the material presented in this paper.
This article is available at http://jpmph.org/.