Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 57(1); 2024 > Article
-
Original Article
Comorbid Conditions in Persons Exposed to Ionizing Radiation and Veterans of the Soviet–Afghan War: A Cohort Study in Kazakhstan -
Saule Sarkulova1

 , Roza Tatayeva2
, Roza Tatayeva2 , Dinara Urazalina3
, Dinara Urazalina3 , Ekaterina Ossadchaya2
, Ekaterina Ossadchaya2 , Venera Rakhmetova1
, Venera Rakhmetova1
-
Journal of Preventive Medicine and Public Health 2024;57(1):55-64.
DOI: https://doi.org/10.3961/jpmph.23.333
Published online: November 1, 2023
- 902 Views
- 79 Download
1Department of Internal Diseases with Course of Nephrology, Hematology, Allergy and Immunology, Astana Medical University, Astana, Kazakhstan
2Department of General Biology and Genomics, L. N. Gumilyov Eurasian National University, Astana, Kazakhstan
3Central Clinical Hospital for Veterans of the Patriotic War of the Ministry of Health of the Republic of Kazakhstan, Astana, Kazakhstan
- Corresponding author: Saule Sarkulova, Department of Internal Diseases with Course of Nephrology, Hematology, Allergy and Immunology, Astana Medical University, Beibitshilik Street 49/A, Astana 010000, Kazakhstan E-mail: ssarkulova@yahoo.com
Copyright © 2024 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives:
- This study investigated the prevalence and characteristics of comorbid conditions in patients exposed to ionizing radiation and those who were involved in the Soviet–Afghan war.
-
Methods:
- This study analyzed the frequency and spectrum of morbidity and comorbidity in patients over a long-term period (30-35 years) following exposure to ionizing radiation at the Semipalatinsk nuclear test site or the Chornobyl nuclear power plant, and among participants of the Soviet–Afghan war. A cohort study, both prospective and retrospective, was conducted on 675 patients who underwent comprehensive examinations.
-
Results:
- Numerical data were analyzed using the Statistica 6 program. The results are presented as the mean±standard deviation, median, and interquartile range (25-75th percentiles). The statistical significance of between-group differences was assessed using the Student t-test and Pearson chi-square test. A p-value of less than 0.05 was considered statistically significant. We found a high prevalence of cardiovascular diseases, including hypertension (55.0%) and cardiac ischemia (32.9%); these rates exceeded the average for this age group in the general population.
-
Conclusions:
- The cumulative impact of causal occupational, environmental, and ultra-high stress factors in the combat zone in participants of the Soviet–Afghan war, along with common conventional factors, contributed to the formation of a specific comorbidity structure. This necessitates a rational approach to identifying early predictors of cardiovascular events and central nervous system disorders, as well as pathognomonic clinical symptoms in this patient cohort. It also underscores the importance of selecting suitable methods and strategies for implementing treatment and prevention measures.
- To date, the problem of how occupational and environmental factors influence the development of comorbidities remains understudied. The increase in multiple diseases with age (i.e., comorbidities) is widely discussed in the literature and is closely linked to the demographic situation in many countries. This problem is particularly relevant for cardiology patients due to the high prevalence of cardiovascular diseases and their pathophysiological association with damage to various organs [1]. This problem manifests both as an increase in the number of patients with comorbidities, on the one hand, and an increase in the overall comorbidity index in individual patients, on the other. Ultimately, the presence of comorbidities and high cardiovascular risk hinders adequate rehabilitation and is associated with polypharmacy, extended hospital stays, and the incidence of complications, disability, and mortality [2].
- Extensive research has been conducted on comorbidities. However, every medical and research domain inevitably has gaps that need more investigation, and the field of comorbidities is no exception. While numerous studies have explored the individual health impacts of ionizing radiation (IR) exposure and participatioln in military conflicts, there is a notable dearth of comprehensive research into the combined or cumulative effects of these occupational and environmental factors on comorbidities. The current literature often delves separately into the health outcomes of radiation exposure and those of war veterans. The intersection where both factors converge, potentially compounding health risks, remains underexplored.
- The increase in comorbidities with age, which primarily reflects involutional processes in the body, is the subject of many studies and publications [2]. Among the factors influencing comorbidities, in addition to age-related (i.e., involutional) factors, genetic, social, infectious, and iatrogenic factors have also been identified. However, the problem of comorbidities in persons exposed to IR, participants of the Soviet–Afghan war and participants of other regional military conflicts (Hungary, Czechoslovakia) has been little studied. This problem is particularly pertinent now, as the participants in military conflicts, the liquidators of the Chornobyl accident, the Army servicemen assigned to the Semipalatinsk nuclear test site, as well as those who lived in nearby territories during nuclear tests, are included in the older age category. Consequently, involutional processes, in addition to factors associated with special conditions in this cohort of patients, are naturally manifesting as systemic disorders of the body. Thirty-seven years have passed since the Chornobyl accident, 34 years since the end of the Soviet–Afghan war, and 32 years since the closure of the Semipalatinsk test site. Most clinical studies on the health status of participants in these tragic events were published in the short term—that is, in the first decades [3-6].
- Fewer studies have investigated the ongoing health impacts of these distant events in exposed individuals themselves. At present, researchers are mainly focusing on studying the consequences of IR in the descendants of individuals affected by the Semipalatinsk nuclear test site and the Chornobyl nuclear power plant [6,7]. In the Central Clinical Hospital for Veterans of the Patriotic War in Astana, Kazakhstan, veterans of the Great Patriotic War (i.e., World War II), participants in the Soviet–Afghan war, liquidators of the Chornobyl accident, and persons exposed to IR at the Semipalatinsk nuclear test site undergo inpatient treatment and rehabilitation. The purpose of this study was to analyze the prevalence rate and characteristics of comorbid conditions in patients exposed to IR and participants in the Soviet–Afghan war. Specifically, comprehensive examinations were conducted of patients upon admission to the hospital, morbidity and characteristics of comorbid conditions in patients were analyzed, and a statistical analysis was conducted to identify early predictors of cardiovascular diseases.
- Understanding the role of occupational and environmental factors in the development of comorbidities can pave the way for better preventive measures, early diagnosis, and holistic treatment strategies. Given the immense implications for public health, it is vital that this area receives more attention and resources in both research and policy domains.
INTRODUCTION
- A cohort study, both prospective and retrospective, was carried out among hospital patients who received inpatient treatment between 2017 and 2019. This study involved 675 patients. Upon admission to the hospital, all patients underwent comprehensive examinations, as follows:
- (1) Cardiovascular workups: electrocardiography (ECG), daily mobile telemetry ECG, echocardiography, ambulatory blood pressure monitoring, ultrasound of brachiocephalic vessels and arteries of the lower extremities, ultrasound of the abdominal cavity and small pelvis, and peak flowmetry. According to the indications, fibrogastroendoscopy, computed tomography, magnetic resonance imaging, and electroencephalography were performed. The following invasive methods were used according to the indications: coronary angiography, electrophysiological studies of the heart, and load tests (bicycle ergometry and 6 minutes of walking).
- (2) Biochemical laboratory tests: levels of bilirubin, aspartate transaminase, alanine transaminase, gamma-glutamyl transpeptidase, alkaline phosphatase, creatinine, glomerular filtration rate, urea, hormones (thyroid-stimulating hormone and free T4), antibody titer to thyroglobulin, glucose, glycemic profile, glycated hemoglobin, lipid profile (total cholesterol, low-density and high-density lipoprotein cholesterol, and thyroglobulin), and coagulation tests (international normalized ratio, prothrombin time, activated partial thromboplastin time).
- (3) Psycho-emotional assessments: the frequency, nature, and severity of psycho-emotional disorders (tests: MiniMult, VP Zaytsev).
- (4) Conventional risk factors were analyzed: smoking, alcohol intake, elevated body mass index (BMI), obesity, impaired glucose tolerance (IGT), hypercholesterolemia (HCH), low physical activity, and hyperuricemia. A BMI of 30.0 kg/m 2 was taken as an indicator of obesity.
- The exclusion criteria were acute coronary syndrome, malignant neoplasms, and psychiatric illness/disorders.
- Statistical Analysis
- Digital data were processed using the Statistica 6 program and presented as mean±standard deviation, median, and interquartile range (IQR; 25th to 75th percentiles). The statistical significance of between-group differences was assessed using the Student t-test and Pearson chi-square test. A p-value of less than 0.05 was considered statistically significant.
- For a more detailed analysis of the prevalence and clinical characteristics, we divided all patients into three groups. Group I comprised 152 patients who were exposed to IR while serving at the Semipalatinsk test site, as well as individuals who resided in the surrounding areas of the Semipalatinsk test site during nuclear tests. All were males, with a median±SD age of 61.8±8.0 (IQR, 56-68) years. Group II consisted of 246 patients, all of whom were males involved in the cleanup of the Chornobyl accident, with a median±SD age of 58.3±7.6 (IQR, 52-63) years. Group III included 277 individuals, all male participants in the Soviet-Afghan war, with a median±SD age of 53.9±4.9 (IQR, 50-56) years.
- Ethics Statement
- All research was conducted with the consent of the patients and approved by the local ethical committee. The investigations were conducted in accordance with the rules of the Declaration of Helsinki, as revised in 2013. All participants were informed that their anonymity would be assured and received explanations of the purpose of the research, how their data would be utilized, and any associated risks. All participants consented to participate in the research.
METHODS
- An analysis of the entire patient cohort admitted to the therapy department during the study period revealed that cardiovascular diseases were the most prevalent. Arterial hypertension (HT) was diagnosed in 375 (55.6%) patients, while coronary artery disease was found in 223 (33.0%) patients, presenting as angina II-III functional class (FC), myocardial infarction, or ischemic cardiomyopathy. Cerebrovascular pathology was the second most common condition, affecting 461 patients (68.3%). This was complicated by stroke in 11.1% of cases and manifested as dyscirculatory encephalopathy (DEP) of the second degree in 73.7% of patients, and the third degree in 26.3% of patients. The study also noted a high prevalence of endocrine pathology, particularly disorders of lipid and carbohydrate metabolism. Obesity, predominantly of the visceral type, was observed in 467 (69.2%) cases, with 61.8% being of the first degree and 7.4% of the second degree. Diabetes mellitus was also common, with type 2 diabetes found in 149 (22.1%) patients, type 1 diabetes in 26 (3.9%) patients, and IGT in more than half (56.0%) of the patients. Diseases of the musculoskeletal system were also prevalent, particularly spinal osteochondrosis in 43.2% of patients and deforming osteoarthritis in 33.2% of patients. Gastrointestinal diseases were also common, with non-alcoholic fatty liver disease found in 32.8% of patients and chronic pancreatitis in 28.3% of patients.
- A comparative analysis showed significant differences in the prevalence spectrum among the studied groups. Among patients exposed to radiation at the Semipalatinsk test site (group I) and the Chornobyl nuclear power plant (group II), there was a notably high frequency of advanced-stage HT (stages 2-3; 67.8 and 55.5% of patients, respectively), and coronary artery disease (40.8 and 33.3%, respectively). We also identified a high prevalence of type 2 diabetes mellitus (23.7 and 18.3%, respectively). This factor correlates with a high prevalence of obesity. Specifically, 71.1% of patients in group I and 68.7% in group II had obesity of degrees I-II. Overall, metabolic syndrome, which includes visceral obesity, HCH, type 2 diabetes/IGT, and HT, and in some patients, hyperuricemia, was present in 21.1% of patients in group I and in 18.3% of cases in group II.
- These groups of patients often exhibited thyroid pathology, with occurrences in 21.7% and 22.3% of cases, respectively. The most common form was nodular goiter, found in 66.7% and 56.3% of these cases. Diffuse nodular goiter was less common, appearing in 8.6% and 5.4% of cases, while cystic formations were present in 24.7% and 38.3% of cases. The findings from these studies highlight a high frequency of peripheral vascular lesions: in 41.4% and 36.6% of patients, respectively, atherosclerosis of the brachiocephalic arteries, abdominal aorta, and lower extremity vessels were detected during examination. Additionally, clinical symptoms of Raynaud’s syndrome were identified in a subset of patients (5.3 and 4.5%).
- In contrast, in group III (Soviet–Afghan war participants), multifocal atherosclerosis (25.6%) with damage to the brachiocephalic vessels and arteries of the lower extremities was less common. Thyroid pathology, primarily in the form of cysticnodular formations with euthyroidism, was also significantly less prevalent (14.1%). As previously noted, a high frequency of HT was found in individuals exposed to IR. Concurrently, this study revealed a high incidence of complications (19.1%), particularly acute cerebrovascular accidents, especially among the Chornobyl accident liquidators (23.2%). Of particular interest is the fact that some patients experienced strokes without HT. From this, it can be inferred that in this category of patients exposed to IR, the clinical picture was dominated by signs of cerebrovascular pathology, primarily in the form of second-degree (and in some cases, third-degree) DEP. Psycho-emotional disorders with asthenic-neurotic syndrome, characterized by rapid fatigue, weakness, and sleep disorders, were also prevalent.
- In the cohort of patients studied who were exposed to IR, the most prevalent conditions were vascular pathologies, which presented clinically as HT, cerebrovascular diseases, and peripheral vascular lesions. However, in group III, which consisted of Soviet–Afghan war veterans, cardiovascular diseases were also common, with HT present in 55.9% of patients and coronary artery disease in 30.7%. These rates exceeded those of the general population. Despite this, the clinical presentation in these patients was dominated by signs of cerebrovascular pathology, resulting from injuries and contusions sustained during military operations. These manifested as signs of DEP of II-III degree, and in some patients, severe neurological symptoms, including convulsive syndrome (7.2%), dizziness, persistent headaches, and noise in the head. Psycho-emotional disorders, such as anxiety-depressive and neurasthenic syndromes, were also observed, with some cases exhibiting psychopathic, aggressive manifestations. The frequency of common conventional risk factors, including smoking, obesity, IGT, HCH, low physical activity, and hyperuricemia, was quite high across all three study groups, with no significant differences. Obesity was present in 71.1%, 68.7%, and 65.0% of patients in the 3 groups, respectively, while smoking was reported in 67.8%, 63.0%, and 60.6% of patients. IGT was found in 65.1%, 58.1%, and 52.3% of patients, and HCH in 28.9%, 25.1%, and 31.7%. It is clear that the health of the cardiovascular and nervous systems in the Chornobyl accident liquidators, those present at the nuclear test site, and war veterans was influenced not only by the absolute values of IR, injuries, concussions, and extreme stress situations in the war zone, but also by age, constitutional features, lifestyle, and the presence of common risk factors.
- Taking into account the common presence of multisystemic disease in the research cohort, the authors analyzed comorbidities in patients with the most common cardiovascular pathologies. Specifically, 357 patients with ischemic heart disease, angina pectoris (FC II-III) and myocardial infarction (19.9%) were compared (Table 1). In group I (patients with coronary artery disease who received IR at the Semipalatinsk test site), the most common comorbidities were HT (89.9%) and cerebrovascular pathology in the form of second-degree to third-degree DEP (87.2%).
- This was followed by metabolic disorders: obesity, predominantly visceral (76.1%) and type 2 diabetes (26.6%), and lesions of the musculoskeletal system (36.7%). Notably, peripheral vascular lesions were highly frequent, appearing in 46.8% of cases. Thyroid disease was present in 24.8% of cases, with a quarter of these showing an increase in the thyroglobulin autoantibody titer. In group II, consisting of those liquidators of the Chornobyl accident, coronary artery disease most frequently co-occurred with HT (93.2%) and cardiovascular disease in the form of DEP (83.8%). Peripheral vascular lesions were present in 45.3% of cases, and thyroid disorders in 30.8%. Additionally, one-third of this group (30.5%) exhibited an increased titer of thyroglobulin antibodies.
- Furthermore, in this group of patients with coronary artery disease, the following conditions were also frequently observed: osteoarthritis (28.2%) and type 2 diabetes (25.6%).
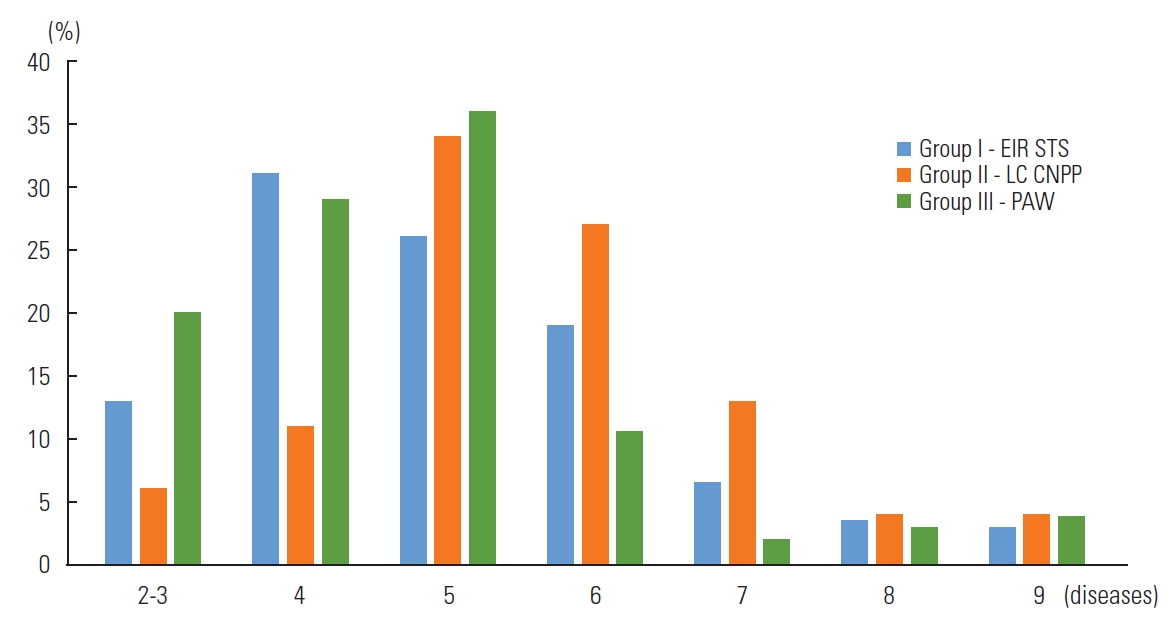
- An analysis of clinical observations showed that cardiovascular disease held a significant place in the comorbidity patterns of patients with coronary artery disease who were war veterans (group III). In this group, cardiovascular disease was present in 100% of cases, with all patients diagnosed with second-degree or third-degree DEP (Table 1). The distinctiveness of comorbidities in war veterans was not only due to the high frequency of central nervous system damage from injuries and concussions, but also the severity of cerebrovascular syndrome (conditions affecting blood flow to the brain). Third-degree DEP was observed in 21.4% of cases, while neuropsychiatric disorders were present in 27.5%. HT was the second most common condition in this group, affecting 82.4% of patients. Osteoarthritis was the third most common, affecting 35.8% of patients, and type 2 diabetes was observed in 18.3% of patients. Notably, a high prevalence of obesity was observed across all 3 patient groups (76.1, 70.9, and 69.5%, respectively). In war veterans with coronary artery disease, the prevalence of thyroid disease was 12.2%, and peripheral vascular lesions were present in 23.7% of cases, which is significantly lower than in groups of patients exposed to radiation. The authors analyzed the degree of comorbidity in the studied groups (Figure 1).
- In group I (patients exposed to IR at the Semipalatinsk test site), the most common number of comorbidities was 4 (31.7%), followed in descending order by 5 diseases (26.0%), 6 (18.7%), and 7 or more (12.2%). Among the liquidators of the Chornobyl accident (group II), the most common number of comorbidities was 5 (33.8%), while 27.3% of them had 6 pathologies and 20.7% had 7 or more diseases.
- Among war veterans, the most common number of comorbidities was 5, followed by 6 (10.5%) and 7-9 (8.4%). The mean number of comorbidities in each group was 4.57, 4.61, and 4.74, respectively.
RESULTS
- Exposure to IR and involvement in local wars can have significant impacts on both physical and mental health. When these factors coexist or when individuals are exposed to both, the complexity of potential health issues increases. Studying comorbid conditions in these individuals is crucial for addressing their unique healthcare needs. The findings of a cohort study conducted on the general population of patients seen at veterans’ hospitals suggested that the overall comorbidity structure aligns with the indices for this entire age group [2]. Concurrently, the authors’ research also identified some disparities. Specifically, the prevalence of HT was 55.6% and that of coronary ischemia (CI) was 32.9%, exceeding the rates observed in the general population, where the prevalence of HT ranges from 39% to 42% and that of CI from 10% to 20% [5,8]. Numerous clinical studies have demonstrated an elevated risk of developing cardiovascular diseases, including HT and coronary heart disease, among individuals exposed to radiation [8-11].
- The second most prevalent condition in this study was cerebrovascular disease, specifically DEP, which accounts for 68.3% of cases. This was often complicated by stroke (11.1%) in the absence of HT. The sequence of disease incidence generally aligned with that of the average population. These findings provide a foundation for a more detailed examination of the incidence structure within this cohort, considering causal factors. A comparative analysis revealed significant differences in the comorbidity structure of the groups studied. For instance, in patients with coronary artery disease who were exposed to radiation at the Semipalatinsk nuclear test site and the Chornobyl nuclear power plant, HT was the most prevalent in the long-term, mirroring the general population [5,8]. However, the comorbidity structure diverged significantly beyond this. Cerebrovascular pathology, specifically second-degree to third-degree DEP became less prominent. These patients also exhibited a relatively high incidence of peripheral vascular lesions, with multifocal atherosclerosis (46.8, 45.3%, respectively) and thyroid pathology (24.8, 30.8%, respectively), primarily characterized by hypofunction and an increased titers of thyroglobulin antibodies. Notably, among the Chornobyl accident liquidators, thyroid disorders ranked fourth. Numerous studies have confirmed the high frequency of thyroid lesions in individuals exposed to low doses of radiation [3,4].
- Damage to the endothelium of small vessels, leading to stromal fibrosis and a decrease in thyroid function, is believed to be the primary mechanism behind the development of post-radiation hypothyroidism [12,13]. In nearly half of the two groups studied (46.8, 45.3%, respectively), ischemic heart disease was found in conjunction with multifocal atherosclerosis. The atherogenic effect of low-dose radiation exposure is supported by numerous studies [14]. Therefore, a common characteristic among patients exposed to IR, and a defining feature of comorbidity in this patient category, is the high frequency of coronary artery disease associated with HT, cardiovascular disease, peripheral vascular and thyroid lesions. This is in contrast to the general population indicators. In a large-scale, population-based study of comorbid pathology with cardiovascular diseases in the United States, it was demonstrated that diabetes mellitus (around 40.0%), arthritis (40.6-45.6%), and anemia (38.7-51.2%) were most commonly observed. Nearly 1 patient in 4 patients had chronic kidney disease, cataracts, chronic obstructive pulmonary disease, or depression [3]. Numerous studies [15] indicate that the general population incidence of obesity and diabetes in patients with coronary artery disease ranges from 28% to 44%. However, the observed frequency of obesity and coronary artery disease association in our study was significantly higher (76.1, 70.9, and 69.5%, respectively). Concurrently, lipid metabolism disorders, with degree I-II obesity, were most commonly observed in groups of individuals exposed to radiation. The occurrence of lipid metabolism disorders and the development of obesity due to low-dose radiation exposure have been corroborated by other authors’ studies.
- Numerous clinical and experimental studies have indicated generalized lesions of the microcirculatory bed vessels in individuals exposed to IR [14-16]. Other researchers have found similar pathomorphological changes in the vessels, such as vasculitis and microvascular disorders, which play a significant role in atherogenesis. Many authors have suggested that under the influence of multiple small doses of radiation, genome instability develops. This is a genetic effect triggered by free radical mechanisms, which activate chain reactions of lipid peroxidation and increase the production of reactive oxygen species, while decreasing the regulatory function of endothelial nitric oxide synthetase [7,17]. The present study demonstrated the systemic nature of these lesions, resulting in a complex specific comorbidity structure in patients over the long term following exposure to IR. The analysis of clinical observations and experimental data supports the hypothesis of the biological effect of low doses of radiation on tissues with slow cellular renewal, which are not considered responsible for the immediate outcome of irradiation [18]. These tissues primarily include endothelial cells, the main structural and functional element of the microcirculatory bed. Endothelial dysfunction can lead to the development of HT and contribute to the progression of atherosclerosis. Japanese researchers have reported a high prevalence of arterial HT and dyslipidemia among residents of areas evacuated after the Fukushima accident [7].
- In domestic studies of the consequences of the actions of the Semipalatinsk landfill, a high prevalence of arterial HT, coronary heart disease, and dyslipidemia has been identified. Grosche et al. [18] also highlighted the high mortality rate from circulatory system diseases among those exposed to radiation at the Semipalatinsk test site. This finding is corroborated by other studies, which have found a high incidence of vascular lesions in this group over the long term following IR exposure, including arterial HT, cerebrovascular diseases complicated by stroke, and multifocal atherosclerosis. There is a notable lack of clinical data in both domestic and international literature regarding the study of cerebrovascular pathology among those exposed to radiation [19,20]. However, as other studies have demonstrated, cerebrovascular lesions are not only frequent but also significant in terms of the clinical characteristics of patients. Ungvari et al. [21] identified microvascular endothelial lesions in the brain. Most research has focused on the study of neuropsychiatric status and autonomic dysfunction [22].
- The high frequency and severity of cerebrovascular diseases observed in this study may be attributed to the long-term period (25-30 years) of the study following radioactive exposure. During this time, pathophysiological processes and regulatory system disruptions led to a new clinical situation (somatic pathologies and their unique combinations). Currently, clinical research involving Soviet–Afghan war participants is largely under-studied in both domestic/Russian and international literature. However, this patient group, often presenting with severe combined pathology, warrants close scrutiny, comprehensive study of their clinical status, and the development of management algorithms and treatment and rehabilitation methods. In this patient category, as with the general population, there is a high prevalence of constitutional and metabolic risk factors. Traumatic stress further increases the risk of developing cardiovascular comorbidities [23].
- The pathogenetic relationship of many diseases associated with long-term periods following IR still requires in-depth study. Most published works have focused on short-term research, including the co-occurrence pattern of various pathologies. For instance, according to Porovsky et al. [15], an examination of the liquidators involved in the aftermath of the Chornobyl nuclear power plant accidents revealed that, within a span of 10-14 years, each liquidator was diagnosed with an average of 8.3 diseases, ranging from 5 to 13. This frequency of syntropy is notably higher than the results found in our study [24]. However, it is important to note that our long-term study (34 years post-incident) only included liquidators who survived, thus skewing our sample towards those with a more favorable prognosis. Our findings suggest that vascular disorders are systemic in nature in the long-term aftermath of IR, with a particular emphasis on lesions of the cerebral vessels and the central nervous system. In some instances, strokes developed without arterial HT (17.1%). This perspective is also supported by other researchers [25,26].
- Researchers have evaluated various comorbidity indices proposed for predicting mortality, disease severity, and disability, primarily aimed at assessing economic costs. However, the unique structure of pathology associations in patients is not encompassed within these proposed indices. Given this, it appears necessary to develop an appropriate diagnostic standard, along with additional markers for severity assessment and prognosis, for this patient category [27,28].
- In conclusion, it is crucial to understand the comorbid conditions in individuals exposed to IR and veterans of regional conflicts. Their unique experiences and exposures require specialized healthcare strategies and a more profound understanding of potential health challenges. The knowledge gained from these studies can significantly influence healthcare policies and interventions designed to meet their specific needs.
- Every research or study endeavor inherently has its own set of limitations. It is vital to understand these limitations for the appropriate interpretation of the findings and recommendations. One such limitation is recall bias. Particularly in retrospective studies, participants may not accurately remember past events or exposures. If participants or subjects are not selected randomly, inherent differences may exist in the groups being compared, which can lead to skewed results. This study recruited patients who passed a preliminary examination and were then further selected based on specific characteristics. While it may seem that recognizing a study’s limitations could undermine the research, the reality is quite the opposite. Acknowledging and understanding these constraints provides context, ensuring that findings are interpreted correctly and with due caution. It also provides guidance for future research, suggesting areas where further studies or different methodologies might yield clearer insights.
- The findings of this study demonstrate that the morbidity structure in the long-term period for the cohort of patients exposed to specific causal factors, such as IR and stressful military conflict situations, significantly differs from general population indicators. While cardiovascular diseases (arterial HT, coronary heart disease) are also prominent, cerebrovascular diseases are more prevalent, often manifesting in severe forms (second- to third-degree DEP) with frequent complications, such as strokes [29-31]. A distinctive feature of this cohort is the relatively high frequency of peripheral vascular lesions, multifocal atherosclerosis, and thyroid pathology. The significant differences observed in the comorbidity structure among subgroups of patients with coronary heart disease suggest a causal influence of professional, man-made, environmental, and stress factors. Long-term exposure to radiation results in comorbidities characterized by a predominance of generalized vascular lesions (multifocal atherosclerosis, strokes, cerebrovascular disease), categorizing patients with cardiovascular diseases in this cohort as high and very high cardiovascular risk. In the context of ultra-high stress situations, injuries, and contusions experienced by war veterans, central nervous system lesions become more prominent than cardiovascular diseases in the comorbidity structure. These include second-degree and third-degree DEP, frequent strokes, and neuropsychiatric disorders [32].
- This patient cohort commonly exhibits behavioral, constitutional, and metabolic factors. When combined with specific factors, these significantly impact the development of their comorbidity. Summarizing the results of this research and the views of numerous authors, it can be asserted that understanding the impact of professional and environmental factors, particularly those related to IR, as well as the ultra-high stress situations encountered in war zones, is crucial in shaping a specific comorbidity structure. This understanding necessitates a rational approach to identifying early predictors of disorders in the cardiovascular and central nervous systems. Recognizing pathognomonic clinical symptoms in this patient cohort can assist clinicians in devising appropriate methods and strategies for therapeutic and preventive measures.
- The distinctive morbidity patterns that emerge from exposure to IR and stressful wartime situations pose distinct challenges to patient management and broader healthcare strategies. Grasping these implications is crucial for delivering optimal care to affected individuals and ensuring that healthcare systems are sufficiently prepared to meet their needs. A holistic approach is worth considering, where patients can access oncologists, endocrinologists, cardiologists, and mental health professionals all within the same care center. Additionally, due to heightened cancer risks, regular screenings (such as thyroid ultrasounds or mammograms) are vital for early detection of malignancies [33,34]. Addressing the implications of these specific morbidity patterns necessitates a multi-dimensional, patient-centric approach. Such an approach is not solely about treating diseases, but also about providing comprehensive care that tackles physical, emotional, and social challenges, with the ultimate goal of enhancing the quality of life and longevity of affected individuals.
- The preliminary results presented in this paper focus on the characteristics of comorbid conditions in patients who have experienced long-term exposure to IR and in war veterans. These findings lay the groundwork for a more detailed exploration of comorbidities within this group. The authors believe it is necessary to conduct a separate, in-depth investigation into how comorbidities influence the cardiovascular risk of these diseases and the prognosis of patients. The phenomenon of comorbid conditions presents a complex array of challenges and opportunities for research. A multidisciplinary approach, incorporating perspectives from medicine, sociology, economics, and technology, is crucial to fully understand and manage the intricacies of comorbidities.
DISCUSSION
-
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
-
Funding
None.
-
Author Contributions
Conceptualization: Sarkulova S, Tatayeva R. Data curation: Tatayeva R. Formal analysis: Urazalina D, Tatayeva R, Rakhmetova V, Ossadchaya E. Funding acquisition: None. Methodology: Rakhmetova V. Project administration: Tatayeva R. Visualization: Rakhmetova V. Writing – original draft: Sarkulova S, Tatayeva R. Writing – review & editing: Urazalina D, Ossadchaya K, Rakhmetova V.
Notes
Acknowledgements
| Comorbid pathology | Exposed to ionizing radiation at the Semipalatinsk test site | Liquidators of the consequences of the Chornobyl accident | Veterans of the Soviet–Afghan war | Total (n = 357) | Assessing differences (χ2) |
|---|---|---|---|---|---|
| Arterial hypertension | 98 (89.9) | 109 (93.2) | 108 (82.4) | 315 (88.2) | 0.86 |
| Cerebrovascular disease | 95 (87.2) | 98 (83.8) | 131 (100) | 324 (90.6) | 2.01 |
| Dyscirculatory encephalopathy, second-degree | 93 (85.3) | 96 (82.1) | 103 (76.8) | 292 (81.8) | 0.33 |
| Dyscirculatory encephalopathy, third-degree | 2 (1.8) | 2 (1.7) | 28 (21.4) | 32 (9.0) | 35.42*** |
| Peripheral vessel disease | 51 (46.8) | 53 (45.3) | 35 (26.7) | 139 (38.9) | 8.08* |
| Obesity | 83 (76.1) | 83 (70.9) | 91 (69.5) | 257 (72.0) | 0.40 |
| Type 2 diabetes mellitus | 29 (26.6) | 30 (25.6) | 24 (18.3) | 83 (23.2) | 2.18 |
| Acute disorders of cerebral circulation | 14 (12.8) | 20 (17.1) | 8 (6.1) | 42 (11.8) | 6.47* |
| Thyroid disease | 27 (24.8) | 36 (30.8) | 16 (12.2) | 79 (22.1) | 10.11*** |
| Osteoarthritis | 38 (36.7) | 33 (28.2) | 47 (35.8) | 126 (35.3) | 1.69 |
| Chronic pancreatitis | 15 (13.7) | 17 (14.5) | 11 (8.4) | 43 (12.0) | 2.32 |
| Chronic obstructive pulmonary disease | 14 (12.8) | 13 (11.1) | 9 (6.9) | 36 (10.1) | 2.28 |
| Non-alcoholic fatty liver disease | 9 (8.3) | 10 (8.5) | 9 (6.9) | 28 (7.8) | 0.26 |
| Chronic kidney disease | 4 (3.6) | 2 (1.7) | 9 (6.9) | 15 (4.2) | 4.02 |
| Other | 23 (21.1) | 20 (17.1) | 14 (10.7) | 57 (16.0) | 4.17 |
- 1. Vance D, Larsen KI, Eagerton G, Wright MA. Comorbidities and cognitive functioning: implications for nursing research and practice. J Neurosci Nurs 2011;43(4):215-224. https://doi.org/10.1097/JNN.0b013e3182212a04ArticlePubMed
- 2. Ekusheva EV. Elderly patient with comorbid pathology in the practice of a cardiologist. RMJ Med Rev 2018;11(2):26-29. (Russian)
- 3. Pokrovsky YV, Tetenev FF. Comorbidity in medical practice. Sib Med Rev 2015;4: 5-10. (Russian)
- 4. Kabdrakhmanov K. Human consequences of nuclear weapons tests in Kazakhstan. Almaty: Olke; 2003. p. 46 (Russian)
- 5. Nikiforov AM. Medical consequences of the Chornobyl accident. Saint Petersburg: Petersburg State University; 2005. p. 229-233 (Russian)
- 6. Rudnitskiy VA, Semke VY, Garganeeva NP. Neuro-mental disorders associated with concomitant somatic disorders in Chernobyl accident emergency workers. Russ Psychiatr J 2010;6: 34-40. (Russian)
- 7. Suskov II, Kuz’mina NS, Suskova VS, Baleva LS, Sipiagina AE. The problem of induced genome instability as the basis of the increased morbidity in children exposed to low-intensity radiation at low doses. Radiats Biol Radioecol 2006;46(2):167-177. (Russian)PubMed
- 8. Raghunathan D, Khilji MI, Hassan SA, Yusuf SW. Radiation-induced cardiovascular disease. Curr Atheroscler Rep 2017;19(5):22. https://doi.org/10.1007/s11883-017-0658-xArticlePubMed
- 9. Stepanova IeI, Berezovs’kyĭ VIa, Kolpakov IE, Kondrashova VH, Lytvynets’ OM. Endothelium dependent vascular reactivity and autonomic homeostasis in children living in radiation-contaminated areas. Lik Sprava 2013;(2):22-38. (Ukrainian)
- 10. Azizova T, Briks K, Bannikova M, Grigoryeva E. Hypertension incidence risk in a cohort of Russian workers exposed to radiation at the Mayak Production Association over prolonged periods. Hypertension 2019;73(6):1174-1184. https://doi.org/10.1161/HYPERTENSIONAHA.118.11719ArticlePubMed
- 11. Markabayeva A, Bauer S, Pivina L, Bjørklund G, Chirumbolo S, Kerimkulova A, et al. Increased prevalence of essential hypertension in areas previously exposed to fallout due to nuclear weapons testing at the Semipalatinsk test site, Kazakhstan. Environ Res 2018;167: 129-135. doi: https://doi.org/10.1016/j.envres.2018.07.016ArticlePubMed
- 12. Land CE, Kwon D, Hoffman FO, Moroz B, Drozdovitch V, Bouville A, et al. Accounting for shared and unshared dosimetric uncertainties in the dose response for ultrasound-detected thyroid nodules after exposure to radioactive fallout. Radiat Res 2015;183(2):159-173. https://doi.org/10.1667/RR13794.1ArticlePubMedPMC
- 13. Ron E, Brenner A. Non-malignant thyroid diseases after a wide range of radiation exposures. Radiat Res 201;174(6):877-888. https://doi.org/10.1667/RR1953.1Article
- 14. Lowe D, Raj K. Premature aging induced by radiation exhibits pro-atherosclerotic effects mediated by epigenetic activation of CD44 expression. Aging Cell 2014;13(5):900-910. https://doi.org/10.1111/acel.12253ArticlePubMedPMC
- 15. Porovsky YV, Tetenev FF. Factors of inflammation and the state of the microcirculatory bed in patients exposed to low doses of ionizing radiation. Bull New Med Technol 2012;18(2):358-361. (Russian)
- 16. Telkova IL. Cardiovascular disease manifestations in Chernobyl liquidators: 25 years later. Clinico-analytical review. Cardiovasc Ther Prev 2012;11(3):62-69. (Russian). https://doi.org/10.15829/1728-8800-2012-3-62-69Article
- 17. Chaizhunusova N, Madiyeva M, Tanaka K, Hoshi M, Kawano N, Noso Y, et al. Cytogenetic abnormalities of the descendants of permanent residents of heavily contaminated East Kazakhstan. Radiat Environ Biophys 2017;56(4):337-343. https://doi.org/10.1007/s00411-017-0717-2ArticlePubMed
- 18. Grosche B, Lackland DT, Land CE, Simon SL, Apsalikov KN, Pivina LM, et al. Mortality from cardiovascular diseases in the Semipalatinsk historical cohort, 1960-1999, and its relationship to radiation exposure. Radiat Res 2011;176(5):660-669. https://doi.org/10.1667/rr2211.1ArticlePubMedPMC
- 19. Semenova Y, Pivina L, Belikhina T, Manatova A, Abisheva A, Ainabekova E, et al. Mortality due to cerebrovascular accidents in East Kazakhstan over the period of 2013-2017. Eur J Public Health 2018;28(suppl_4):cky218.164. https://doi.org/10.1093/eurpub/cky218.164Article
- 20. Ivanov VK, Maksiutov MA, Chekin SIu, Petrov AV, Tsyb AF, Biriukov AP, et al. The radiation risks of cerebrovascular diseases among the liquidators. Radiats Biol Radioecol 2005;45(3):261-270. (Russian)PubMed
- 21. Ungvari Z, Podlutsky A, Sosnowska D, Tucsek Z, Toth P, Deak F, et al. Ionizing radiation promotes the acquisition of a senescence-associated secretory phenotype and impairs angiogenic capacity in cerebromicrovascular endothelial cells: role of increased DNA damage and decreased DNA repair capacity in microvascular radiosensitivity. J Gerontol A Biol Sci Med Sci 2013;68(12):1443-1457. https://doi.org/10.1093/gerona/glt057ArticlePubMedPMC
- 22. Pivina LM, Semenova YM, Rakhypbekov TK, Dyussupov AA, Belikhina TI, Manatova AM. Prevalence of depression in the offspring of people exposed to radiation in East Kazakhstan: Almira Manatova. Eur J Public Health 2017;27(suppl_3):ckx189.196. https://doi.org/10.1093/eurpub/ckx189.196Article
- 23. Krantz DS, Shank LM, Goodie JL. Post-traumatic stress disorder (PTSD) as a systemic disorder: pathways to cardiovascular disease. Health Psychol 2022;41(10):651-662. https://doi.org/10.1037/hea0001127ArticlePubMed
- 24. Ungvari Z, Pacher P, Csiszar A. Can simvastatin promote tumor growth by inducing angiogenesis similar to VEGF? Med Hypotheses 2002;58(1):858-856. https://doi.org/10.1054/mehy.2001.1465Article
- 25. Okassova AK, Ilderbayev OZ, Nursafina AZ, Zharmakhanova GM, Rakhimova BB, Yessilbaeva BT, et al. Evaluation of lipid peroxidation under immobilization stress in irradiated animals in experiment. Open Access Maced J Med Sci 2021;9(A):119-122. https://doi.org/10.3889/oamjms.2021.5781Article
- 26. Mel’nychuk DO, Hryshchenko VA. Exchange of bile pigments under the action of ecopathogenic factors on organism. Ukr Biochem J 2014;86(5):156. (Ukrainian)PubMed
- 27. Chulenbayeva L, Ilderbayev O, Suleymeneva D, Kaliyeva A, Kabdykanov S, Nurgaziyev M, et al. Prolonged inhalation exposure to coal dust on irradiated rats and consequences. ScientificWorldJournl 2022;2022: 8824275. https://doi.org/10.1155/2022/8824275Article
- 28. Stepanov V, Vagaitseva K, Kharkov V, Cherednichenko A, Bocharova A, Berezina G, et al. Forensic and population genetic characteristics of 62 X chromosome SNPs revealed by multiplex PCR and MALDI-TOF mass spectrometry genotyping in 4 North Eurasian populations. Leg Med (Tokyo) 2016;18: 66-71. https://doi.org/10.1016/j.legalmed.2015.12.008ArticlePubMed
- 29. Abil’dinova GZh, Kuleshov NP, Sviatova GS. Chromosomal instability parameters in the population affected by nuclear explosions at the Semipalatinsk nuclear test site. Russ J Genet 2003;39: 944-947. https://doi.org/10.1023/A:1025391109169Article
- 30. Ilderbayev O, Zharmakhanova G, Rakhyzhanova S, Musaynova A, Ilderbayeva G, Nursafina A, et al. Immune system response after immobilization stress in the background of ionizing radi-]\\ation. Trends Sci 2022;19(13):4637. https://doi.org/10.48048/tis.2022.4637Article
- 31. Salimova AZ, Kutuev IA, Khusainova RI, Akhmetova VL, Sviatova GS, Berezina GM, et al. Analysis of ethnogeographic groups of Kazakhs based on nuclear genome DNA polymorphism. Russ J Genet 2005;41: 794-800. https://doi.org/10.1007/s11177-005-0162-1Article
- 32. Chulenbayeva L, Ilderbayev O, Taldykbayev Z, Ilderbayeva G, Argynbekova A. Phytocorrection of immunological and biochemical changes in the combined impact of coal dust and high dose of radiation. Georgian Med News 2018;(Issue):141-150. (Russian)
- 33. Saade LJ, Tfayli A. Pneumonitis in non-small cell lung cancer patients receiving atezolizumab post chemo-radiation. Asian Pac J Cancer Prev 2023;24(3):737-740. https://doi.org/10.31557/APJCP.2023.24.3.737ArticlePubMedPMC
- 34. Ilderbayeva G, Zhetpisbaev B, Ilderbayev О, Taldykbayev Zh, Bekeeva S. Metabolic processes of organism in remote period after the combined effects of radiation and emotional stress. Georgian Med News 2016;(250):76-82. (Russian)
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


