Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(6); 2023 > Article
-
Original Article
Vaccination Status and In-hospital Mortality Among Adults With COVID-19 in Jakarta, Indonesia: A Retrospective Hospital-based Cohort Study -
Hotma Martogi Lorensi Hutapea1,2
 , Pandji Wibawa Dhewantara1
, Pandji Wibawa Dhewantara1 , Anton Suryatma1
, Anton Suryatma1 , Raras Anasi3
, Raras Anasi3 , Harimat Hendarwan1
, Harimat Hendarwan1 , Mondastri Korib Sudaryo2
, Mondastri Korib Sudaryo2 , Dwi Gayatri2
, Dwi Gayatri2
-
Journal of Preventive Medicine and Public Health 2023;56(6):542-551.
DOI: https://doi.org/10.3961/jpmph.23.360
Published online: October 30, 2023
- 969 Views
- 76 Download
1National Research and Innovation Agency, Jakarta, Indonesia
2Department of Epidemiology, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
3Institute of Health Policy Development, Ministry of Health of Indonesia, Jakarta, Indonesia
- Corresponding author: Hotma Martogi Lorensi Hutapea, National Research and Innovation Agency, Jl. M.H. Thamrin No. 8, Jakarta 10340, Indonesia E-mail: hotm002@brin.go.id
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- Prospective studies on vaccination status and mortality related to coronavirus disease 2019 (COVID-19) in low-resource settings are still limited. We assessed the association between vaccination status (full, partial, or none) and in-hospital mortality among COVID-19 patients at most hospitals in Jakarta, Indonesia during the Delta predomination wave.
-
Methods
- We conducted a retrospective cohort study among hospitalized COVID-19 patients who met the study criteria (>18 years old and admitted for inpatient treatment because of laboratory-confirmed severe acute respiratory syndrome coronavirus 2 infection). We linked individual-level data in the hospital admission database with vaccination records. Several socio-demographic and clinical characteristics were also analyzed. A Cox proportional hazards regression model was used to explore the association between vaccination status and in-hospital mortality in this patient group.
-
Results
- In total, 40 827 patients were included in this study. Of these, 70% were unvaccinated (n=28 543) and 19.3% (n=7882) died during hospitalization. The mean age of the patients was 49 years (range, 35-59), 53.2% were female, 22.0% had hypertension, and 14.2% were treated in the intensive care unit, and the median hospital length of stay across the group was 9 days. Our study showed that the risk of in-hospital mortality among fully and partially vaccinated patients was lower than among unvaccinated adults (adjusted hazard ratio [aHR], 0.43; 95% confidence interval [CI], 0.40 to 0.47 and aHR, 0.70; 95% CI, 0.64 to 0.77, respectively).
-
Conclusions
- Vaccinated patients had fewer severe outcomes among hospitalized adults during the Delta wave in Jakarta. These features should be carefully considered by healthcare professionals in treating adults within this patient group.
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection causes coronavirus disease 2019 (COVID-19), which has caused approximately 759 million cases and 6.8 million fatalities worldwide as of March 2023 [1]. In Indonesia, since the initial detection of COVID-19 in early March 2020, there have been over 6.7 million reported cases and 160 956 fatalities nationwide [2]. During the COVID-19 pandemic, various variants of SARS-CoV-2 (i.e., Alpha, Beta, Delta, and Omicron) emerged. Prior to the emergence of the Omicron variant, the Delta variant of SARS-CoV-2 was predominant in many countries, including Indonesia, leading to an increase in emergency visits, intensive care unit (ICU) occupancy, and a significant rise in infection rates and deaths [3]. Despite the World Health Organization’s recommended health measures for COVID-19, the health systems of many countries have been severely impacted by the pandemic [4]. Therefore, alternative strategies, such as the development of a COVID-19 vaccine with suitable effectiveness, were needed to alleviate the COVID-19-related burden in most countries.
- In 2021, several COVID-19 vaccines of varying effectiveness were developed by a number of countries. Some countries had the privilege of selecting a specific type of vaccine, such as mRNA vaccines (Moderna, Pfizer), recombinant vaccines (AstraZeneca), and subunit vaccines (Novavax) [5], but most developing countries had only Sinovac-CoronaVac, an inactivated vaccine that was developed earlier [6]. Evidence indicates that the efficacy of the Sinovac-CoronaVac vaccine against symptomatic (63.8%) and severe (75.3%) COVID-19 conditions caused by the Delta variant is lower among the fully vaccinated population [7], compared to Moderna, Pfizer, AstraZeneca, and Novavax, which have efficacies of 98.3%, 98.5%, 91.0%, and 82.0% respectively. Despite these varying levels of vaccine effectiveness, studies have shown that COVID-19 vaccines reduce mortality in hospitalized patients with moderate to severe diseases [8], decrease the hospital length of stay, increase home discharges [9], and reduce COVID-19-related mortality among treated patients [10]. Therefore, understanding the effectiveness of vaccines across different pathogen variants is crucial.
- Among the variants and subvariants of COVID-19, the Delta variant presented unique challenges to overcome [11]. Although information about the relationship between the COVID-19 vaccine and mortality is available from various countries [8], research evaluating the impact of the COVID-19 vaccine on in-hospital mortality during the Delta-dominant period in developing countries is still limited. This is particularly true for studies that use a cohort study approach in population settings. Therefore, this study aims to assess the effect of vaccination status on in-hospital mortality among a large number of COVID-19 patients in Jakarta, Indonesia, during the wave of Delta variant predominance.
INTRODUCTION
- Study Participants
- We conducted a retrospective cohort study by reviewing 138 out of 140 COVID-19 referral hospitals’ admission records between June 1, 2021 and September 30, 2021 when the Delta (B.1.617.2) variant was prevalent in Jakarta. The inclusion criteria for the study were patients aged 18 years and older who were admitted for inpatient treatment due to a laboratory-confirmed diagnosis of SARS-CoV-2 infection. Patients with significant missing information, such as discharge status, type of care, and vaccination history, were excluded. We evaluated the hospital records using an electronic application called Pcare, which is integrated with each hospital’s health information system in Jakarta. The Pcare application was developed by the Social Health Insurance Administration Body, which is responsible for registering health facilities and recording their services related to the COVID-19 vaccination program [12]. Jakarta was the epicenter of the SARS-CoV-2 infection in Indonesia, recording the highest number of COVID-19 cases during the period of this study [13].
- Measurements
- The study outcome was in-hospital mortality, which was defined as patients with COVID-19 who died in the hospital during inpatient treatment [14]. The study exposure was vaccination status, which was defined based on whether an individual had received 1 or more doses of a COVID-19 vaccine [15]. We classified patients as fully vaccinated if they received the second dose of any COVID-19 vaccine at least 14 days after the first dose, allowing for complete antibody production [16]. Patients were considered partially vaccinated if they received the first dose of a COVID-19 vaccine at least 7 days prior to hospital admission. Conversely, patients were deemed unvaccinated if they had not received any COVID-19 vaccines before hospitalization [17]. In this study, we used the date of hospital admission rather than the SARS-CoV-2 test date, as the latter information was not available in the Pcare records.
- The Pcare application contains unique, individual data on demographic variables such as age, sex, education, and occupation, as well as clinical characteristics. These include comorbidities, treatment, length of stay, outcome (whether deceased or discharged), hospitalization history (including dates of admission and discharge), diagnoses, and hospitalization outcomes such as ICU admission and invasive mechanical ventilation (IMV) [18]. Medical comorbidities for each patient were identified and classified according to the International Classification of Diseases 10th revision (ICD-10) clinical diagnosis codes [19]. Vaccination history was extracted from national electronic COVID-19 vaccine registry. We used a deterministic linkage approach to link the COVID-19 vaccine registry with Pcare data using a unique ID. Duplications and completeness of the records (e.g., identifier, date of hospitalization, discharge status, vaccination history) were checked.
- Statistical Analysis
- Depending on the data distribution, continuous data were presented as either the median and standard deviation (SD) or the interquartile range (IQR), while categorical variables were represented in terms of frequencies and proportions (%). The Shapiro-Wilk normality test was employed to test for normal distribution [20]. To compare the demographic and clinical characteristics between fully vaccinated and unvaccinated patients, the chi-square test was used for categorical variables, while the Kruskal-Wallis test or Wilcoxon rank-sum tests were used for continuous variables [21].
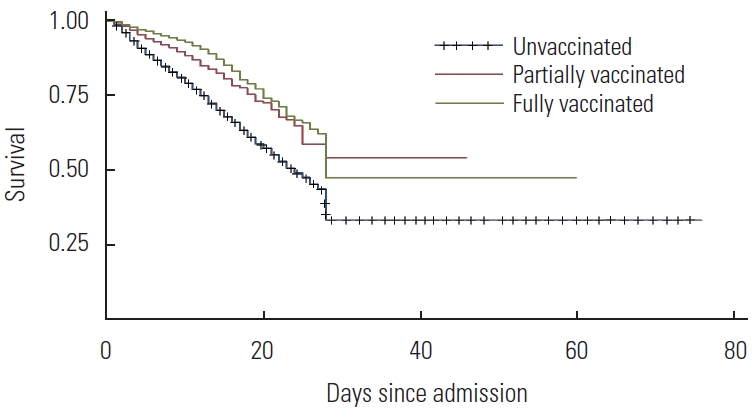
- We utilized the Cox-proportional hazard model to evaluate the relationship between vaccination status and in-hospital mortality [22]. First, the Cox-proportional hazard model was employed to individually assess the association of each covariate (age, sex, occupation, number of comorbidities, asthma, chronic kidney disease [CKD], chronic obstructive pulmonary disease [COPD], coronary artery disease [CAD], diabetes, hypertension, human immunodeficiency virus [HIV], heart failure, ICU treatment, and IMV) with in-hospital mortality. Subsequently, we examined the association between in-hospital mortality and vaccination status, adjusting for all the aforementioned covariates (age, sex, occupation, number of comorbidities, asthma, CKD, COPD, CAD, diabetes, hypertension, HIV, heart failure, ICU treatment, and IMV) [23]. A Kaplan-Meier failure function plot was created to illustrate the progression of in-hospital mortality among fully vaccinated, partially vaccinated, and unvaccinated hospitalized patients over a 5-week period following admission [24]. All study analyses were performed using Stata version 16 (StataCorp., College Station, TX, USA).
- Ethics Statement
- This study was approved by the Health Research Ethics Committee, National Institute of Health Research and Development, Ministry of Health, Indonesia (LB. 02.01/2/KE.103/2021) and performed in accordance with the principles of the Declaration of Helsinki. The informed consent was waived because of the retrospective nature of this study.
METHODS
- Patient Characteristics
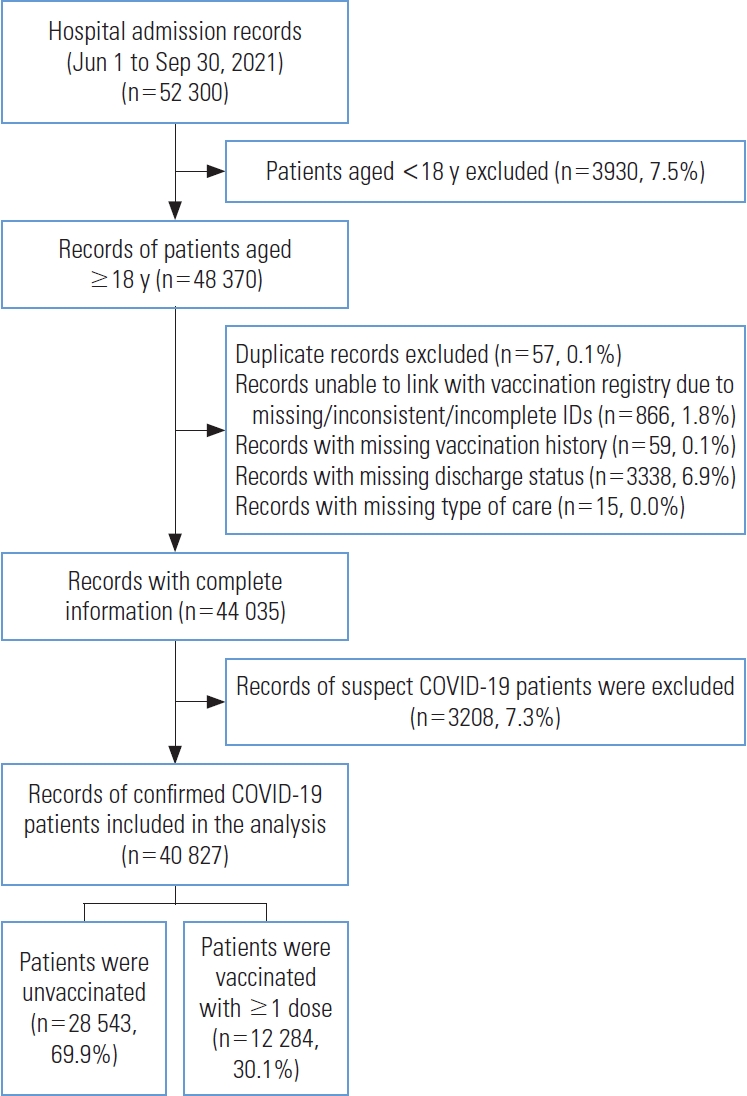
- The Pcare application recorded a total of 52 300 patients, but only 40 827 patients were included in the analysis. The primary reasons for analytical exclusion were predominantly missing information on discharge status (6.7%) and failure to link the vaccination registry with the Pcare application (1.8%) (Figure 1). The average age of the patients was 49 years (range, 35-59), with 53.2% being female and 94.6% not being healthcare workers (Table 1). While 61.6% of patients reported no comorbidities, 22.0% had hypertension, of which 14.2% were treated in the ICU. The median hospital stay for the group was 9 days, and 19.8% of patients died during their hospital treatment (Table 1).
- In-hospital mortality was more common in unvaccinated patients (23.5%) than in partially (12.6%) and fully vaccinated patients (8.3%). When considering vaccination status, the majority of hospitalized adults who were fully vaccinated belonged to the oldest age groups (>50 years; IQR 33-65) (Table 1). Only 10.1% of fully vaccinated patients had two or more comorbidities, with hypertension and diabetes being the most common. Within the fully vaccinated group, patients with hypertension were the most prevalent (25.2%) compared to other comorbidities, while the majority of patients with diabetes were unvaccinated (19.5%). Among unvaccinated patients, 16.7% were treated in the ICU and 4.4% required IMV, which was higher compared to fully vaccinated patients at 7.6% and 1.5%, respectively. The median length of hospital stay across all vaccination statuses was similar (9 days) (Table 1).
- In this study, during COVID-19 hospitalization, the majority of surviving patients (56.5%) were in the younger age group (18-49 years), while those who did not survive were predominantly aged over 60 years (44.9%) (data not shown). Among the survivors, there was a predominance of female patients (54.7%) without any comorbidities (65.6%). The proportion of patients with hypertension was similar between survivors (21.3%) and non-survivors (25.2%), but the percentage of patients with diabetes was lower among survivors (15.3%) compared to non-survivors (31.4%). Patients who were treated in the ICU and received IMV were more common among non-survivors (17.1%) than among survivors (0.4%) (Table 1).
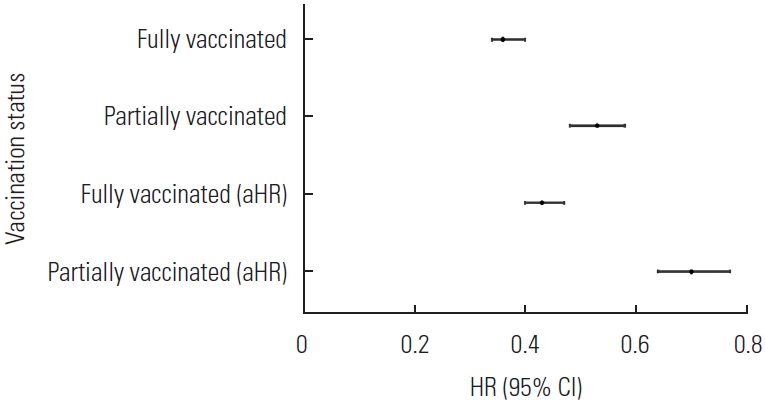
- Our study showed that patients who were either partially vaccinated (adjusted hazard ratio [aHR], 0.70; 95% confidence interval [CI], 0.64 to 0.77) or fully vaccinated (aHR, 0.43; 95% CI, 0.40 to 0.47) had a higher level of protection against in-hospital mortality than those who were unvaccinated (Figure 2). The overall incidence of in-hospital mortality was 0.021 per 1000 person-days. The mortality rate for the fully vaccinated group was lower (0.008 per 1000 person-days) than that of the unvaccinated group (0.024 per 1000 person-days). The mortality rate for the partially vaccinated patients was 0.013 per 1000 person-days. This rate was slightly higher than that of the fully vaccinated group, but it was still lower than the rate for the unvaccinated group (Figure 3). In-hospital mortality was found to be associated with all covariates (age, sex, occupation, and treatment received by the patients), with the exception of the number of comorbidities (Supplemental Materials 1 and 2).
RESULTS
Vaccination status and in-hospital mortality
- Our study investigated the association between vaccination status and in-hospital mortality among COVID-19 patients in Jakarta, Indonesia. Broadly speaking, our findings indicated that fully vaccinated adults experienced a significant reduction in in-hospital mortality compared to those who were only partially vaccinated or unvaccinated. As anticipated, our results align with previous studies conducted in similar contexts [10,25,26].
- Even before COVID-19 vaccine development, many posited that vaccination could play a crucial role in reducing both the mortality rate and severity of the disease [27]. As expected, our study is in agreement with previous studies [10,25,26]. The primary explanation for this likely stems from theoretical aspects. For instance, Sinovac-CoronaVac is an inactivated vaccine that stimulates the production of neutralizing antibodies (NAb) against SARS-CoV-2 [17]. Despite Sinovac-CoronaVac’s comparatively lower vaccine effectiveness, it mimics a natural infection in a milder form, yet it is potent enough to generate a sufficient and enduring immune response [6]. Furthermore, the presence of NAb in human cells prior to infection thwarts further viral invasion, thereby mitigating the effects of the infection, including its severity and associated mortality [28].
- Achieving adequate protection from a vaccination theoretically necessitates an appropriate number of vaccine doses. Evidence has demonstrated that a minimum of 2 doses of a vaccine is crucial to induce an immune response against the pathogen, whereas a single dose only results in partial immunity [29]. Furthermore, antibody levels elicited by COVID-19 vaccines may decrease over time, leading to the recommendation that individuals receive a subsequent dose of the vaccine [29]. Therefore, our immune system is better equipped to respond more rapidly and comprehensively to the same pathogen infection in the future.
- Regardless of the severity and mortality rates of diseases, vaccines play a crucial role in controlling the spread of pathogens within society [30]. For instance, the European Centre for Disease Prevention and Control has reported that a decrease in incidence over time is indicative of successful vaccine performance in reducing disease transmission [31]. Similarly, a study demonstrated that a vaccine could reduce an individual’s susceptibility to SARS-CoV-2 infection by 89.4%. Furthermore, the rate of community transmission and viral load kinetics among household contacts exposed to the Delta variant was lower in the fully vaccinated group than in the unvaccinated group during the secondary attack rate [32].
- Consistent with prior research, our study determined that various socio-demographic and clinical characteristics have an impact on in-hospital mortality [33]. This is likely due to the less effective control of SARS-CoV-2 by the immune systems of certain patient groups, specifically those of older age and male patients, as a result of depleted cellular immune function [34,35]. Furthermore, the initial global distribution of the COVID-19 vaccine was primarily focused on certain professions, such as healthcare workers, due to a shortage of vaccines. As a result, it is anticipated that professions not prioritized for vaccination may face a higher risk of COVID-19-related mortality [36].
- Although our study did not find a correlation between COPD, HIV, and in-hospital mortality, a systematic review and meta-analysis highlighted that certain significant comorbidities in adults, such as diabetes, hypertension, CKD, and immunosuppression, were linked to an elevated risk of severe illness from COVID-19 [37]. Our findings may be inconsistent with previous studies due to potential underreporting of patients’ comorbidity statuses, which could have led to a biased estimation of the risk association among various comorbidities in this study.
- Although there is evidence suggesting a diminished efficacy against Delta-associated infections compared to other variants, research indicates that the available COVID-19 vaccines still provide protection against severe outcomes [7,28,38]. In this study, we found that vaccinated individuals were less likely to experience critical outcomes. Consequently, vaccination proves beneficial in preventing more severe illnesses, resulting in a lower rate of hospitalization, ICU admission, and IMV necessity among fully or partially vaccinated adults compared to those who are unvaccinated.
- Strengths and Limitation
- Our study contributes to a better understanding of the vaccination status and in-hospital mortality among adults in Jakarta, Indonesia. This study, which utilized a large representative sample size and covered most hospitals in Jakarta, employed a superior study design approach. However, it also had several limitations. First, we did not have access to information on other clinical conditions of the patients, such as body mass index, oxygen saturation, and symptoms. As a result, the risk estimation for in-hospital mortality must be interpreted with caution. Second, the data may underreport comorbidities due to potential variations among hospitals in identifying underlying medical conditions. Third, several important factors, such as patients’ history of a previous infection, were unavailable within the Pcare application. Despite these limitations, our study is sufficiently robust to describe the association between vaccination status and in-hospital mortality within the described population composition.
- In conclusion, our findings indicate that vaccinated adults had a lower risk of in-hospital mortality compared to their unvaccinated counterparts. Additionally, our findings indicated that certain socio-demographic characteristics, specifically age and sex, were associated with in-hospital mortality. Consequently, healthcare professionals should consider these specific characteristics as a crucial component in the treatment of adults within this patient group.
DISCUSSION
DATA AVAILABILITY
SUPPLEMENTAL MATERIALS
Supplemental Material 1.
Supplemental Material 2.
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Hutapea HML, Dhewantara PW, Suryatma A. Data curation: Dhewantara PW, Suryatma A, Anasi R. Formal analysis: Hutapea HML, Dhewantara PW, Anasi R. Funding acquisition: None. Methodology: Hutapea HML, Dhewantara PW, Hendarwan H. Project administration: Dhewantara PW, Suryatma A. Visualization: Hutapea HML, Dhewantara PW, Sudaryo MK, Gayatri D. Writing – original draft: Hutapea HML, Dhewantara PW, Gayatri D. Writing – review & editing: Hutapea HML, Dhewantara PW, Suryatma A, Anasi R, Hendarwan H, Sudaryo MK, Gayatri D.
Notes
ACKNOWLEDGEMENTS
| Characteristics | Vaccination status |
In-hospital mortality |
|||
|---|---|---|---|---|---|
| No (n = 32 945) | Yes (n = 7882) | ||||
| Age (y) | Unvaccinated | 50.0±15.2 | 46.0±15.4 | 58.0±13.3 | |
| Partially vaccinated | 46.0±13.7 | ||||
| Fully vaccinated | 51.0±17.8 | ||||
| Overall | 49.0±15.7 | ||||
| Sex, female1 | Unvaccinated | 15 750 (55.2) | 18 023 (54.7) | 3695 (46.9) | |
| Partially vaccinated | 1790 (47.1) | ||||
| Fully vaccinated | 4178 (49.3) | ||||
| Total | 21 718 (53.2) | ||||
| Occupation1 | |||||
| Non-HCWs | Unvaccinated | 28 248 (99.0) | 30 737 (93.3) | 7865 (99.8) | |
| Partially vaccinated | 3708 (97.5) | ||||
| Fully vaccinated | 6646 (78.4) | ||||
| Total | 38 602 (94.6) | ||||
| HCWs | Unvaccinated | 295 (1.0) | 2208 (6.7) | 17 (0.2) | |
| Partially vaccinated | 94 (2.5) | ||||
| Fully vaccinated | 1836 (21.6) | ||||
| Total | 2225 (5.4) | ||||
| No. of comorbidities1 | |||||
| None | Unvaccinated | 17 356 (60.8) | 21 600 (65.6) | 3564 (45.2) | |
| Partially vaccinated | 2555 (67.2) | ||||
| Fully vaccinated | 5253 (61.9) | ||||
| Total | 25 164 (61.6) | ||||
| One | Unvaccinated | 8384 (29.4) | 8657 (26.3) | 3080 (39.1) | |
| Partially vaccinated | 980 (25.8) | ||||
| Fully vaccinated | 2373 (28.0) | ||||
| Total | 11 737 (28.8) | ||||
| Two or more | Unvaccinated | 2803 (9.8) | 2688 (8.2) | 1238 (15.7) | |
| Partially vaccinated | 267 (7.0) | ||||
| Fully vaccinated | 856 (10.1) | ||||
| Total | 3926 (9.6) | ||||
| Comorbidities1 | |||||
| Asthma | Unvaccinated | 295 (1.0) | 394 (1.2) | 49 (0.6) | |
| Partially vaccinated | 41 (1.1) | ||||
| Fully vaccinated | 107 (1.3) | ||||
| Total | 443 (1.1) | ||||
| CKD | Unvaccinated | 858 (3.0) | 446 (1.4) | 585 (7.4) | |
| Partially vaccinated | 48 (1.3) | ||||
| Fully vaccinated | 125 (1.5) | ||||
| Total | 1031 (2.5) | ||||
| COPD | Unvaccinated | 52 (0.2) | 57 (0.2) | 14 (0.2) | |
| Partially vaccinated | 1 (0.0) | ||||
| Fully vaccinated | 18 (0.2) | ||||
| Total | 71 (0.2) | ||||
| CAD | Unvaccinated | 958 (3.4) | 962 (2.9) | 404 (5.1) | |
| Partially vaccinated | 88 (2.3) | ||||
| Fully vaccinated | 320 (3.8) | ||||
| Total | 1366 (3.4) | ||||
| Diabetes | Unvaccinated | 5570 (19.5) | 5055 (15.3) | 2475 (31.4) | |
| Partially vaccinated | 561 (14.8) | ||||
| Fully vaccinated | 1399 (16.5) | ||||
| Total | 7530 (18.4) | ||||
| Hypertension | Unvaccinated | 6081 (19.5) | 6998 (21.3) | 1983 (25.2) | |
| Partially vaccinated | 760 (20.0) | ||||
| Fully vaccinated | 2140 (25.2) | ||||
| Total | 8981 (22.0) | ||||
| HIV | Unvaccinated | 86 (0.3) | 78 (0.2) | 28 (0.4) | |
| Partially vaccinated | 9 (0.2) | ||||
| Fully vaccinated | 11 (0.1) | ||||
| Total | 106 (0.3) | ||||
| Heart failure | Unvaccinated | 343 (1.2) | 253 (0.8) | 161 (2.0) | |
| Partially vaccinated | 22 (0.6) | ||||
| Fully vaccinated | 49 (0.6) | ||||
| Total | 414 (1.1) | ||||
| Hospitalization outcome | |||||
| ICU1 | Unvaccinated | 4768 (16.7) | 2075 (6.3) | 3727 (47.3) | |
| Partially vaccinated | 388 (10.2) | ||||
| Fully vaccinated | 646 (7.6) | ||||
| Total | 5802 (14.2) | ||||
| IMV1 | Unvaccinated | 1252 (4.4) | 114 (0.4) | 1348 (17.1) | |
| Partially vaccinated | 82 (2.2) | ||||
| Fully vaccinated | 128 (1.5) | ||||
| Total | 1462 (3.6) | ||||
| Length of stay (day) | Unvaccinated | 9.0±5.4 | 9.0±4.9 | 6.0±5.9 | |
| Partially vaccinated | 9.0±4.8 | ||||
| Fully vaccinated | 9.0±4.4 | ||||
| Overall | 9.0±5.2 | ||||
| In-hospital mortality1 | Unvaccinated | 6705 (23.5) | - | - | |
| Partially vaccinated | 477 (12.6) | ||||
| Fully vaccinated | 700 (8.3) | ||||
| Total | 7882 (19.3) | ||||
| Days since last vaccination dose | Unvaccinated | N/A | 97.0±36.7 | 84.0±25.2 | |
| Partially vaccinated | 95.0±36.1 | ||||
| Fully vaccinated | 95.0±36.1 | ||||
| Overall | 80.0±46.2 | ||||
Values are presented as median±standard deviation or number (%); Percentages presented for the vaccination status number refer to the number of each group; Percentages presented for demographic characteristics, comorbidities, and hospitalization outcomes are row percentages.
HCW, healthcare worker; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CAD, coronary artery disease; HIV, human immunodeficiency virus; ICU, intensive care unit; IMV, invasive mechanical ventilation; N/A, not available.
1 The number for unvaccinated group =28 543 patients, partially vaccinated group =3802 patients, and fully vaccinated group =8482 patients, and the total number of participants was 40 827.
- 1. World Health Organization. WHO coronavirus (COVID-19) dashboard [cited 2023 Mar 11]. Available from: https://covid19.who.int/
- 2. Ministry of Health of Indonesia. COVID-19 dashboard [cited 2023 Mar 15]. Available from: https://infeksiemerging.kemkes.go.id/dashboard/covid-19 (Indonesian)
- 3. Hakim MS, Wibawa H, Setiawaty V, et al. Is the infection of the SARS-CoV-2 Delta variant associated with the outcomes of COVID-19 patients? Front Med (Lausanne) 2021;8: 780611PubMedPMC
- 4. Haileamlak A. The impact of COVID-19 on health and health systems. Ethiop J Health Sci 2021;31(6):1073-1074PubMedPMC
- 5. Sparke M, Levy O. Competing responses to global inequalities in access to COVID vaccines: vaccine diplomacy and vaccine charity versus vaccine liberty. Clin Infect Dis 2022;75(Suppl 1):S86-S92ArticlePubMedPMCPDF
- 6. Choi EM. COVID-19 vaccines for low- and middle-income countries. Trans R Soc Trop Med Hyg 2021;115(5):447-456ArticlePubMedPMCPDF
- 7. Ma C, Sun W, Tang T, Jia M, Liu Y, Wan Y, et al. Effectiveness of adenovirus type 5 vectored and inactivated COVID-19 vaccines against symptomatic COVID-19, COVID-19 pneumonia, and severe COVID-19 caused by the B.1.617.2 (Delta) variant: evidence from an outbreak in Yunnan, China, 2021. Vaccine 2022;40(20):2869-2874ArticlePubMedPMC
- 8. Huespe IA, Ferraris A, Lalueza A, Valdez PR, Peroni ML, Cayetti LA, et al. COVID-19 vaccines reduce mortality in hospitalized patients with oxygen requirements: differences between vaccine subtypes. A multicontinental cohort study. J Med Virol 2023;95(5):e28786ArticlePubMed
- 9. Lee SW, Ma D, Davoodian A, Ayutyanont N, Werner B. COVID-19 vaccination decreased COVID-19 hospital length of stay, in-hospital death, and increased home discharge. Prev Med Rep 2023;32: 102152ArticlePubMedPMC
- 10. Muthukrishnan J, Vardhan V, Mangalesh S, Koley M, Shankar S, Yadav AK, et al. Vaccination status and COVID-19 related mortality: a hospital based cross sectional study. Med J Armed Forces India 2021;77: S278-S282ArticlePubMedPMC
- 11. Li M, Lou F, Fan H. SARS-CoV-2 variants of concern Delta: a great challenge to prevention and control of COVID-19. Sig Transduct Target Ther 2021;6: 349ArticlePubMedPMCPDF
- 12. Ministry of Health of the Republic of Indonesia; Ministry of Communication and Information Technology of the Republic of Indonesia. Joint Decree on one COVID-19 vaccination data. Jakarta: Ministry of Health of the Republic of Indonesia; 2021. p. 13 (indonesian)
- 13. Ministry of Health of the Republic of Indonesia. Latest news on coronavirus disease (COVID-19), 23 November 2021 [cited 2023 Mar 11]. Available from: https://infeksiemerging.kemkes.go.id/index.php/situasi-infeksi-emerging/situasi-terkini-perkembangan-coronavirus-disease-covid-19-23-november-2021 (Indonesian)
- 14. Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Netw Open 2020;3(12):e2029058ArticlePubMedPMC
- 15. Taylor CA, Whitaker M, Anglin O, Milucky J, Patel K, Pham H, et al. COVID-19-associated hospitalizations among adults during SARS-CoV-2 Delta and Omicron variant predominance, by race/ethnicity and vaccination status - COVID-NET, 14 states, July 2021-January 2022. MMWR Morb Mortal Wkly Rep 2022;71(12):466-473ArticlePubMedPMC
- 16. Liang XM, Xu QY, Jia ZJ, Wu MJ, Liu YY, Lin LR, et al. A third dose of an inactivated vaccine dramatically increased the levels and decay times of anti-SARS-CoV-2 antibodies, but disappointingly declined again: a prospective, longitudinal, cohort study at 18 serial time points over 368 days. Front Immunol 2022;13: 876037ArticlePubMedPMC
- 17. World Health Organization. The Sinovac-CoronaVac COVID-19 vaccine: what you need to know. 2022 Jun 10 [cited 2023 Mar 15]. Available from: https://www.who.int/news-room/featurestories/detail/the-sinovac-covid-19-vaccine-what-you-needto-know?gclid=Cj0KCQiAo7KqBhDhARIsAKhZ4uhvjYOWxJQUlunY-byP9F_TzCaBTsm9vzWb_NdLuC-IZidzPXoFK_caAmEFEALw_wcB
- 18. Social Health Insurance Administration Body. How to use Pcare [cited 2023 Mar 15]. Available from: https://indonesia.go.id/kategori/kesehatan/1139/cara-gunakan-pcare-bpjs-kesehatan?lang=1 (Indonesian)
- 19. Centers for Disease Control and Prevention. National center for health statistics International Classification of Diseases, (ICD-10-CM/PCS) transition - background. 2021 [cited 2023 Mar 15]. Available from: https://www.cdc.gov/nchs/icd/icd10.htm
- 20. Mishra P, Pandey CM, Singh U, Gupta A, Sahu C, Keshri A. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth 2019;22(1):67-72ArticlePubMedPMC
- 21. Lee SW. Regression analysis for continuous independent variables in medical research: statistical standard and guideline of Life Cycle Committee. Life Cycle 2022;2: e3ArticlePDF
- 22. Grant SW, Hickey GL, Head SJ. Statistical primer: multivariable regression considerations and pitfalls. Eur J Cardiothorac Surg 2019;55(2):179-185ArticlePubMed
- 23. Gopalan N, Senthil S, Prabakar NL, Senguttuvan T, Bhaskar A, Jagannathan M, et al. Predictors of mortality among hospitalized COVID-19 patients and risk score formulation for prioritizing tertiary care-an experience from South India. PLoS One 2022;17(2):e0263471ArticlePubMedPMC
- 24. Calabuig JM, García-Raffi LM, García-Valiente A, Sánchez-Pérez EA. Kaplan-Meier type survival curves for COVID-19: a health data based decision-making tool. Front Public Health 2021;9: 646863ArticlePubMedPMC
- 25. Rahman MS, Harun MG, Sumon SA, Mohona TM, Abdullah SA, Khan MN, et al. Hospitalization and mortality by vaccination status among COVID-19 patients aged ≥25 years in Bangladesh: results from a multicenter cross-sectional study. Vaccines (Basel) 2022;10(12):1987ArticlePubMedPMC
- 26. Grapsa E, Adamos G, Andrianopoulos I, Tsolaki V, Giannakoulis VG, Karavidas N, et al. Association between vaccination status and mortality among intubated patients with COVID-19-related acute respiratory distress syndrome. JAMA Netw Open 2022;5(10):e2235219ArticlePubMedPMC
- 27. Derrough T, Olsson K, Gianfredi V, Simondon F, Heijbel H, Danielsson N, et al. Immunisation Information Systems - useful tools for monitoring vaccination programmes in EU/EEA countries, 2016. Euro Surveill 2017;22(17):30519ArticlePubMedPMC
- 28. Huang YZ, Kuan CC. Vaccination to reduce severe COVID-19 and mortality in COVID-19 patients: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci 2022;26(5):1770-1776PubMed
- 29. Shekhar R, Garg I, Pal S, Kottewar S, Sheikh AB. COVID-19 vaccine booster: to boost or not to boost. Infect Dis Rep 2021;13(4):924-929ArticlePubMedPMC
- 30. Suthar AB, Wang J, Seffren V, Wiegand RE, Griffing S, Zell E. Public health impact of covid-19 vaccines in the US: observational study. BMJ 2022;377: e069317ArticlePubMedPMC
- 31. European Centre for Disease Prevention and Control. Risk of SARS-CoV-2 transmission from newly-infected individuals with documented previous infection or vaccination. 2021 2021 Mar 29 [cited 2023 Aug 1]. Available from: https://www.ecdc.europa.eu/en/publications-data/sars-cov-2-transmission-newly-infected-individuals-previous-infection#no-link
- 32. Prunas O, Warren JL, Crawford FW, Gazit S, Patalon T, Weinberger DM, et al. Vaccination with BNT162b2 reduces transmission of SARS-CoV-2 to household contacts in Israel. Science 2022;375(6585):1151-1154ArticlePubMedPMC
- 33. Sheikh A, McMenamin J, Taylor B, Robertson C; Public Health Scotland and the EAVE II Collaborators. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021;397(10293):2461-2462ArticlePubMedPMC
- 34. Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ 2020;11(1):29ArticlePubMedPMCPDF
- 35. Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 2020;11(1):6317ArticlePubMedPMCPDF
- 36. Thorsteinsdottir B, Madsen BE. Prioritizing health care workers and first responders for access to the COVID19 vaccine is not unethical, but both fair and effective - an ethical analysis. Scand J Trauma Resusc Emerg Med 2021;29(1):77ArticlePubMedPMCPDF
- 37. Thakur B, Dubey P, Benitez J, Torres JP, Reddy S, Shokar N, et al. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Rep 2021;11(1):8562ArticlePubMedPMCPDF
- 38. Pormohammad A, Zarei M, Ghorbani S, Mohammadi M, Aghayari Sheikh Neshin S, Khatami A, et al. Effectiveness of COVID-19 vaccines against Delta (B.1.617.2) variant: a systematic review and meta-analysis of clinical studies. Vaccines (Basel) 2021;10(1):23ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite




