Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 53(4); 2020 > Article
-
Perspective
Yemen’s Cholera Epidemic Is a One Health Issue -
Qin Xiang Ng1
 , Michelle Lee Zhi Qing De Deyn2
, Michelle Lee Zhi Qing De Deyn2 , Wayren Loke1
, Wayren Loke1 , Wee Song Yeo3
, Wee Song Yeo3
-
Journal of Preventive Medicine and Public Health 2020;53(4):289-292.
DOI: https://doi.org/10.3961/jpmph.20.154
Published online: June 10, 2020
1Ministry of Health Holdings Pte Ltd., Singapore
2Department of Medicine, James Cook University Hospital, Middlesbrough, United Kingdom
3Mount Elizabeth Hospital, Singapore
- Corresponding author: Qin Xiang Ng, MBBS, MPH Ministry of Health Holdings Pte Ltd., 1 Maritime Square, Singapore 099253, Singapore E-mail: ng.qin.xiang@u.nus.edu
Copyright © 2020 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
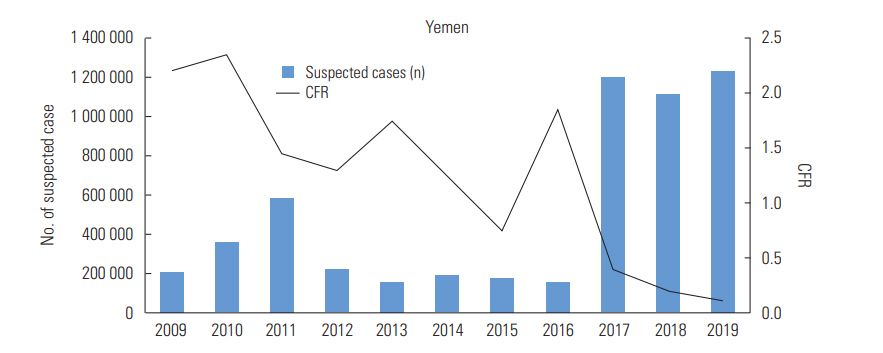
- Yemen has been faced with the worst cholera epidemic of modern times, with more than 1 million suspected cases and 3000 deaths at the time of writing. This problem is largely due to the longstanding civil war between pro-government forces and the Houthi armed movement, which has severely damaged already vulnerable sanitation and healthcare facilities and systems in the country. It is further compounded by a dire lack of basic amenities, chronic malnutrition, and unfavourable weather conditions. Another contributory component may be aerial transfer by cholera-infected chironomid insects. To contain the spread of cholera in Yemen, a nation-wide armistice should be negotiated, and national and local committees must be convened to coordinate efforts on the ground. Community isolation facilities with proper sanitation, reliable disposal systems, and a clean water supply should be set up to isolate and treat sick patients. The continuity of vaccination programmes should be ensured. Public health campaigns to educate local communities about good hygiene practices and nutrition are also necessary. The One Health paradigm emphasizes a multi-sectoral and transdisciplinary understanding and approach to prevent and mitigate the threat of communicable diseases. This paradigm is highly applicable to the ongoing cholera crisis in Yemen, as it demands a holistic and whole-of-society approach at the local, regional, and national levels. The key stakeholders and warring parties in Yemen must work towards a lasting ceasefire during these trying times, especially given the extra burden from the mounting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak worldwide.
- This paper is a perspective, so it did not need ethical approval.
Ethics Statement
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
None.
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Conceptualization: QXN. Data curation: QXN, MLZQDD, WL, WSY. Formal analysis: QXN, MLZQDD, WL, WSY. Funding acquisition: None. Project administration: QXN, WSY. Writing – original draft: QXN. Writing – review & editing: QXN, MLZQDD, WL, WSY.
Notes
- 1. World Health Organization. Yemen. 2020 [cited 2020 Apr 20]. Available from: https://www.who.int/emergencies/crises/yem/en/Article
- 2. Haidera M, Alhakimi SA, Noaman A, Al Kebsi A, Noaman A, Fencl A, et al. Water scarcity and climate change adaptation for Yemen’s vulnerable communities. Local Environ 2011;16(5):473-488Article
- 3. Merrell DS, Butler SM, Qadri F, Dolganov NA, Alam A, Cohen MB, et al. Host-induced epidemic spread of the cholera bacterium. Nature 2002;417(6889):642-645ArticlePubMedPMCPDF
- 4. Federspiel F, Ali M. The cholera outbreak in Yemen: lessons learned and way forward. BMC Public Health 2018;18(1):1338ArticlePubMedPMCPDF
- 5. Paz S. The cholera epidemic in Yemen - how did it start? The role of El Niño conditions followed by regional winds. Environ Res 2019;176: 108571ArticlePubMed
- 6. Almagro-Moreno S, Taylor RK. Cholera: environmental reservoirs and impact on disease transmission. Microbiol Spectr 2013;1(2):OH-0003-2012Article
- 7. Faruque SM, Naser IB, Islam MJ, Faruque AS, Ghosh AN, Nair GB, et al. Seasonal epidemics of cholera inversely correlate with the prevalence of environmental cholera phages. Proc Natl Acad Sci U S A 2005;102(5):1702-1707ArticlePubMedPMC
- 8. Gebreyes WA, Dupouy-Camet J, Newport MJ, Oliveira CJ, Schlesinger LS, Saif YM, et al. The global one health paradigm: challenges and opportunities for tackling infectious diseases at the human, animal, and environment interface in low-resource settings. PLoS Negl Trop Dis 2014;8(11):e3257ArticlePubMedPMC
- 9. Médecins Sans Frontières. Saving lives without salaries: government health staff in Yemen. [cited 2020 May 1]. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/msf-yemen-salaries-lr-def.pdf
- 10. Qadri F, Ali M, Lynch J, Chowdhury F, Khan AI, Wierzba TF, et al. Efficacy of a single-dose regimen of inactivated whole-cell oral cholera vaccine: results from 2 years of follow-up of a randomised trial. Lancet Infect Dis 2018;18(6):666-674ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Emerging zoonotic diseases in Southeast Asia in the period 2011–2022: a systematic literature review
Thanh Trung Nguyen, Thi Ngan Mai, Sinh Dang-Xuan, Hung Nguyen-Viet, Fred Unger, Hu Suk Lee
Veterinary Quarterly.2024; 44(1): 1. CrossRef - One Health in practice: Benefits and challenges of multisectoral coordination and collaboration in managing public health risks: A meta-analysis
Valentina Thobias Sanga, Esron D. Karimuribo, Abubakar S. Hoza
International Journal of One Health.2024; : 26. CrossRef - Transition of biological wastewater treatment from flocculent activated sludge to granular sludge systems towards circular economy
Philip Semaha, Zhongfang Lei, Tian Yuan, Zhenya Zhang, Kazuya Shimizu
Bioresource Technology Reports.2023; 21: 101294. CrossRef - Progress toward alleviating preventable waterborne diseases over the past 30 years
Tim Ford, Steve Hamner
Cambridge Prisms: Water.2023;[Epub] CrossRef - Early Determination of Case Fatality Rate of Covid-19 Pandemic During the Ongoing Yemeni Armed Conflict
Abdulla Salem Bin Ghouth, Ali Ahmed Al-Waleedi, Marhami Fahriani, Firzan Nainu, Harapan Harapan
Disaster Medicine and Public Health Preparedness.2022; 16(5): 1827. CrossRef - Food security and emerging infectious disease: risk assessment and risk management
Valeria Trivellone, Eric P. Hoberg, Walter A. Boeger, Daniel R. Brooks
Royal Society Open Science.2022;[Epub] CrossRef - Simulation-Based Assessment of Cholera Epidemic Response: A Case Study of Al-Hudaydah, Yemen
Pei Shan Loo, Anaely Aguiar, Birgit Kopainsky
Systems.2022; 11(1): 3. CrossRef - COVID-19 Pandemic in the Midst of Civil War: Planetary Health and Plant Omics Field Notes from Aden, Yemen
Abdulsamad Taresh Abdullah, Jawdat Hassen, Areeg Abdulsamad Abdullah, Mehmet Ağırbaşlı
OMICS: A Journal of Integrative Biology.2020; 24(12): 685. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


